A failed IUI doesn’t mean the end of your dream to conceive.Understanding why it happens can bring you peace of mind, restore hope, and help guide you towards the next step in your journey to parenthood.
Why does IUI fail?
Even when everything seems perfect, intrauterine insemination (IUI) doesn’t always lead to pregnancy. While the procedure helps sperm get closer to the egg, it can’t guarantee fertilisation or implantation. IUI failure can happen at several points:
Ovulation might not happen as expected:
Timing is critical, and sometimes the egg isn’t released when predicted.
Sperm may not fertilise the egg:
Even healthy sperm can occasionally fail to meet or penetrate the egg.
The fertilised egg might not implant:
Sometimes the embryo doesn’t attach to the uterine lining.
Implantation may not continue:
Hormonal imbalances or uterine conditions can prevent the pregnancy from developing.
What are the common reasons for IUI failure?
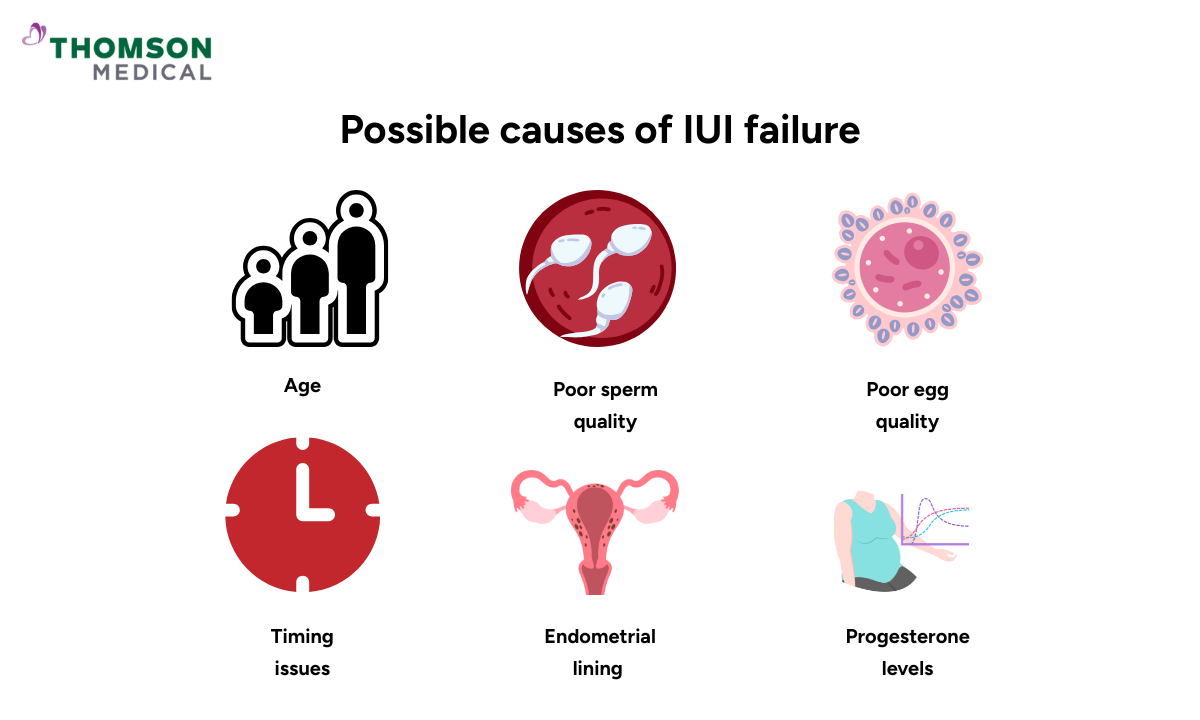
Several factors can affect the success of IUI. Therefore, understanding them can help you and your doctor adjust your treatment plan for better results.
Age
Female age is one of the biggest factors. Fertility starts to decline after 35 and drops more sharply after 40.
As we age, egg quality and quantity decrease, leading to a higher risk of chromosomal abnormalities.
The uterine environment may also become less receptive to implantation over time.
Poor sperm quality
Even after sperm washing and concentration, low motility or abnormal shape can limit fertilisation chances.
DNA fragmentation in sperm (not picked up in standard tests) can cause fertilisation failure or poor embryo development.
In cases of severely poor sperm quality, IVF with ICSI (injecting a single sperm into an egg) might be recommended instead of IUI.
Poor egg quality
Eggs of lower quality may lead to:
Fertilisation failure
Poor embryo development
Implantation problems
Common causes include age, genetic issues, smoking, excessive alcohol or caffeine intake, and ovarian conditions such as PCOS or diminished ovarian reserve.
