Falls among older adults are more common than many people realise. If you are caring for an elderly parent or family member, you may find yourself watching more closely, wondering what signs to look out for and when a fall needs medical attention.
Understanding why falls happen, which warning signs matter most, and when to seek urgent care can help you feel more confident in those moments of uncertainty. With the right information, you can take practical steps to protect the person who once looked after you.
Why falls are more than just accidents
As we age, our bodies change in ways that can affect balance, strength, and coordination. These natural changes, combined with certain health conditions and environmental factors, make falls more likely. While many falls result in minor bruises, some can lead to serious injuries such as hip fractures, head trauma, or loss of independence.
Understanding what increases fall risk gives you the chance to make meaningful changes. You don't need to address everything at once. Even small adjustments can genuinely help. If a fall has already happened, see it as a signal to reassess their environment and needs together, supporting not just their safety but their confidence and ability to live comfortably at home.
Common causes of falls in older adults
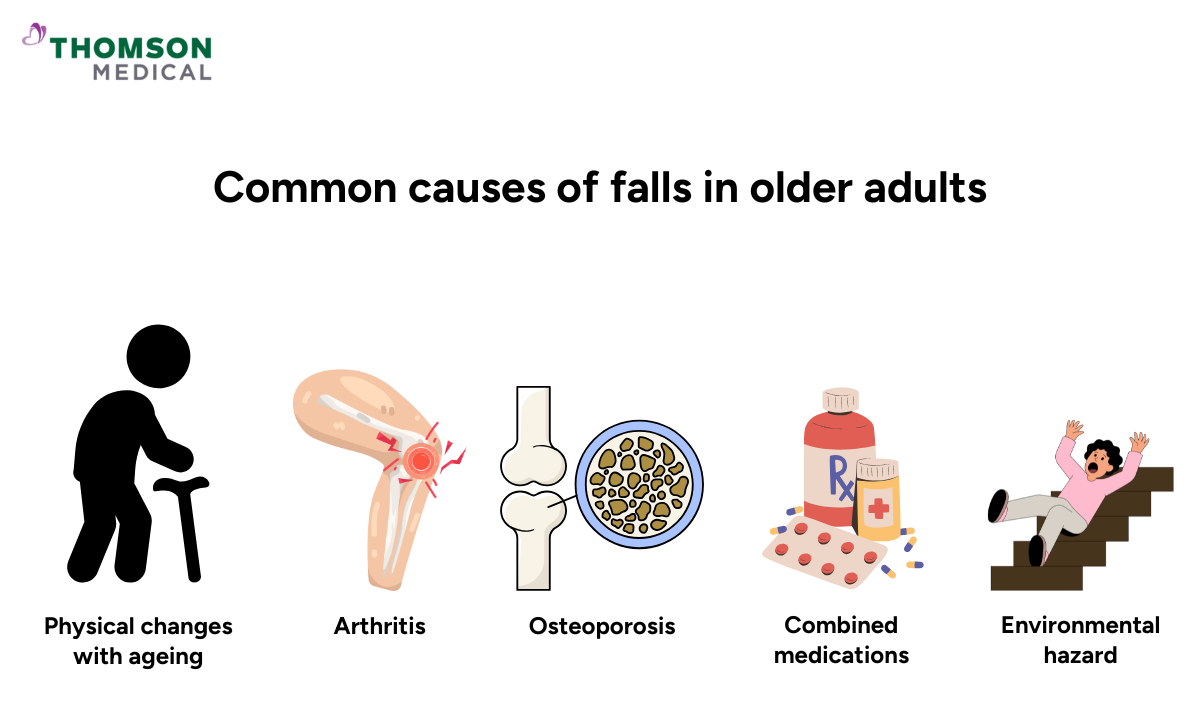
Falls rarely have a single cause. Several factors usually combine to create a situation where balance is lost. Understanding these helps you identify what's most relevant to your situation.
