The itch has woken you up at 3 am again. You've tried countless creams, avoided certain foods, and changed your skincare routine, yet your eczema keeps coming back (flaring up).
To address this chronic issue, Traditional Chinese Medicine (TCM) takes a different approach. Rather than just treating the symptoms, it works to identify the internal imbalances and triggers that may be causing your flare-ups.
What is eczema?

If you experience eczema, your skin barrier becomes weakened, causing it to lose moisture more easily. This makes it more susceptible to irritants, which can penetrate the skin and cause inflammation, leaving you with dry, red, and itchy patches.
Flare-ups can be triggered by things like dust mites, heat and humidity, stress, poor sleep, and even your soap. If your parents had eczema, asthma, or hay fever, you're more likely to develop it too. You may have atopic dermatitis (the most common type), contact dermatitis from something you've touched, or other eczema types.
The frustrating part is that even when you avoid triggers and use creams, it keeps coming back. This is where TCM takes a different approach.
How does TCM view eczema differently?
TCM doesn't just look at your skin. It looks at your whole body as a connected system, including how Qi (your body’s energy) and blood flow through your body. When the circulation is good, you feel healthy and energetic. When it's blocked or weak, issues like eczema can show up.
In TCM, your eczema is seen as a signal of internal imbalance. Physicians believe that weak digestion creates dampness (excess moisture) in your body. When this dampness combines with outside factors like wind, it shows up as eczema on your skin.
TCM physicians look for different patterns based on what they see.
Wind and dampness causes sudden, severe itching with red bumps, usually on the upper body
Damp-heat cause eczema to flare up quickly, with irritating red patches
Spleen deficiency with dampness shows up in long-term cases as pale, scaly, or thickened skin
The treatment works on clearing dampness and wind while making your digestion stronger to prevent the dampness from building up again. It tackles the root problem, not just the symptoms on your skin.
If you’re looking to address eczema at its root, request an appointment at Thomson Chinese Medicine. Our physicians can help to assess your overall balance and create a personalised treatment plan.
Our eczema physician
Loading...
What TCM treatments are available for eczema?
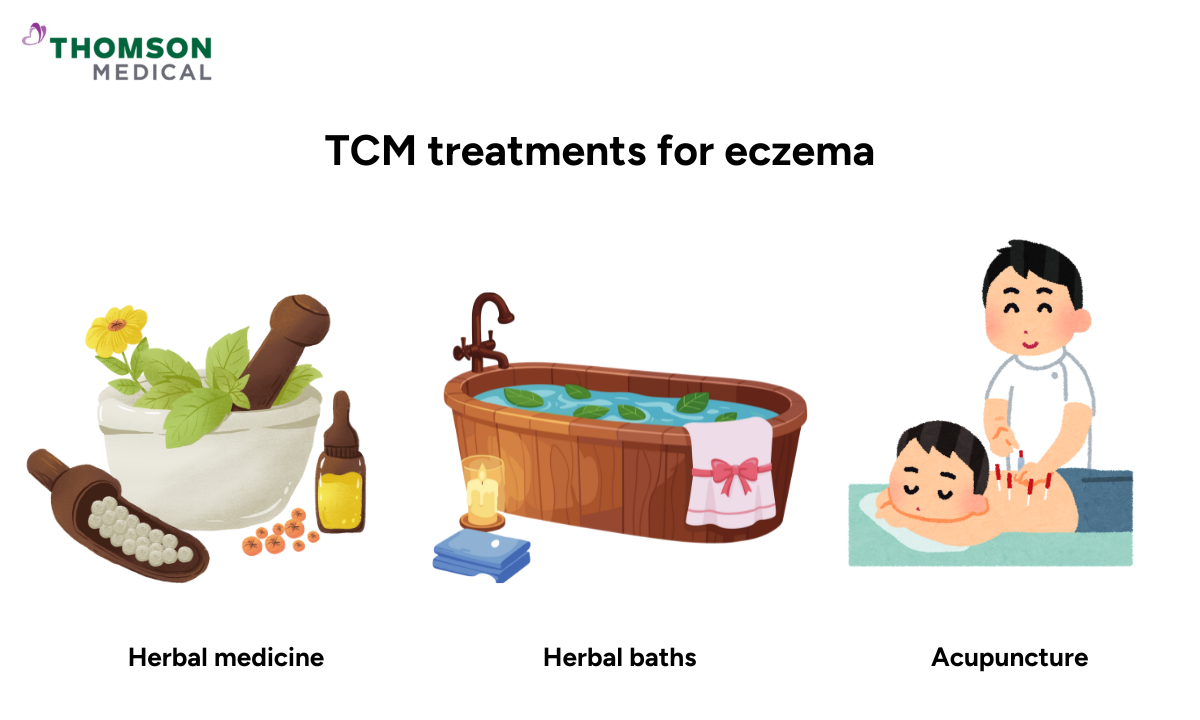
TCM offers several personalised approaches to managing eczema. Treatments are tailored to your symptoms and are adjusted over time to suit your needs.
