If you and your partner have been trying to conceive for over a year without success, it can feel frustrating and disheartening. There are many reasons why you might be having difficulty conceiving, and one possibility is male-factor infertility, which is characterised by an absence or low number of sperm in the semen (azoospermia).
To support you during this fertility journey, your fertility specialist may recommend fertility treatments combined with sperm retrieval procedures to help you welcome your little angel into the world.
What is an aspirated sperm?
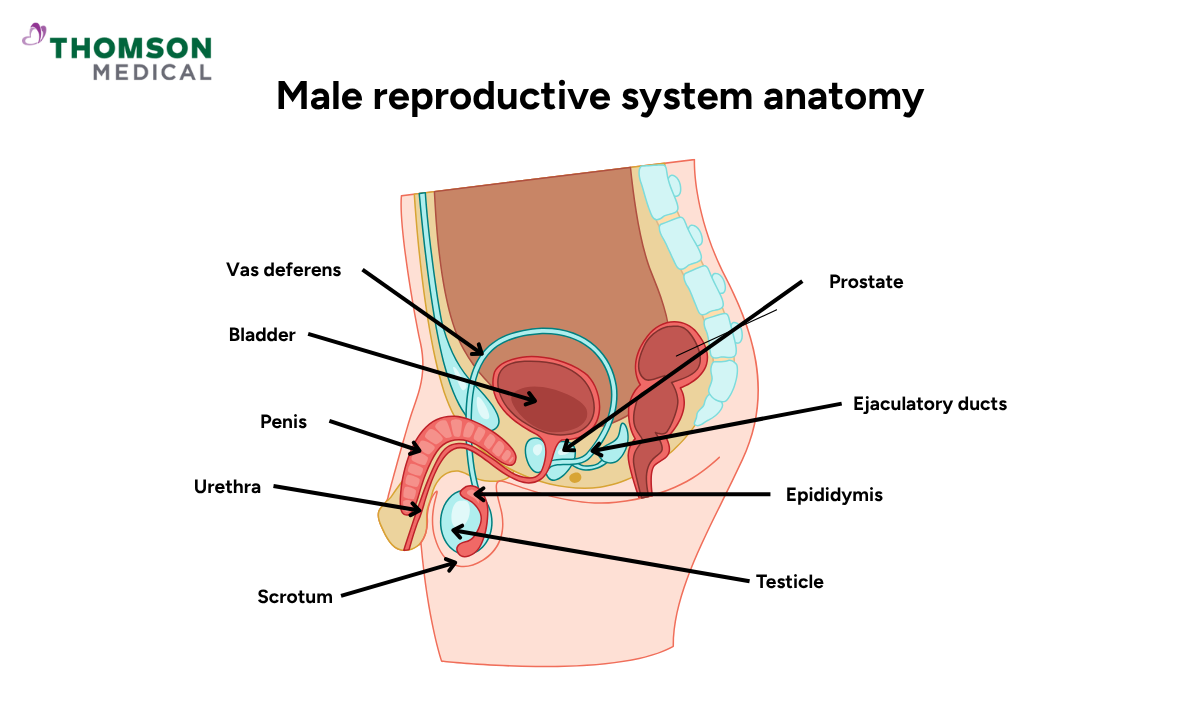
Aspirated sperm is sperm that's retrieved artificially through a surgical procedure (sperm extraction) or through needle-guided procedures that withdraw sperm directly from the testicles or epididymis, also known as sperm aspiration.
Your doctor will usually recommend this procedure if you are experiencing male infertility issues that prevent sperm from appearing in your semen during ejaculation. This condition can be caused by:
Obstructive azoospermia
This condition occurs when your testicles produce sperm normally, but a physical blockage causes the sperm to be trapped within your reproductive tract, usually in the epididymis or vas deferens. Common causes include:
Abnormal cyst or growth
Trauma or injury to the testicle
Blockages from injury or surgery
Infections that leads to inflammation, such as epididymitis (inflammation of the epididymis)
Reproductive tract blockage due to a vasectomy or the congenital absence of the vas deferens.
