Breast cancer is the most common cancer among women in Singapore. Data from the Singapore Cancer Registry under the Ministry of Health (MOH) shows that over 2,000 women in Singapore are diagnosed with breast cancer each year.
For many women, the decision to undergo breast screening can bring both relief and anxiety. Studies show that breast cancer has a 5-year survival rate exceeding 90% when detected at the localised stage before spreading to nearby tissues. This makes regular breast cancer screening an essential part of women's preventive healthcare.
The recommended method to detect early signs of breast cancer is to go for a mammogram. A supplementary breast ultrasound may also be ordered by your doctor. In this article, we will explain what you need to know about breast cancer screening.
When to consider clinical breast screening?
Women may consider professional breast screening in situations such as:
Routine screening based on age or risk profile
Dense breast tissue requiring additional imaging
Family history of breast cancer or related conditions
Previous abnormal screening results needing follow-up
New symptoms such as lumps, pain, or nipple discharge
Professional evaluation combines screening results with individual medical history and risk factors to provide a thorough assessment of breast health.
Types of Breast Screening
There are 2 common types of clinical breast examination that you can choose from, on top of monthly breast self-examinations:
- Mammogram
- Breast ultrasound
Mammogram
A mammogram screening is an x-ray of the breasts and is the most reliable screening tool for early breast cancer and other breast diseases.
Screening refers to a process to check for early disease when there are no signs or symptoms yet. A mammogram can detect tiny lumps or calcium spots in the breasts, which may be a sign of early breast cancer, or caused by non-cancerous reasons.
During the x-ray, a female radiographer will place your breast between two flat plastic plates and compress it for a few seconds. This is performed on one breast at a time. Patients may experience some discomfort when the breast tissue is compressed for a clearer image. Additional angles and views may also be taken for closer examination.
The patient will be exposed to a low dose of radiation during the procedure (equivalent to exposure to environmental background radiation for two months), so the overall radiation risk is low. As such, the potential benefits outweigh the risks.
If there is an abnormal mammogram result, your doctor may recommend further tests in your medical report. It is important to note that age and breast density can affect the accuracy of the mammogram screening test, which are also possible reasons for additional tests. For example, younger women tend to have denser breast tissue, which could mean that abnormalities will not appear during the mammogram and is ineffective in detecting cancer.
For women with dense breasts or those at higher risk of breast cancer, your doctor may recommend a Contrast Enhanced Mammography (CEM). This imaging technique combines standard mammography with contrast dye to provide clearer images and improve cancer detection, particularly in dense breast tissue.
Breast Ultrasound
An ultrasound of the breasts is safe, non-invasive, and painless, and is the same technology used to monitor a baby during pregnancy. The procedure helps to detect lumps and determines if a lump is solid or cystic.
However, an ultrasound cannot detect calcium spots. Therefore, your doctor may order an ultrasound-guided biopsy to confirm what type of lump it is. An ultrasound may also supplement a mammogram for ladies with dense breasts.
If you have breast implants or a family history of breast cancer, talk to your doctor to ask about MRI screening. For patients where breast cancer screening picks up an abnormality, consult your doctor, and they will advise if you need a biopsy.