Herbal medicine
Your TCM physician will create an herbal formula specifically for you. Unlike over-the-counter medicine, this herbal formula is based on your symptoms, body type, and internal health.
The herbs work to cool inflammation, clear dampness from your body, nourish your blood, and strengthen your digestion. You might receive formulas like Xiao Feng San if wind and itching are your main issues, or Dang Gui Yin Zi if your skin is very dry and needs moisture. Specific herbs like Ku Shen and Huang Bai are commonly used because they naturally cool and reduce inflammation.
Acupuncture
Acupuncture stimulates specific points on your body that influence your immune system and inflammation. It helps to control your body’s response to triggers and supports natural healing.
The treatment also improves blood circulation to your skin, which helps bring nutrients and oxygen to affected areas. Better blood circulation supports overall skin health. Many people find acupuncture relaxing, which also helps since stress is a common eczema trigger.
Dietary adjustments
What you eat matters more than you might think when it comes to eczema. Because TCM sees a strong link between your gut health and your skin, the food choices you make directly affect whether dampness builds up in your body.
This usually means adding more cooling foods like leafy greens and certain fruits, while cutting back on foods that create heat and dampness like spicy dishes, fried foods, and shellfish. Because TCM sees a strong link between your gut health and your skin, supporting your digestion through food choices can help reduce eczema flare-ups.
Herbal baths
Herbal baths are a gentler alternative for alleviating your symptoms, particularly if you find it difficult to take herbal medicine orally. You will soak in warm water infused with Chinese herbs that work directly on your skin.
As you relax, your skin will absorb the healing compounds from the herbs, which will calm the itch and reduce redness. You can also prepare herbal baths at home; your physician can recommend specific formulations. They will advise you on which herbs to use, how to prepare them properly and how often to use them, depending on your individual condition.
Eczema TCM treatment doesn't just focus on the skin; it also addresses the underlying issue inside your body. Request an appointment with a TCM physician at Thomson Chinese Medicine to get an assessment to address internal balance and long-term relief.
What treatments should you avoid?
While TCM offers many helpful options, some approaches might not give you the results you're looking for.
Generic herbal products like teas or creams aren't tailored to your specific type of eczema. What works for someone else might not work for you, and these products may not help or could even make things worse.
Too many cooling foods or herbs can have the opposite effect. Using too much can weaken your digestion and create more dampness, which is exactly what TCM is trying to clear from your body. Balance is what matters most when changing your diet.
Some herbs are very potent and require specialist knowledge for safe use. Don't use them on your own without talking to a professional first. A qualified TCM physician knows how to use them correctly for your situation.
How long does TCM treatment take to work?
TCM works slowly but surely because it's teaching your body to heal itself from the inside out, not just covering up symptoms. You'll likely start feeling better within the first few weeks.
Most people start with sessions every two weeks, combining herbal drinks and herbal baths. In the first four to eight weeks, you'll probably notice:
Better sleep because you're not scratching all night
Less itchiness
Red patches fading
Less dryness
Improved skin barrier function
If you've had eczema for years or have been using steroids for a long time, expect around three months of active treatment. After that, you'll move into maintenance care to keep your body strong and stop future flare-ups.
Who can benefit from TCM eczema treatment?