Non-obstructive azoospermia
As the name implies, non-obstructive azoospermia means that there’s no blockage or obstruction interfering with the sperm transportation from the epididymis to the urethra. Instead, this condition results from severely impaired or absent sperm production within your testicles. Common causes include:
Severe varicocele (enlarged veins in the scrotum)
Hormonal imbalances, such as low testosterone
Previous chemotherapy or radiation treatment
Certain medications or steroid use that affect sperm production
Genetic conditions such as Klinefelter syndrome or Kallmann syndrome
Lifestyle factors such as excessive alcohol consumption, smoking, or prolonged exposure to high temperatures
Additionally, a sperm retrieval procedure may be required for certain fertility conditions, such as severe oligospermia (a very low sperm count) or necrospermia (a high percentage of deceased sperm).
For further information on whether sperm retrieval procedures could help you conceive, schedule an appointment with Thomson Fertility Centre. Our fertility specialists can help determine whether these procedures are suitable for your fertility condition.
How does the doctor retrieve your sperm?
If you have been diagnosed with male infertility, depending on the cause of your condition, there are a few methods your fertility doctor can use to retrieve your sperm.
For obstructive azoospermia:
If your fertility issues are caused by blockages in the reproductive tract that prevent sperm from being released through ejaculation, your doctor can perform several procedures.
Percutaneous epididymal sperm aspiration (PESA):
PESA is a minimally invasive procedure where your doctor carefully inserted a fine needle through the scrotum's skin directly into the epididymis to retrieve sperm.
However, since this procedure is performed without direct visualisation, your doctor cannot say exactly where the needle is located in the epididymis. This limitation can sometimes make it difficult to obtain sufficient sperm for use in fertility treatment.
Microsurgical epididymal sperm aspiration (MESA):
During a MESA procedure, your surgeon will make a small incision in your scrotum and use a surgical microscope to visualise and access your epididymis directly.
This method is often chosen because the microscope enables your doctor to identify the best locations for sperm collection and recover larger quantities of mature, high-quality sperm compared to PESA.
Testicular sperm aspiration (TESA):
Unlike MESA and PESA, TESA involves aspirating sperm directly from your testicles rather than the epididymis.
To perform it, your doctor makes a small puncture in your scrotal skin and uses a spring-loaded biopsy needle to collect testicular tissue that contains sperm.
TESA can successfully retrieve sperm, but it often only collects a small sample of tissue, limiting the quantity. This can sometimes make it challenging to use the retrieved sperm for fertility treatment.
For non-obstructive azoospermia
If your fertility issues are caused by non-obstructive azoospermia, which is characterised by severely impaired or absent sperm production in the testicles, then surgical sperm retrieval becomes necessary.
Testicular sperm extraction (TESE):
TESE involves making a small incision in the scrotum and surgically removing a small piece of testicular tissue to be examined for the presence of sperm.
The tissue is immediately examined in the laboratory to identify viable sperm that can be used for fertilisation.
You may experience discomfort after the procedure, but don't worry, your doctor will provide you with comprehensive post-procedure care instructions and follow-up appointments.
Microsurgical TESE:
Microsurgical TESE, also known as micro-TESE, is the most complex sperm retrieval technique. This technique employs microsurgery to accurately extract sperm from the testicular tissue.
While you're under general anaesthesia, your surgeon uses a surgical microscope to carefully examine your testicular tissue and identify areas most likely to contain sperm. The microscope helps locate which tubules within your testicle have the best chance of containing viable sperm.
During the procedure, small tissue samples are sent to the laboratory to determine whether sufficient sperm have been harvested for your treatment cycle.
Our fertility specialists
Loading...
Can you do intrauterine insemination (IUI) with aspirated sperm?
Yes, aspirated sperm can be used for an IUI procedure, though there are considerations regarding its use. This is because sperm obtained from aspiration procedures, particularly in cases of non-obstructive azoospermia, may not be suitable for IUI due to their potential lack of motility and low quality.
However, IUI with aspirated sperm is possible if the retrieved sperm is sufficiently mobile and has a normal shape. If the sperm is properly processed and washed to concentrate the healthiest sperm, it can be used for IUI as effectively as sperm obtained through natural ejaculation.
For the best results, many fertility specialists recommend combining sperm aspiration with intracytoplasmic sperm injection (ICSI) during IVF rather than IUI. ICSI offers a higher chance of successful fertilisation because a single healthy sperm is injected directly into an egg, eliminating the need for it to swim and penetrate naturally.
