Trying to conceive can be both exciting and overwhelming. For many couples, assisted reproductive technology (ART) such as IVF provides new hope. But success doesn’t just depend on fertilisation. It depends on how well the embryo develops in the early days after.
One of the most important milestones in this journey is the blastocyst stage. This stage decides whether a fertilised egg will continue growing and eventually become a healthy pregnancy.
Knowing how blastocysts form, develop, and implant can help you make informed decisions during your IVF treatment. It also gives you insight into the earliest steps of how life begins.
What is a blastocyst?
A blastocyst is an early-stage embryo that develops about five to six days after fertilisation. It marks a key point in early embryonic development when the fertilised egg (zygote) has divided many times to form a hollow ball of over 200 cells.
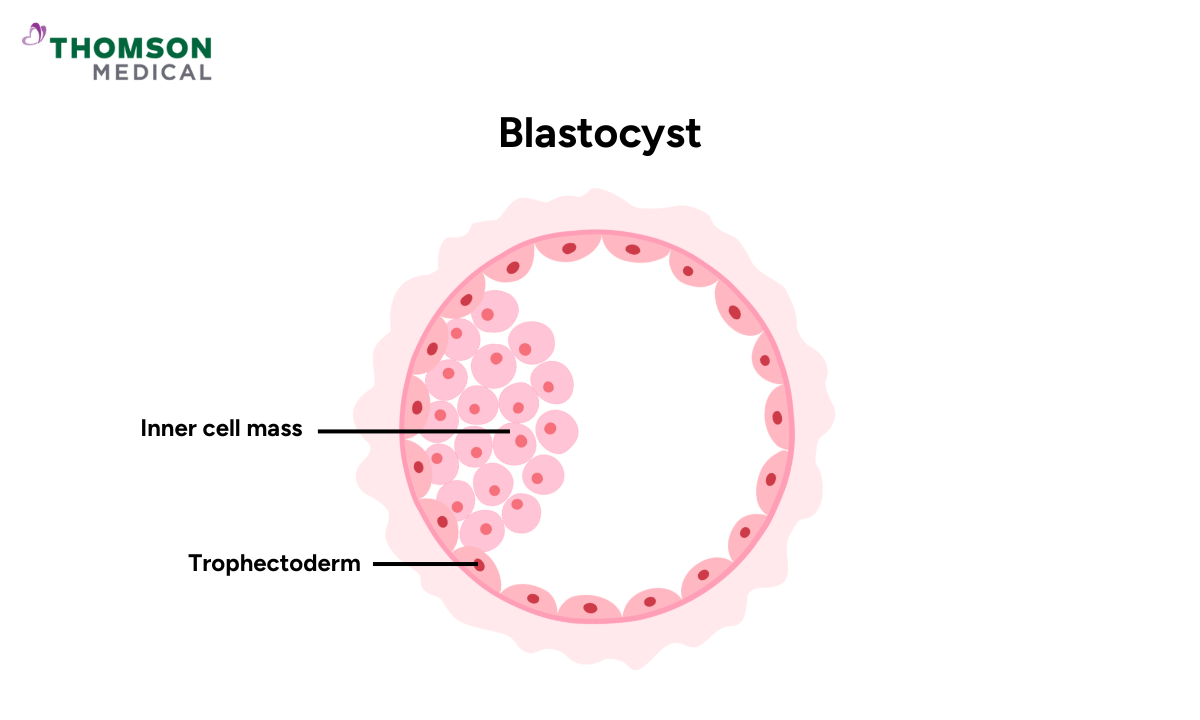
This ball has two main parts:
Inner cell mass (ICM), which develops into the baby
Trophectoderm (outer layer), which forms the placenta and surrounding tissues
The blastocyst stage marks a significant shift. Your embryo has gone from a simple cluster of cells to a more complex structure that's ready to implant in your uterine lining.
Where does blastocyst implantation occur?
In a normal pregnancy, the blastocyst implants in the lining of the uterus (endometrium), most commonly along the upper part of the uterine wall. This is where the embryo will grow and develop throughout pregnancy.Sometimes, a blastocyst doesn’t make it to the womb. Instead, it implants outside the womb (usually in a fallopian tube), which leads to an ectopic pregnancy and requires immediate medical attention.
What is the purpose of the blastocyst?
The primary function of the blastocyst is implantation. Before this can happen, the blastocyst must first "hatch" from its protective outer shell called the zona pellucida. Once the blastocyst breaks free from this shell, usually around day six or seven, it can attach itself to the lining of your uterus (called the endometrium).
Once implantation occurs, the embryo can:
Begin forming the placenta
Access oxygen and nutrients
Continue developing into a healthy pregnancy
Without successful implantation, pregnancy cannot continue. This makes the blastocyst stage a vital checkpoint in reproduction. Not all embryos reach the blastocyst stage – this natural selection process helps ensure that only the most developmentally capable embryos progress to pregnancy.
In IVF (In Vitro Fertilisation), doctors and embryologists assess the embryo’s growth and quality to determine which blastocyst has the best chance of implanting successfully.
Our fertility specialists
Loading...
What are the signs of blastocyst implantation?