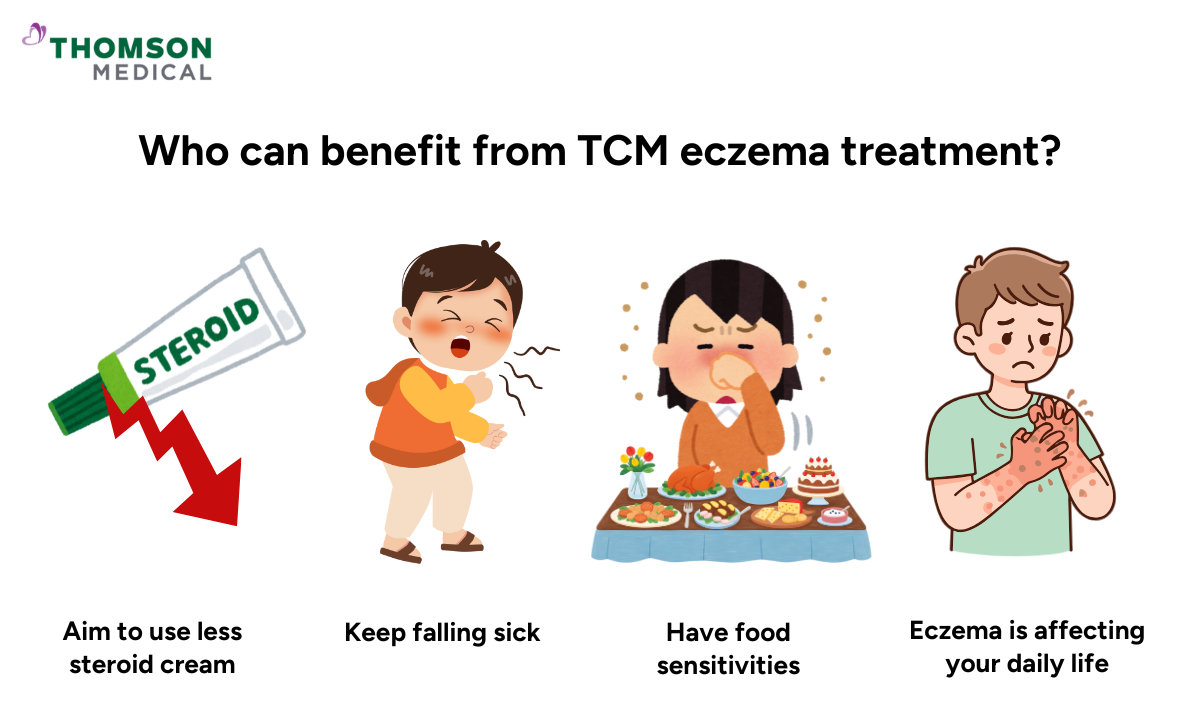
You might be wondering if TCM is right for you. It's especially worth considering if you:
Haven't found relief with conventional treatments
Want to reduce how much you depend on steroid creams
Keep falling sick or feel constantly tired (signs of Qi deficiency)
Have food sensitivities alongside your eczema
Feel like your eczema is affecting your daily life
TCM can work alongside your current treatments. You don't have to choose between Western medicine and TCM. Many people use both and find this combined approach gives them the best results. Just make sure your doctors know what you're taking so they can coordinate your care.
TCM can work alongside your current eczema treatment. Request an appointment with Thomson Chinese Medicine to see how a combined approach may support your skin and overall health.
FAQ
Can TCM cure my eczema?
While TCM doesn't guarantee a cure, it can significantly improve your symptoms and reduce how often you get flare-ups. Many people find they can manage their eczema much better with consistent TCM treatment.
Is TCM safe for children with eczema?
Yes, TCM is generally safe for children when prescribed by a qualified physician. Herbal baths are especially gentle and effective for young children. The formulas are adjusted to suit your child's age and constitution.
Can TCM be used alongside conventional eczema treatments?
Yes, many people use both together, especially for the first time. As your body responds to TCM treatment, you might find you need less steroid cream over time. Keep both your TCM physician and dermatologist informed about everything you're using.
How quickly will you see an improvement with TCM for your eczema?
Most people notice their itching and redness improving within a few weeks to a couple of months. For significant healing, especially if you've had eczema for years, you're looking at three to six months of consistent treatment.
Does TCM address the root cause of eczema?
Yes, TCM aims to address the underlying imbalances that cause your eczema, rather than simply suppressing the symptoms. That's why treatment takes longer, but the results tend to last.
What can you expect during your first TCM appointment?
Your physician will spend time learning about your symptoms, medical history, diet, sleep patterns, and stress levels. They'll examine your tongue and feel your pulse, which helps them assess what's happening inside your body. Then they'll create a personalised treatment plan based on this assessment.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, request an appointment with Thomson Chinese Medicine today.
Reference:
Hon, K., Chan, B., & Leung, P. (2011). Chinese herbal medicine research in eczema treatment. Chinese Medicine, 6(1), 17. https://doi.org/10.1186/1749-8546-6-17
Physician Jun Negoro
Traditional Chinese Medicine
Thomson Chinese Medicine (TCM Paragon Medical Centre) and 1 other
English, Mandarin
Alliance MediNet

