Sometimes, couples who once thought their family was complete may find themselves wanting a child.
If you or your partner has had a vasectomy, you might be wondering if it’s still possible to get pregnant – and whether intrauterine insemination (IUI) could help. This article will explain how IUI works after a vasectomy, what other options are available, and what to expect if you’re planning to grow your family again.
What is a vasectomy?
A vasectomy is a permanent birth control option for men who are sure they don't want to have children in the future. During this minor surgical procedure, your doctor will cut or block the vas deferens – these are the small tubes that carry sperm from your testicles to mix with your semen.
Vasectomy is a low-risk surgery, during which the operation can be done with local anaesthesia. The operation can be performed on an outpatient basis, which means you can return home the same day after the procedure.
Is it possible to reverse the procedure?
Yes, vasectomy reversal is possible, though it's important to know that it's a more complex surgery than the original vasectomy. There are actually two different approaches your surgeon might take, depending on your specific situation.
Vasovasostomy
Vasovasostomy is a type of procedure to reverse vasectomy by reconnecting the vas deferens, the thin tubes that carry the sperm from the testicles. It is a simple procedure, and the success rate of reverse sterilisation is high.
Vasoepididymostomy
Vasoepididymostomy is a type of complex procedure to reverse vasectomy by reconnecting the vas deferens to the epididymis, bypassing the blockage caused by vasectomy or other obstruction. It is a more complex procedure than vasovasostomy and requires specialised microsurgical skills. The success rate can be high when performed by experienced surgeons.
How does vasectomy affect fertility?
A vasectomy prevents pregnancy by blocking sperm from entering the semen. Even though the testicles continue to produce sperm, the procedure stops it from travelling through the vas deferens. Instead, the body naturally reabsorbs the unused sperm.
While vasectomy is a highly effective method of contraception, it’s not immediately effective. It usually takes about 2 to 3 months, or roughly 15 to 20 ejaculations, to completely clear any remaining sperm from the reproductive tract. During this time, it’s important to use another form of birth control until your doctor confirms that your semen is sperm-free.
.png?branch=production)
Can you do IUI after a vasectomy?
Yes, IUI is possible after a vasectomy, but it usually involves an additional step to retrieve sperm. Since sperm is no longer present in the semen after a vasectomy, it must be collected through other methods.
The collection can be done by reversing the vasectomy or using sperm retrieval techniques. Once sperm is obtained, it can be used for IUI or other fertility treatments like IVF.
For more information about your fertility options after a vasectomy or to receive advice tailored to your unique situation, consider speaking with a fertility specialist. You may contact Thomson Medical to arrange a consultation for personalised guidance on treatment options and the next step in your journey.
IUI specialists
Loading...
How is the sperm retrieved?
If you’ve had a vasectomy and want to conceive, sperm can be retrieved directly from the reproductive tract through minor surgical procedures. Two common methods are as follows:
Sperm aspiration (PESA, MESA)
PESA
Percutaneous Epididymal Sperm Aspiration (PESA) is a procedure where sperm is collected from the epididymis (a small coiled tube near the testicle where sperm is stored).
It’s typically used when there’s a blockage in the reproductive tract (obstructive azoospermia).
The procedure is done under local anaesthesia. A fine needle is gently inserted into the epididymis, and fluid is drawn out using a syringe.
This fluid is examined under a microscope to check for sperm. If sperm are found, they can be used fresh or frozen for future use in treatments like In-Vitro Fertilisation (IVF) with ICSI (Intracytoplasmic Sperm Injection).
If PESA doesn’t yield sperm, other methods like TESE may be needed.
MESA
Microsurgical Epididymal Sperm Aspiration (MESA) is another method where sperm are retrieved from the epididymis.
This procedure is performed using an operating microscope, often under general anaesthesia.
A small incision is made in the scrotum, and under magnification, tubules of the epididymis are carefully opened to aspirate sperm.
MESA allows the retrieval of a larger quantity of high-quality sperm, which can be used immediately or frozen for future fertility treatments like IVF with ICSI.
MESA is especially useful when a larger number of sperm are needed for multiple cycles, or when previous aspiration methods have not been successful.
Sperm extraction (TESE, Micro-TESE)
TESE
Testicular Sperm Extraction (TESE) is a surgical sperm retrieval procedure, which involves retrieving sperm directly from the testicles.
It is also done under local anaesthesia. A small tissue sample is taken from the testicle using a fine needle.
This sample, which contains sperm-producing tubules, is then examined under a microscope to find sperm.
If viable sperm are found, they are either used immediately or frozen for future IVF with ICSI.
Micro-TESE
Microdissection TESE (Micro-TESE) is an advanced form of TESE.
The procedure uses an operating microscope to carefully select the seminiferous tubules most likely to contain sperm, reducing damage to the testicle.
Micro-TESE is particularly beneficial for men with non-obstructive azoospermia, offering higher success rates compared to conventional TESE.
Retrieved sperm can be used immediately or cryopreserved for future IVF.
Both methods are safe and effective options for men who have had a vasectomy and wish to father a child through assisted reproduction.
How to support successful conception after IUI?