Implantation can trigger subtle body changes, sometimes mistaken for early period symptoms. Common signs may include:
Light spotting or minor bleeding (implantation bleeding)
Cramping similar to menstrual cramps
Slight change in basal body temperature
Tiredness or mood changes due to hormonal shifts
Keep in mind that many people experience no noticeable signs. Implantation can happen silently, and that's completely normal.
Factors that affect blastocyst development
Whether a blastocyst grows and survives depends on several important factors, both in the lab and within your body. Understanding these helps explain why not every embryo develops the same way.
Laboratory Conditions
Embryos grow in a carefully controlled environment during IVF:
The culture media (nutrient-rich solution) to meet the embryo's need
Temperature and pH must stay constant to prevent stress
Clean air and sterile tools reduce contamination risks
Low light and low oxygen levels protect embryo DNA
All these factors support healthy blastocyst formation.
Egg and sperm quality
Egg quality has the biggest impact on development. As women age, egg quality naturally declines. Your overall reproductive health also plays a role.
Sperm quality matters too. Both the egg and sperm must have healthy DNA for the embryo to grow normally and reach the blastocyst stage.
Natural selection of embryos
Some embryos stop developing on their own. This happens when they have genetic issues or lack of energy to continue dividing. It's nature's way of selecting only the healthiest embryos to move forward. While it can feel discouraging, this process is completely natural.
Preimplantation Genetic Testing (PGT-A)
PGT-A checks whether an embryo has the right number of chromosomes. It can be helpful if you’ve had:
Repeated pregnancy loss
Failed implantation
Advanced maternal age (over 40)
PGT-A doesn’t guarantee pregnancy or a live birth. But it helps identify embryos with the best potential to succeed.
An embryologist’s skill also plays an important role. They assess each embryo under the microscope to find the ones most likely to develop into a healthy pregnancy.
If you’re undergoing IVF or planning for it, knowing what affects blastocyst development can help you make informed choices. Request an appointment with Thomson Medical to consult our fertility specialists, learn how these factors may apply to your situation, and explore ways to improve your embryo development outcomes.
Why is the blastocyst so important for IVF?
IVF, embryos are grown in the laboratory for several days. Allowing them to reach the blastocyst stage gives fertility specialists a better view of which embryos are developing normally. A healthy, expanding blastocyst has a higher chance of implanting successfully in your uterus. This can increase the likelihood of achieving pregnancy.
Benefits of growing blastocyst
Through blastocyst culture (the process of allowing embryos to develop to day five or six before transfer) specialists gain a clearer understanding of each embryo’s strength and potential for implantation. The main benefits include:
Follows the natural timing of conception, as embryos normally reach the uterus around this stage
Improve success rates by increasing the chances of implantation and pregnancy
Helps reduce multiple births by allowing specialists to select a single strong embryo for transfer
However, not every fertilised egg reaches this stage. If you start with only a few fertilised eggs, it's possible that none may develop into blastocysts. This can feel discouraging.
In cases like these, your doctor may recommend an earlier embryo transfer (typically on day three). This still offers a reasonable chance of pregnancy.
What are the risks and limitations of blastocysts?
Despite its benefits, blastocyst culture isn’t suitable for everyone. Some embryos don’t survive to day five, especially when you start with only a few fertilised eggs. In such cases, your doctor may recommend an earlier transfer on day three instead.
Although transferring at the blastocyst stage often improves success rates, there’s still a chance that no embryos will reach it. This can be emotionally challenging and difficult to process.
But this doesn't mean your IVF has failed. It simply reflects the natural biological variation in how embryos develop. Your fertility team will work with you to adjust your treatment plan based on your individual circumstances.
If you’re considering blastocyst transfer, it’s important to understand both its benefits and limitations. Request an appointment with Thomson Medical to speak with our fertility specialists, who can assess your situation and recommend the most suitable approach for your IVF journey.
FAQ
What is a blastocyst?
The blastocyst is a stage of embryo development, appearing around day five after fertilisation. It includes both the inner cell mass (which forms the baby) and the outer layer (which forms the placenta).
Is a blastocyst good for IVF?
Yes. Reaching this stage shows the embryo is strong and developing normally. Blastocyst transfer in IVF is linked with higher implantation and pregnancy rates.
How many eggs reach the blastocyst stage in IVF?
Not all fertilised eggs make it to this stage. On average, about 30–50% develop into blastocysts, depending on egg and sperm quality, as well as lab conditions.
Can a blastocyst split into twins?
Yes. If the inner cell mass divides early in development, it can lead to monozygotic twins (identical twins).
Which comes first, embryo or blastocyst?
The embryo forms first. The blastocyst is a later stage in that embryo’s growth, occurring after several rounds of cell division.
What is the baby called after a blastocyst?
After implantation, the blastocyst becomes an embryo until around eight weeks of pregnancy. From that point, it is called a foetus.
Can everyone have a blastocyst transfer?
Blastocyst transfer isn’t suitable for everyone. It’s mainly a laboratory process used to identify which embryos have the best potential. For patients with only one or two embryos, there’s little benefit in keeping them in the lab longer, as those embryos have already shown they’re suitable for transfer.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