HPB Screen For Life Breast Cancer Screening
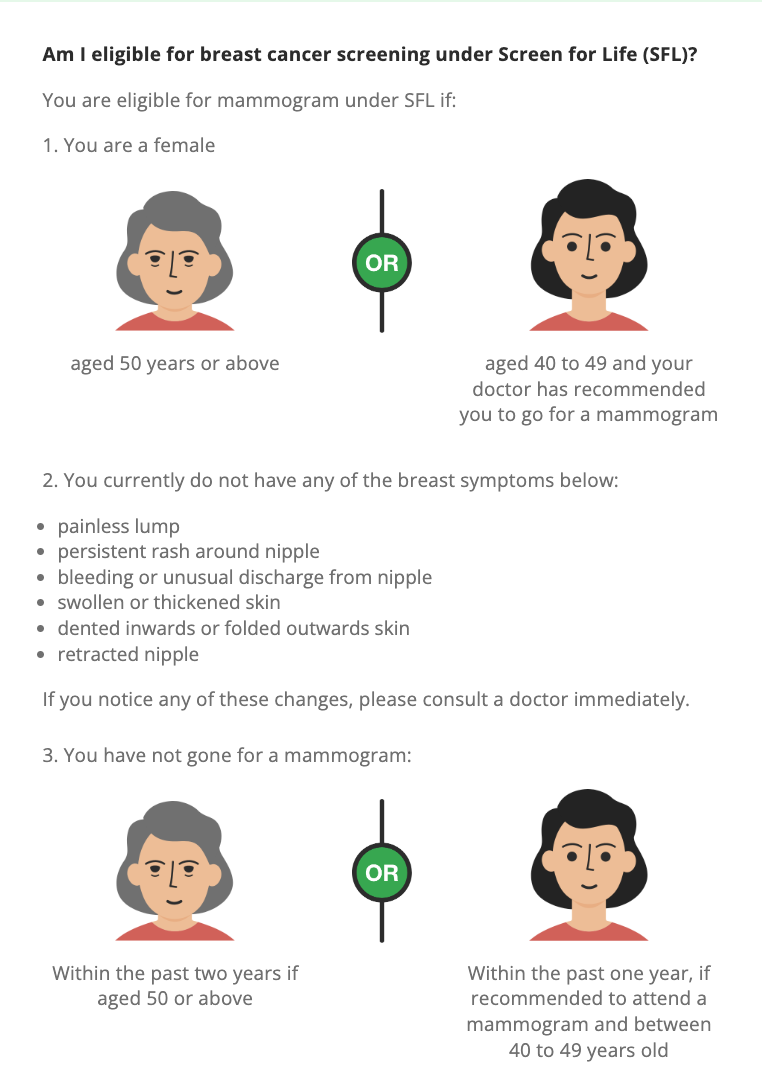
The Screen For Life Breast Cancer Screening programme by the Singapore Health Promotion Board (HPB) offers subsidised mammogram screenings for women aged 50 and above, or women between the ages of 40 to 49, who decided to make a mammogram appointment after consulting their doctor.
You may get a subsidised mammogram screening test at participating Breast Screening Centres verified by the Health Promotion Board and the Singapore Cancer Society.
To be eligible for the screening, you must not have the following breast symptoms:
- painless lump
- persistent rash around nipple
- bleeding or unusual discharge from nipple
- swollen or thickened skin
- dented inwards or folded outwards skin
- retracted nipple
For women over 50, you haven't gone for a mammogram within the past two years. For women aged 40 and 49, you haven't gone for a mammogram within the past year.
Breast screening packages at Thomson Breast Centre
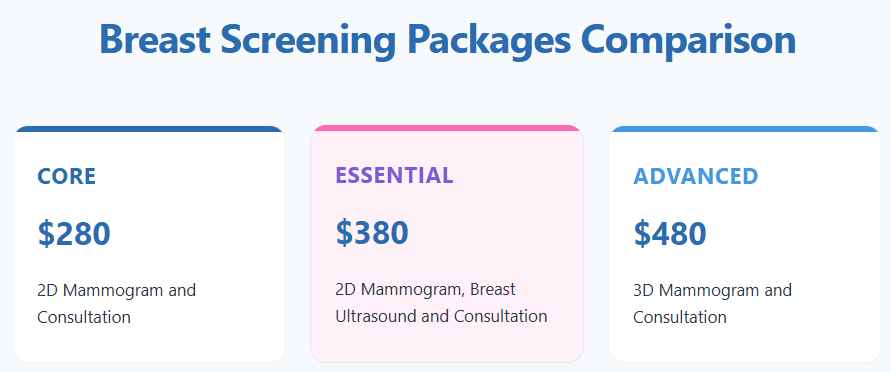
Package | What’s Included | Suitable For |
Core – $280 | • 2D Digital Mammogram • Consultation with specialist | Women going for routine or first-time breast screening |
Essential – $380 | • 2D Digital Mammogram • Breast Ultrasound • Consultation with specialist | Women with dense breast tissue or those seeking a more comprehensive check |
Advanced – $480 | • 3D Mammography (Tomosynthesis) • Consultation with specialist | Women with dense breasts or a family history of breast conditions |
Each package includes a specialist consultation to review results and discuss any follow-up if required. Your healthcare provider can help determine the most suitable package based on your age, breast density, family history, and individual risk factors.