Timing issues
Precise timing is critical for IUI success. The procedure is ideally done 24–36 hours after the ovulation trigger (hCG injection).
If done too early, sperm may die before ovulation. If too late, the egg may no longer be viable (egg lifespan is about 24 hours of ovulation).
Abnormal endometrial lining
A healthy endometrial lining (7–14 mm thick) is essential for implantation and a successful pregnancy.
Thin lining, fibroids, adhesions, or polyps may interfere with embryo attachment.
Poor blood flow or inflammation (e.g., chronic endometritis) can also reduce receptivity.
Progesterone levels
After ovulation, progesterone supports the uterine lining and early embryo development.
Low progesterone can lead to poor luteal phase support or early miscarriage.
Doctors may prescribe progesterone supplements (vaginal or injectable) to improve outcomes.
Are there any symptoms that indicate IUI has failed?
Unfortunately, there are no clear symptoms that can confirm whether an IUI cycle has failed before your pregnancy test. Still, some signs may suggest that the cycle wasn’t successful:
Period-like cramps appearing before 14 days post‑IUI
Menstrual bleeding starting around day 12–14
Lack of pregnancy symptoms, though it’s important to note that many women feel no symptoms even when pregnant
Important: Pregnancy symptoms such as sore breasts, nausea, or cramping can also be caused by progesterone supplements or fertility medications, so they are not reliable indicators.
What should I do after my first IUI failure?
A failed IUI cycle can feel discouraging, but it doesn’t necessarily mean you won’t conceive. Many couples succeed after two or three attempts. Here’s what you can do next:
Review the cycle with your doctor:
Discuss sperm quality, ovulation timing, medication doses, and uterine lining results.
Repeat hormone tests:
If needed, reassess your fertility status.
Consider treatment adjustments:
Changing the timing of the ovulation trigger
Switching or adding stimulation medications (such as Clomid, letrozole, and gonadotropins)
Adding progesterone support for better implantation
Explore additional tests if they haven’t been done yet:
HSG (hysterosalpingogram) to check if fallopian tubes are open
Sperm DNA fragmentation test
Endometrial biopsy for chronic inflammation
AMH and AFC tests to check ovarian reserve
Remember, each cycle provides valuable insights that can improve your next attempt.
Every cycle gives your doctor valuable insights to refine your treatment plan. If you’ve experienced an IUI failure, consider requesting an appointment at Thomson Medical to review your results and explore the best next steps for your fertility journey.
Are there ways to prevent IUI failure?
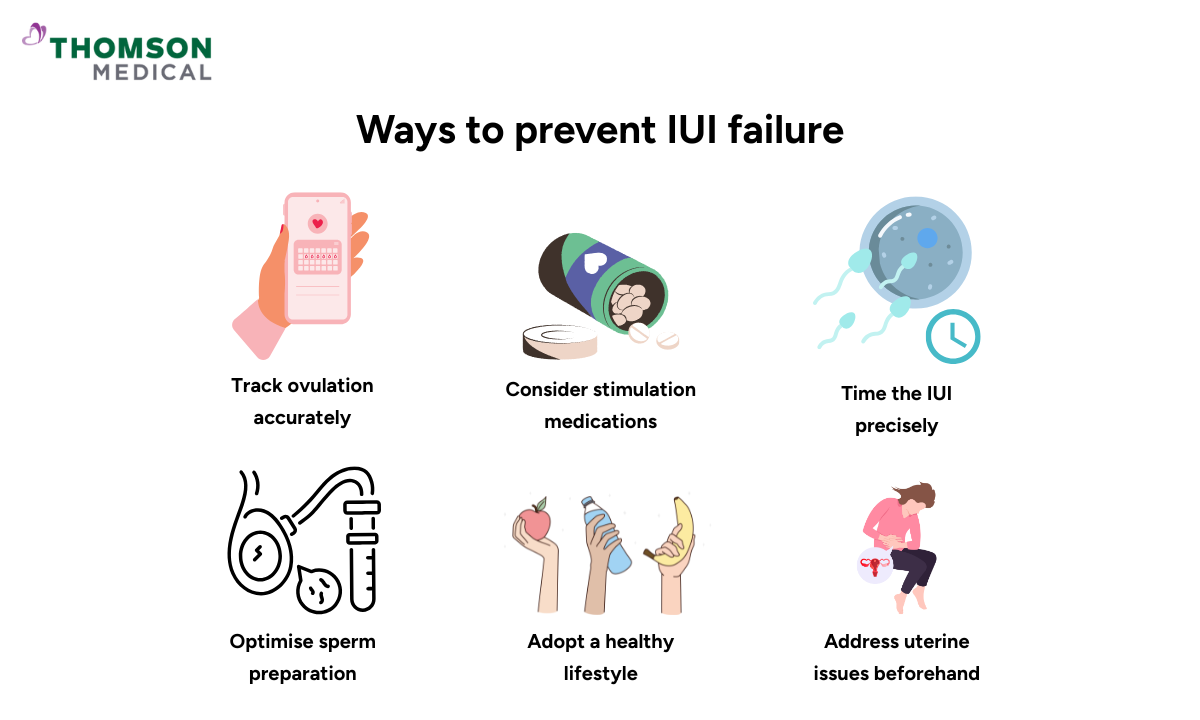
While it’s impossible to completely prevent IUI failure, there are ways to improve your chances of success:
Track ovulation accurately:
Use ultrasound scans or lutenising hormone (LH) surge tests to pinpoint the best timing.
Consider stimulation medications:
These can help produce multiple mature eggs, increasing fertilisation chances.
Time the IUI precisely:
The procedure should be done shortly after the ovulation trigger shot for the best results.
Optimise sperm preparation:
Ensure proper sperm washing and processing in a qualified fertility lab.
Adopt a healthy lifestyle:
Maintain a healthy BMI
Quit smoking and limit alcohol
Reduce caffeine to under 200 mg per day (about one to two cups of coffee)
Address uterine issues beforehand:
Procedures like hysteroscopy can remove polyps or fibroids and treat inflammation to improve implantation.
Small adjustments can make a big difference. Working closely with your fertility specialist ensures your IUI cycle is timed and tailored for the best possible outcome.
When should you consider moving from IUI to IVF?
IUI is often the first step in fertility treatment, but it may not always work for everyone. If you’re weighing IUI vs IVF, you might consider transitioning to IVF in these situations:
You’ve had 3–6 failed IUI cycles, especially if no changes were made to the protocol.
You’re over 35 and want to avoid losing valuable time while egg quality is still good.
There is severe male factor infertility, such as very low sperm count or motility.
You have blocked or damaged fallopian tubes, making natural fertilisation unlikely.
You have endometriosis or pelvic adhesions, which can affect egg release and implantation.
There’s a history of implantation failure or unexplained infertility where IUI hasn’t provided answers.
Understanding the differences between IUI vs. IVF can help you make an informed decision. IVF offers more control and higher success rates in these scenarios, allowing your doctor to closely monitor each stage of fertilisation and embryo development.
FAQ
If I had a previous IUI failure, can I still get pregnant?
Yes! A failed IUI doesn’t mean you can’t conceive in the future. Many people achieve pregnancy after two or three IUI cycles, especially when potential issues are identified and addressed. Adjusting medication, improving timing, or treating underlying conditions can significantly increase your chances of success in future IUI treatments.
What is the number 1 cause of IUI failure?
The most common cause of IUI failure is poor egg quality and/or poor sperm quality, often combined with incorrect timing of insemination. Even when everything appears normal, subtle factors affecting egg health, sperm function, or timing can reduce success rates.
What is the biggest cause of unexplained infertility?
Unexplained infertility often results from a combination of subtle issues that standard tests may not detect, such as:
Mild egg or sperm dysfunction
Poor endometrial receptivity (uterus may not support implantation)
Fertilisation failure or early embryo arrest
Mild or “silent” endometriosis
Can stress cause IUI to fail?
Normally, it depends on the type of stress:
Chronic stress can affect hormones, ovulation, and uterine receptivity, potentially lowering success rates.
Short-term stress (such as nervousness before or after IUI) is less likely to cause failure on its own, but relaxation techniques may help balance hormones and improve overall well-being.
What is the failure rate of IUI?
IUI success varies with age and underlying fertility factors:
10–20% per cycle in women under 35 with no major fertility issues
5–10% per cycle in women over 40
Cumulative success rate of 30–40% after 3–4 cycles
Can I conceive naturally after a failed IUI?
Yes. Many couples with mild or unexplained infertility eventually conceive naturally, even after one or more failed IUI attempts.
When will I get my period if IUI fails?
Most people get their period about 14 days after IUI if the cycle isn’t successful.
If you’re taking progesterone, your period may be slightly delayed.
If there’s no period by day 15, take a pregnancy test to confirm.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
Our gynaecologists
Loading...
For more information, contact us:
Thomson Fertility
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Request an Appointment