Physical changes with ageing
It can be difficult to watch someone you care about move more slowly or seem less steady on their feet. These changes often happen so gradually that they might not notice them themselves, but they can feel quite significant to those around them:
Reduced muscle strength in the legs and core makes maintaining balance harder
Decreased flexibility limits how quickly they can adjust posture
Vision changes make it difficult to see obstacles or judge distances accurately
Inner ear changes (the vestibular system) affect the body's natural balance mechanism
Slower reaction times mean less opportunity to prevent a fall once balance is lost
Medical conditions that increase risk
Some conditions also make falls more likely, either directly or through the treatments needed to manage them:
Arthritis causes joint pain and stiffness that affect movement
Osteoporosis (brittle bone disease) weakens bones, making fractures more likely if a fall occurs
Diabetes can cause nerve damage that reduces sensation in the feet
Heart conditions may lead to dizziness or fainting
Parkinson's disease and dementia affect coordination and judgement
Low blood pressure can cause light-headedness when standing up
Certain medications increase fall risk, especially when multiple medicines are taken together. Sedatives, blood pressure drugs, pain relievers, and muscle relaxants can all cause dizziness or drowsiness.
Medications
It's quite common for older adults to take several medications each day, sometimes five, six, or more different tablets at various times. Keeping track of what to take when, whilst watching for side effects and potential interactions, can feel genuinely overwhelming. What's important to know is that certain medicines especially when combined can affect balance and alertness in ways you might not immediately connect to fall risk:
Sedatives and sleeping tablets (cause drowsiness)
Blood pressure medicines (may cause dizziness)
Anxiety or depression medications (can affect alertness)
Pain relievers (may reduce coordination)
Muscle relaxants (can cause unsteadiness)
If your loved one takes several medications, it's worth discussing their fall risk with their GP. Sometimes adjustments to timing or dosage can help.
Environmental hazards at home
When someone's mobility starts to change, everyday spaces can suddenly feel less safe. You might walk through your parent's home and suddenly see hazards you never noticed before. These are some of the most common environmental risks worth addressing:
Poor lighting, especially at night
Loose rugs or mats that slip
Cluttered walkways with obstacles
Slippery bathroom surfaces
Uneven flooring or loose floorboards
Stairs without proper handrails
Extension cords running across walking areas
Once you start making these adjustments, you'll likely find yourself feeling more at ease about their safety. That peace of mind - knowing you've taken practical steps to protect someone you care about - is genuinely invaluable.
How to reduce the risk of falls in elderly

Small, thoughtful adjustments can make a real difference. Here's where to start:
Home safety modifications
Walking through a familiar home with safety in mind can feel strange at first, but you might suddenly notice risks that have been there for years. Small changes that seem insignificant can make a real difference in preventing falls. You should focus on:
Improving lighting:
Good lighting makes such a difference, especially for elderly people with poorer eyesight. You can:
Install brighter bulbs throughout the home
Add night lights in bedrooms, hallways, and bathrooms
Ensure light switches are easily accessible at room entrances
Consider motion-sensor lights for convenience
Removing hazards:
You might feel hesitant to suggest changes to a home your loved one has lived in for years, but these adjustments truly help:
Secure or remove loose rugs and mats
Clear walkways of clutter, cables, and obstacles
Repair loose floorboards or uneven surfaces
Ensure carpets are firmly attached to the floor
Bathroom safety
Bathrooms are where many falls happen, often because the surfaces often get wet and slippery. Therefore, these modifications provide important security:
Install grab bars near the toilet and in the shower or bath
Use non-slip mats in the bath or shower
Consider a raised toilet seat if needed
Ensure bathroom items are within easy reach
Stairway safety
Stairs can feel daunting as balance and strength change. These improvements make navigating stairs much safer:
Install sturdy handrails on both sides of the stairs
Ensure stairs are well-lit with switches at top and bottom
Mark the edge of steps with contrasting tape if needed
Keep stairs clear of objects because they can become serious tripping hazards
Health and fitness
While fixing up the home environment matters, maintaining physical health is equally important for staying steady and confident. These health-focused steps complement the safety changes you're making at home:
Encourage activities that build leg strength and improve balance
Walking, tai chi, and swimming are beneficial options
Consider physiotherapy if balance is a concern
Always start new activities gradually, as building strength safely takes time