To help increase your chances of conceiving, our fertility specialists at Thomson Fertility Centre can evaluate your aspirated sperm sample and recommend the most suitable fertility treatment. Schedule an appointment with us today.
What are the alternatives to IUI using aspirated sperm?
If your doctor determines that IUI with aspirated sperm isn't the most suitable option for your fertility condition, there are other assisted reproductive technologies (ART) available to help you achieve pregnancy, including:
In vitro fertilisation (IVF)
In vitro fertilisation (IVF) is a type of ART where sperm and eggs are fertilised outside of the body. During the IVF process, your doctor will extract a mature egg from your ovaries. The aspirated sperm and eggs are combined in an incubator to facilitate fertilisation following the egg retrieval process.
After successful fertilisation, the fertilised egg (embryo) will be transferred back into your womb, where it can implant in the uterine lining and develop into a pregnancy. A complete IVF cycle usually lasts 4 to 6 weeks but can be longer if necessary.
Intracytoplasmic sperm injection (ICSI)
ICSI is a specialised type of IVF that effectively utilises aspirated sperm. It's because, during ICSI, a single healthy aspirated sperm is directly injected into a mature egg to achieve fertilisation instead of placing sperm and eggs together and waiting for natural fertilisation to occur.
Regular IVF essentially puts sperm and eggs together in a dish and lets them find each other naturally, while ICSI is more like a matchmaker who introduces them directly. This technique is particularly beneficial for severe male infertility, where natural fertilisation may be difficult.
Once fertilisation occurs, the resulting embryo is carefully monitored before being transferred to the womb to support the beginning of a healthy pregnancy.
FAQ
How can sperm aspiration lead to pregnancy?
Sperm aspiration is a medical procedure that can help those with male fertility issues, such as blockages in the reproductive tract or very low sperm counts. During the procedure, sperm are collected directly from the epididymis or testicles using methods such as PESA, MESA, or TESE.
The sperm can then be used for ART procedures, including IUI, IVF, or ICSI. Among these, IVF with ICSI is generally the most successful approach, particularly if the quantity or quality of the aspirated sperm is limited. ICSI is particularly helpful because it only takes a single healthy sperm to fertilise an egg.
Can unwashed sperm be used for IUI?
No, unwashed sperm is not suitable for IUI. Sperm washing is a necessary laboratory procedure that removes seminal fluid, containing proteins and other substances that could irritate the womb or trigger an immune response.
This step is particularly important for aspirated sperm, as it ensures that only the healthiest and most motile sperm are used for insemination.
Can you do IUI with frozen sperm?
Yes, IUI can be performed using frozen sperm. Before use, however, the sperm must be properly thawed and processed to ensure there are enough healthy, mobile sperm.
Although fresh sperm is generally preferred for IUI, frozen sperm is still a viable and commonly used option.
Is IUI possible with a TESE?
Yes, it is possible to use sperm retrieved via TESE for IUI, provided that the sample has sufficient motility and that the sperm are healthy enough to fertilise the egg.
However, since sperm collected through TESE often have reduced motility or numbers, IVF or ICSI are generally recommended to increase the chances of pregnancy.
Which is better, TESE or PESA, for sperm aspiration?
TESE and PESA have different applications, depending on the cause of fertility issues.
- TESE is often preferred for non-obstructive azoospermia, where there is a very low or absent level of sperm production in the testicles.
- While PESA is used for obstructive azoospermia, where sperm production is normal but a blockage prevents sperm from being released through ejaculation.
Based on your diagnosis and the affected part of the reproductive tract, your doctor will recommend the most suitable approach.
What is the best sperm sample for IUI?
The ideal sperm sample for IUI has high motility, good morphology, and a sufficient sperm count. Sperm quality is vital for IUI, as sperm must swim through the cervix and into the uterus to reach the egg.
Fresh sperm (obtained through ejaculation) is generally preferred to frozen or aspirated sperm for IUI.
The information provided is for general guidance only and should not be considered as medical advice. For a personalised fertility consultation and tailored advice, schedule an appointment with Thomson Fertility Centre today.
For more information, contact us:
Thomson Fertility
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Request an Appointment