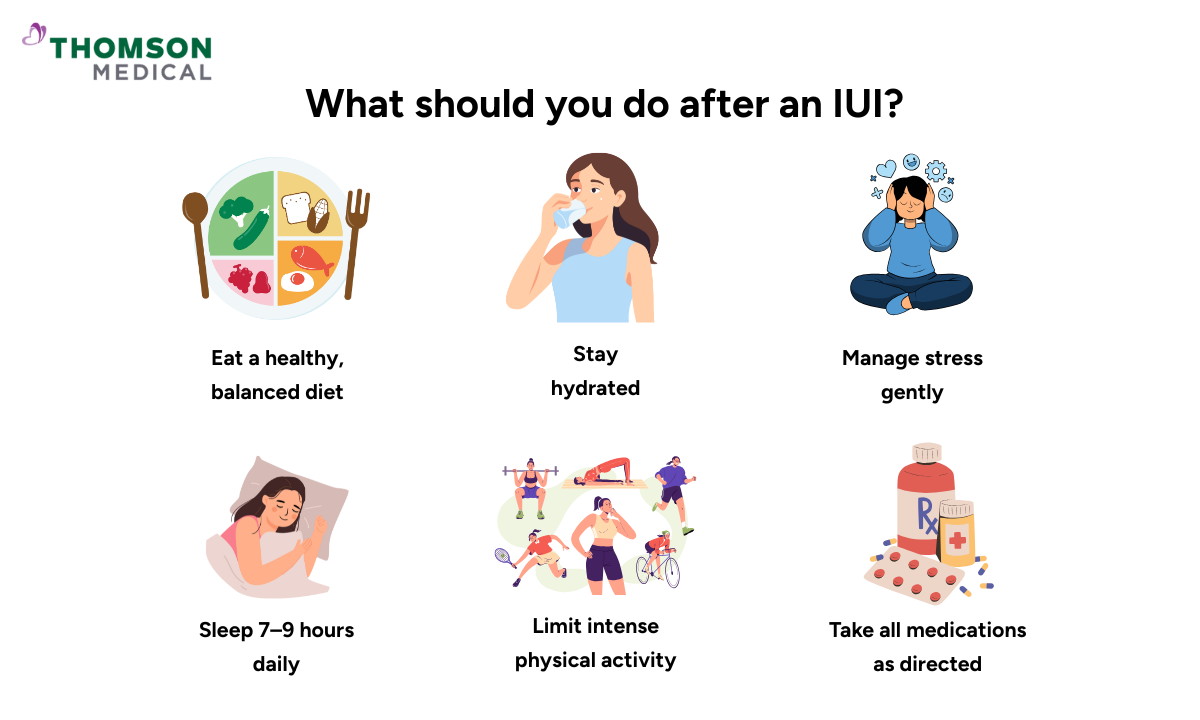
Taking care of your overall well-being plays a key role in supporting conception after IUI. Here are a few simple ways to optimise your lifestyle:
Eat a balanced diet:
Make sure your diet includes protein, antioxidants, omega-3 fatty acids, and vitamins.
Stay hydrated:
Drink around 2–3 litres of water daily. Hydration helps keep your body’s systems, including your reproductive system, functioning smoothly.
Maintain a healthy weight:
Keeping your BMI in a healthy range can improve your chances of conception and support hormonal balance.
Exercise regularly:
You don’t need intense workouts right now. Sticking to moderate, feel-good activities like brisk walking and swimming can help improve the IUI success rates.
Get enough sleep:
Try to get 7–9 hours of quality sleep each night. Rest is vital for hormone regulation and overall reproductive health.
Avoid alcohol and smoking:
Both can negatively affect fertility and lower the chances of a successful IUI.
Manage stress positively:
Try deep breathing, meditation, journaling, or simply doing things you enjoy. Staying calm and mentally supported during the two-week wait can make a real difference.
Stress management techniques such as meditation, staying in a positive mindset, and deep breathing exercises are beneficial.
FAQ
Does IUI work with a vasectomy?
Yes, pregnancy is still possible through IUI after a vasectomy, but it requires sperm retrieval since sperm is no longer present in the semen. This is usually done through a vasectomy reversal or surgical procedures like Percutaneous Epididymal Sperm Aspiration (PESA), TESA (Testicular Sperm Aspiration), or TESE (Testicular Sperm Extraction). If surgical retrieval isn’t an option, donor sperm from a sperm bank can be used for IUI.
Is it possible to get pregnant if my husband had a vasectomy?
While rare, pregnancy can still occur after a vasectomy. There is a small chance of pregnancy (less than 1 in 1,000 women in the first year) due to the possible reconnection of the vas deferens or the presence of remaining sperm in the reproductive tract. A follow-up semen analysis is essential to confirm the success of the procedure.
What are the options for fertility after a vasectomy?
The main fertility options after a vasectomy include:
Vasectomy reversal, which reconnects the vas deferens
Surgical sperm retrieval using techniques like PESA, TESA, or TESE
Followed by Artificial Insemination methods such as IUI or IVF with ICSI
These methods are especially helpful for couples dealing with male factor infertility or fertility issues following sterilisation.
Can you reverse a vasectomy naturally?
No, a vasectomy cannot be reversed naturally. It is considered a permanent method of male contraception, and reversal requires a surgical procedure performed by a specialist in male fertility.
Is gender selection possible in IUI?
Yes, gender selection is possible with intrauterine insemination (IUI), through MicroSort, separating sperm based on their X and Y chromosomes. However, this method is not 100 percent accurate, and there remains a possibility of conceiving a child of the undesired sex.
Is sperm quality affected by retrieval methods like PESA or TESE?
Yes, to some extent. Sperm collected via PESA, TESA, or TESE may have lower motility and be fewer in number compared to ejaculated sperm. However, with advanced assisted reproductive technologies (ART) like IVF with ICSI, even a single healthy sperm can lead to successful fertilisation.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