Breast screening at Thomson Breast Centre
Breast screening is available at Thomson Breast Centre, a dedicated facility within Thomson Medical Centre focusing on the diagnosis and care of breast health.
With over 45 years of experience in women's healthcare, Thomson's clinical team provides breast screening services with individualised care. Here you will get:
Specialist consultation included with every screening package
2D mammography, 3D mammography (tomosynthesis), and breast ultrasound available
Imaging services suitable for various breast tissue types, including dense tissue
Coordination with Thomson's network of specialists and imaging services when follow-up care is required
FAQ
At what age should you get a cancer screening?
Women aged 40 to 49 are recommended to go for a mammogram every year due to the higher breast cancer risk. However, for women aged 50 and above, screenings can be reduced to once every two years.
For younger women below the age of 40, a screening mammogram is not recommended. However, if you have a high risk of breast cancer due to family history or hereditary genetic mutations, you should speak to a breast specialist early, and they will recommend when you should start breast cancer screening.
In addition to screening, all women aged 18 and above should do monthly breast self-examinations (BSE). This examination helps you be familiarised with the look and feel of your breasts. As a result, you can detect any changes and abnormalities in your breast tissues more efficiently and increase the chances of early detection.
If you notice a change in your breasts that seems abnormal or if one breast is different from the other while doing a BSE, you should seek immediate medical advice from your doctor.
Is a mammogram painful?
The whole mammogram procedure is not necessarily painful but you may experience discomfort due to the compression of the breasts between two plates. If it gets too uncomfortable, please do not hesitate to inform your radiographer.
What are the major risk factors for developing breast cancer?
Some women are at higher risk of developing breast cancer. Here are some of the risk factors:
- Having one or more close relatives with breast cancer
- Personal history of breast cancer
- Age: breast cancer risk increases as one gets older, especially after menopause
- Being overweight
- Being physically inactive
- Drinking alcohol regularly
- History of ovarian cancer
- Early-onset of menstruation, or
- Long-term use of combined hormone replacement therapy (of more than five years)
Regular mammograms are essential, even more so for women with these risk factors. Note that not having any risk factors does not mean you will not develop breast cancer. It simply means your breast cancer risk is lower than others. Therefore, it is recommended that you go for a mammogram screening in Singapore even if you do not detect any abnormalities in your breast tissue.
What happens after the diagnosis of breast cancer?
Once your doctor confirms a breast cancer diagnosis, the first process involved is staging. This will help determine the extent of the disease and prognosis. It is also used to plan treatment options.
Breast cancer is typically classified into Stage 0, I, II, III, or IV. These stages are based on the tumour size, the involvement of lymph nodes, and whether it has spread to other body parts.
The presence of tumour markers like estrogen progesterone receptors and proliferation factors (HER2) are also analysed during the staging process, as they may affect the sequence of treatment for surgery versus systemic therapy.
What are the most common treatments for breast cancer?
Once staging is done, your doctor will advise on the ideal treatment options. The course of treatment will highly depend on your overall health, breast cancer type, stage, grade, size, sensitivity to hormones, and your personal preference. The most common treatment options are surgery (lumpectomy or mastectomy), chemotherapy, radiation therapy, and hormonal therapy.