Vision and hearing checks
Vision and hearing can decline so slowly that people don't notice the change themselves. They might not realise they're compensating until you point it out. Regular checks catch these shifts early:
Arrange regular eye examinations
Ensure glasses prescriptions are up to date
Have hearing checked, as it contributes to balance
Clean glasses regularly for optimal vision
Medication review
When someone takes multiple medications, it's easy for things to become complicated. A regular review with the doctor or GP ensures everything is still working as it should:
Ask the GP to review all medications annually
Discuss whether any medicines might affect balance or alertness
Never stop medications without medical advice
Be aware of timing –- some medicines cause dizziness or other side effects when first taken
Proper footwear
The right shoes make more difference than you might think. Here's what to look for:
Choose shoes with non-slip soles and good support
Avoid walking in socks, stockings, or loose slippers
Ensure shoes fit well without being too tight or loose
Consider specialist footwear if foot problems exist
Assistive devices
Don't hesitate to use aids that improve safety:
Walking aids, sticks or frames provide extra stability
Perching stools allow resting while preparing meals
Reaching aids help access high or low items
Shower chairs reduce the need to stand in slippery conditions
The beauty of these aids is how naturally they fit into daily life, as most people find that just one or two simple additions bring genuine comfort and confidence.
Recognising warning signs that falls may occur
It can feel concerning when you start noticing subtle shifts in how older people move. Perhaps they're holding onto furniture more often, or moving more cautiously than they used to. These gentle changes are often the body's way of asking for a bit more support, and recognising them early gives you the chance to help before things become more challenging.
Changes in walking pattern
If you've been spending time with or caring for an elderly loved one, you may start to notice subtle shifts in the way they move. When something changes, you often notice it before they do. These subtle shifts in how they walk can be early warning signs:
Walking more slowly or cautiously than usual
Shuffling feet rather than lifting them
Using walls or furniture for support while walking
Appearing unsteady or swaying
Holding onto objects tightly for balance
Difficulty with daily activities
When older adults start struggling with tasks they've done independently for years, it can be difficult to witness. These changes often happen gradually, but they're important signals that additional support may be needed:
Getting up from a chair or bed
Reaching for items on high shelves
Bending down to pick things up
Climbing stairs
Getting in and out of the bath or shower
Fear of falling and previous falls
Many older adults quietly develop a fear of falling, even if they haven't fallen yet. This anxiety often leads them to limit their activities, which ironically weakens their muscles and balance, making falls more likely. If you've noticed they're doing less or seem more hesitant, it's worth discussing with your doctor.
For anyone who has fallen once is at higher risk of falling again. Even a minor fall should prompt a review of safety measures and potential health issues. Think of it as an opportunity to review safety measures and wellbeing, not because something is inevitably wrong, but as a caring precaution to support continued independence.
Health risks associated with falls
No one wants to dwell on worst-case scenarios, but knowing what's at stake is important. Here's what falls can lead to:
Physical injuries
The injuries from a fall can vary widely from minor bruising to something more serious. Often, the fear of what might happen weighs as heavily as the physical hurt. Here are the injuries that concern families most:
Hip fractures:
Particularly serious and often require surgery and extended rehabilitation
Head injuries:
This can range from minor bumps to severe trauma requiring immediate care
Broken wrists or arms:
From trying to break the fall
Cuts and bruises:
These might heal slowly in older adults
Soft tissue injuries:
Including sprains and strains
Loss of confidence and independence
Sometimes what lingers after a fall isn't the bruise or the ache – it's the fear. You might notice they seem more hesitant or withdrawn, even after their body has healed. This emotional impact is just as real as any physical injury:
Increased fear of falling again
Reduced participation in activities they once enjoyed
Social isolation as they avoid going out
Decreased physical fitness from reduced activity
Loss of independence requiring more assistance with daily tasks
Long-term health decline
For some older adults, a serious fall changes everything. What once took days to bounce back from can now take months, and even after they recover, they may not fully return to their previous independence.
We understand this can feel worrying, but it's important to recognise that small, consistent preventive steps today can make a meaningful difference in maintaining your loved one's mobility and confidence as they age.
