Reaching the end of treatment for an ovarian cyst often brings a sense of relief. Still, noticing familiar symptoms again can raise questions and concern about whether this is something you may face more than once.
Understanding how often ovarian cysts recur, why it happens, and when follow-up is needed can help ease uncertainty and support you in caring for your long-term ovarian health.
What is an ovarian cyst?
An ovarian cyst is a fluid-filled sac that develops on or inside an ovary. Because your ovaries play an important role in ovulation and hormone production, it is natural to feel concerned when changes occur, especially if you have previously already undergone treatment or cyst removal.
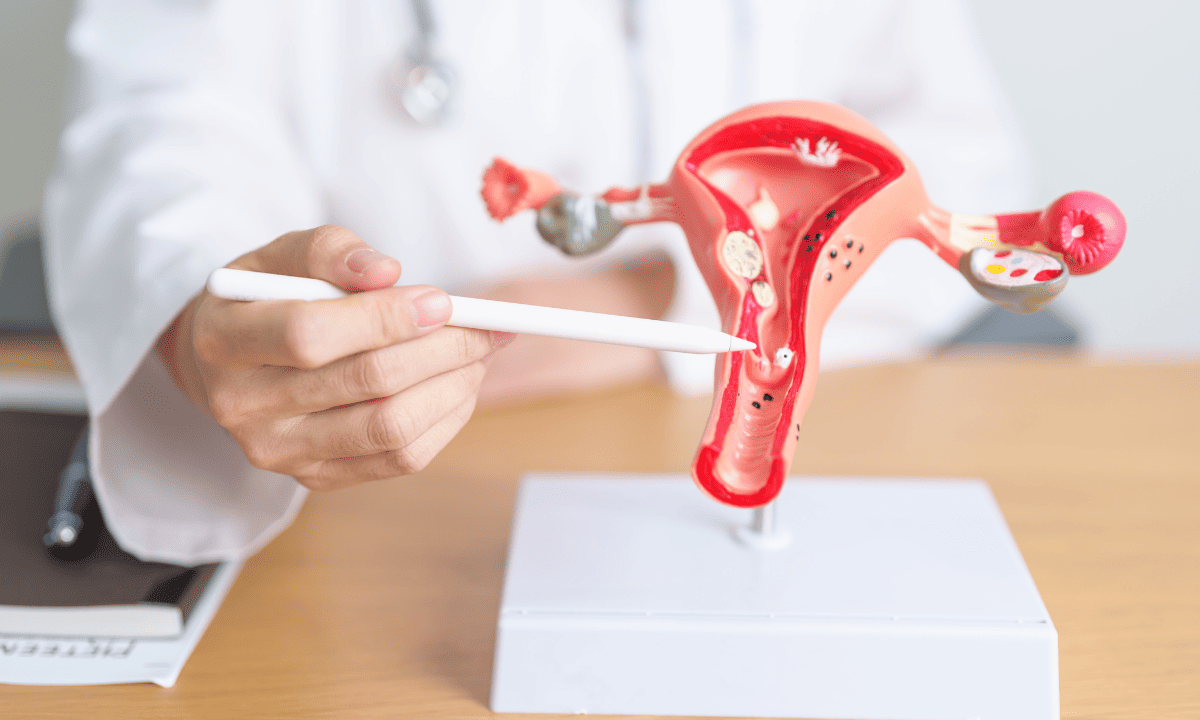
There are two main types of ovarian cysts that doctors commonly see:
Functional cysts:
These are the most common and form during your normal menstrual cycle.
They include follicular cysts (when an egg is not released) and corpus luteum cysts (which form after the egg is released).
Usually harmless and often disappear on their own.
Complex cysts:
These are not related to ovulation and may contain solid areas or have an unusual shape.
Examples include endometrioma cysts and dermoid cysts.
Most are benign but may require closer monitoring or treatment.
The good news is that ovarian cysts are very common, and most are not linked to ovarian cancer. Many cause no symptoms and go away without treatment.
If a cyst persists, grows, or begins to cause discomfort such as pelvic pain or bloating, it’s important to seek medical advice. Your healthcare professional can help you understand what may be happening and guide you towards appropriate care, offering reassurance and support along the way.
Can an ovarian cyst come back?
Yes, ovarian cysts can come back even after they have resolved on their own or been surgically removed. This can feel frustrating, especially if you believed the cyst had been fully treated.
While the word “recurrence” can sound scary, most recurring cysts remain harmless. With regular follow-up and monitoring, your doctor can keep an eye on any changes and step in early if a cyst starts to grow or cause symptoms, helping you stay reassured and in control of your health.
It helps to know that certain types of cysts, especially functional cysts, are closely linked to the natural hormonal changes of your menstrual cycle. Because those hormonal patterns continue, new cysts can sometimes form again.
If you are experiencing recurring ovarian cysts or have ongoing concerns about your symptoms, schedule a consultation at Thomson Medical to discuss monitoring options, possible causes, and a personalised plan to support your long-term ovarian health.
Recurrence rates in Singapore
The chance of a cyst returning isn’t the same for everyone, but it depends largely on the type of cyst you had and how it was treated:
Functional cysts:
These are linked to normal ovulation, so they can return as your cycle continues.
About 10% to 15% of women may experience them again.
They are usually harmless and often settle on their own.
Complex cysts:
Tend to recur over months to years, depending on the cyst type.
Ovarian endometriomas have a higher chance of recurrence, around 30% to 50%, particularly if only part of your cyst is removed surgically.
Knowing which type of cyst you have allows your doctor to explain what it means for your body, whether it is likely to resolve on its own or needs monitoring, and what symptoms to watch for. This can help you better understand what you are dealing with and feel more reassured as you take the next steps forward.
How do I know if I have another ovarian cyst?