What happens after a fall?
If someone has fallen, knowing what to do can help you feel more in control of a scary situation:
Immediate response
Whether you witness the fall or find them on the floor afterwards, the moment can be frightening. Taking a breath and staying as calm as possible helps you both get through it. Here are some actions you should take:
Stay calm and reassure them
Check for injuries before helping them move
Don't rush to help them up –- ensure they're not seriously hurt first
Call for help if you cannot safely assist them or if they're injured
If not injured, help them roll onto their side, rest, then get onto hands and knees
Use a sturdy chair for support as they gradually stand up
Sit them down and monitor them for delayed symptoms
Follow-up actions
Once the immediate situation is handled and your loved one is safe, there are a few important steps to take:
Document what happened, including time, location, and circumstances
Notify their GP, even if there's no apparent injury
Review what caused the fall and make necessary changes
Monitor for delayed symptoms such as pain, bruising, or confusion
Consider arranging a professional falls risk assessment
Going through these steps shows you're taking the situation seriously, and that matters. Even if the fall seemed minor, your diligence could prevent something more serious down the line.
When to seek urgent medical care
In the moments after a fall, it can be hard to know whether you're overreacting or not taking things seriously enough. When it comes to these symptoms, it's always better to err on the side of caution. Contact emergency services or go to A&E immediately if they:
Immediate emergency signs
Trust your instincts – if something feels seriously wrong after a fall, it probably is. In these situations, don't hesitate to call emergency services or go straight to A&E:
Has hit their head, particularly if taking blood-thinning medication
Is unconscious or has lost consciousness, even briefly
Is confused, drowsy, or difficult to wake
Has severe pain, especially in the hip, back, or head
Cannot get up or move a limb
Has visible deformity of an arm or leg suggesting a break
Has bleeding that won't stop
Has difficulty breathing
Shows signs of shock (pale, cold, rapid pulse)
Serious symptoms requiring prompt medical review
Some injuries fall into a grey area, not quite an emergency, but worrying enough that you shouldn't just wait and see. It's worth getting these checked promptly:
Has ongoing pain that limits movement
Develops swelling, bruising, or tenderness over the following hours
Cannot bear weight on a leg
Has reduced range of motion in a joint
Experiences dizziness or ongoing balance problems
Has fallen multiple times recently
Shows signs of dehydration or inability to care for themselves
FAQ
How common are falls in older adults?
Falls are very common among people over 65. The frequency increases with age and certain health conditions. However, falls are not an inevitable part of ageing, and many can be prevented with appropriate measures.
Can all falls be prevented?
While not every fall can be prevented, the risk can be significantly reduced. Many falls result from modifiable factors such as home hazards, medication side effects, or muscle weakness. Addressing these factors proactively helps protect your loved one's safety and independence.
Should I be worried if my loved one falls but isn't hurt?
Yes, any fall warrants attention. Even falls without injury indicate increased risk for future falls. It's important to identify why the fall occurred and make changes to prevent recurrence. Contact the GP to arrange a falls assessment.
Do certain times of day carry a higher fall risk?
Yes, falls in older people are more common during transitions, such as getting up at night to use the bathroom. This is when people may be drowsy, the lighting is poor, and blood pressure may drop upon standing. Installing night lights and allowing time to adjust before walking can help.
What if my loved one lives alone?
Extra precautions are warranted for the elderly living alone. Consider a personal alarm system they can wear that connects to emergency services. Regular check-ins, home safety modifications, and maintaining social connections all contribute to safety. However, living alone doesn't mean they can't be safe – many older adults manage very well with appropriate support.
What are the consequences of falls in the elderly?
Falls can lead to:
-
Physical injuries: fractures (especially hips), head trauma, cuts, and bruising
-
Emotional impact: fear of falling again, loss of confidence, and avoiding activities
-
Cycle of decline: reduced activity leads to weaker muscles, which increases fall risk further
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Medical 24-Hour Urgent Care Centre (Novena)
- Call: 6350 8812
Notice:
The range of services, vaccinations, and tests may vary. Please contact us directly to enquire about the current availability.
Request an Appointment