In their early stages, many recurrent cysts don’t cause any symptoms and are only found during a routine scan. However, if you notice any of the following symptoms, it is important to reach out to your doctor right away:
A dull ache or pressure in your lower abdomen
Persistent bloating that doesn't seem linked to your diet
Pain or deep discomfort during sexual intercourse
If you experience sudden, sharp, or severe pelvic pain, it could mean you may be struggling with a ruptured ovarian cyst or ovarian torsion (twisting). These conditions can cut off blood flow to the ovary or cause internal bleeding, which requires immediate medical attention to keep you safe.
Because symptoms can be subtle or overlap with other conditions, you may not always notice a cyst on your own. Your doctor may recommend imaging tests along with a pelvic exam to better understand what is happening and rule out other causes.
Our gynaecologic oncology specialist
Loading...
When does it usually come back after surgery?
You may experience recurrence differently from others, as the timeline for when an ovarian cyst might reappear varies from person to person.
Functional cysts:
Tend to be more immediate, sometimes showing up within just a few menstrual cycles.
Endometriomas:
Often "slower" to return, sometimes taking months or even years to become noticeable again.
Whether a cyst comes back can depend on how fully it was removed and how your hormones naturally fluctuate. If you are worried that it may return, speak to your doctor so they can suggest follow-up scans to monitor you closely.
Why do they come back?
Cysts can form when normal ovulation or hormone changes in the ovaries do not happen as they usually do. Here are several factors that might influence why a cyst returns:
Hormonal imbalances:
If your menstrual cycles are irregular, it can lead to the formation of new functional cysts.
The "leftover" factor:
During surgery, if even a tiny amount of your cyst tissue isn't fully removed, a new cyst can grow in the same spot.
Underlying health conditions:
If you live with endometriosis or polycystic ovary syndrome (PCOS), your body is naturally more prone to developing cysts repeatedly.
Lifestyle and stress:
While not a direct cause, ongoing stress or metabolic factors such as obesity can affect your hormone balance, raising the chance of cysts returning.
Understanding these factors can help explain why cysts may come back and support a more personalised plan for your care. This will help you feel clearer about what’s happening and more supported moving forward.
How to prevent ovarian cyst recurrence?
It is not always possible to prevent ovarian cysts entirely, but you can follow these steps to reduce your chances of an ovarian cyst coming back:
Attend regular screenings, including pelvic ultrasounds and check-ups, to help your doctor detect any abnormal changes and rule out rare conditions such as ovarian cancer.
Explore hormonal therapies like oral contraceptives to calm your ovaries and prevent new functional cysts from forming.
Manage the root cause, particularly if you have endometriosis or PCOS.
Have a balanced diet and do regular exercise to keep your hormones in a healthier rhythm.
Taking these steps can give you a greater sense of control over your health and reassurance that you’re doing what you can to support your body over time.
If you are concerned about recurrent ovarian cysts or want guidance on medical treatment, schedule a consultation at Thomson Medical today to discuss a personalised care plan based on your health history and needs.
How to treat recurrent ovarian cysts?
If a cyst does return, your care team will work with you to create a plan that prioritises your comfort, your future fertility, and your overall quality of life.
The "wait and see" approach:
For small, simple cysts, your doctor may simply monitor them with regular ultrasounds to see if they resolve on their own.
Hormonal medications:
Your doctor will prescribe medical treatments, such as oral contraceptives, to prevent future cysts and manage current symptoms.
Laparoscopic surgery:
A minimally invasive approach that uses small incisions to reduce discomfort, minimise scarring, and help you return to your normal activities sooner.
If a cyst is growing quickly, causing you pain, or looks complex on a scan, surgical removal may be considered.
Your doctor will take the time to explain the risks and benefits of each option, especially if you are planning a pregnancy or have other health needs. This can help you feel confident that your overall wellbeing leads the decisions of your care team.
FAQ
How common is it for a cyst to grow back?
It is fairly common for ovarian cysts to return, especially functional cysts linked to your menstrual cycle. Endometriomas are more likely to come back, particularly if endometriosis is not fully managed. While recurrence can feel worrying, most cysts remain harmless and can be monitored and managed safely.
Can certain foods trigger ovarian cysts?
There is no strong evidence that specific foods directly cause cysts. That said, diets high in processed foods, sugar, and unhealthy fats can affect your hormone balance. Eating a balanced diet with vegetables, fruits, whole grains, and lean proteins supports your reproductive health and may help lower the risk of recurrence.
Why would a cyst come back after removal?
A cyst can return if the hormonal imbalance or underlying condition that caused it remains. Sometimes, a small part of the cyst may stay behind after surgery, giving it a chance to grow again. Conditions such as endometriosis or PCOS also make new cysts more likely.
How can I prevent a cyst from coming back?
You cannot always prevent cysts entirely, but regular check-ups and scans allow your doctor to catch changes early. Hormonal treatments and managing conditions like endometriosis or PCOS can reduce the chance of recurrence. Maintaining a healthy lifestyle also supports your hormone balance and overall reproductive health.
What factors influence recurrence?
Several things can affect whether a cyst comes back:
Your type of cyst
Your body’s hormonal level
Whether any cyst tissue remained after surgery
Underlying conditions such as endometriosis or PCOS
Changes in your cycle or reproductive stage
Lifestyle factors like stress, weight, and overall health
Understanding these factors can help you and your doctor plan follow-up care and reduce the risk of recurrence while keeping you reassured.
What should I do if my cysts recur?
If you notice a cyst coming back, keep in close contact with your doctor. Regular imaging, including pelvic exams, helps spot any changes early. Depending on the cyst and your symptoms, your doctor may recommend monitoring, hormonal treatment, or surgery. Acting early helps prevent complications such as ovarian cancer and keeps your reproductive health on track.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment