Reading an MRI scan can feel overwhelming and difficult, but it doesn’t have to be. This step-by-step guide will help you understand what to look for, from subtle signals to clear signs of injury, so you can feel more informed and confident about your diagnosis.
What is a meniscus tear?
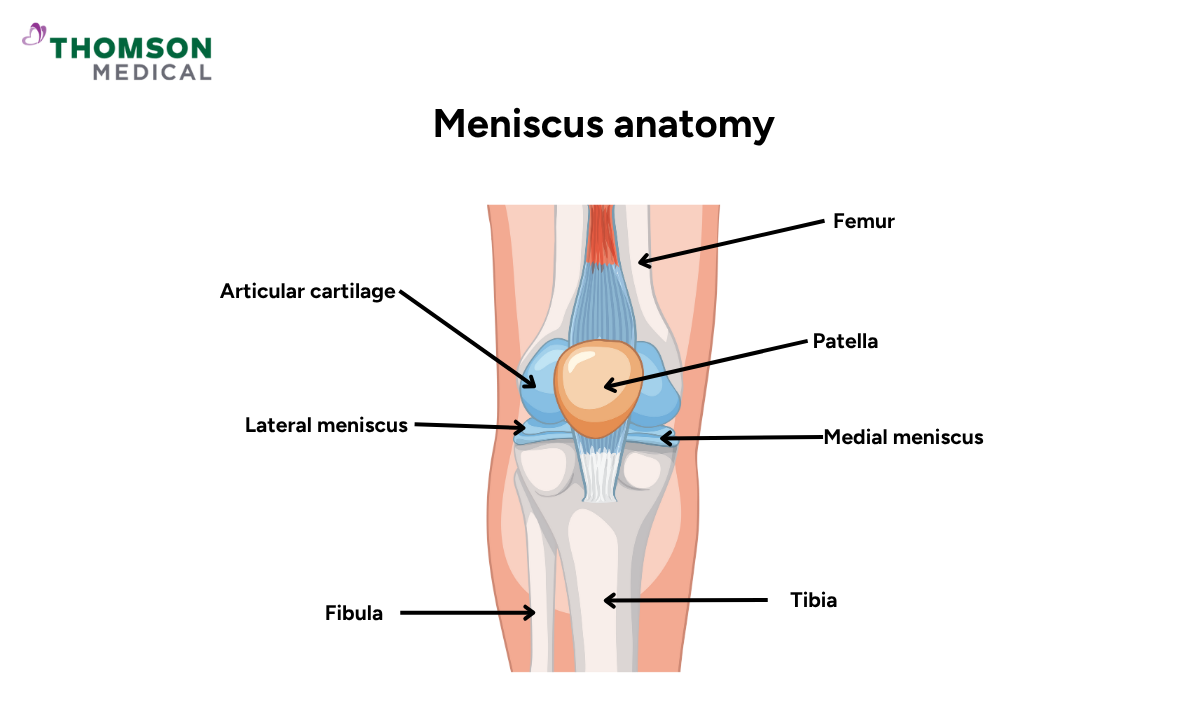
A meniscus tear is a common knee injury affecting the cartilage that cushions your joint. The menisci are two C-shaped pads of tough, rubbery cartilage situated between the thighbone (femur) and shinbone (tibia). Known as the medial and lateral meniscus, they act as shock absorbers and help stabilise the knee whenever you move.
Meniscal tears can occur suddenly from trauma, such as twisting the knee during sports or heavy lifting, or develop gradually due to age-related degeneration and cartilage wear. This injury often causes pain, swelling, stiffness and difficulty moving your knees.
How is an MRI used for detecting meniscus tears?
An MRI (magnetic resonance imaging) is a highly effective, non-invasive method for diagnosing meniscus tears in the knee. This advanced imaging technique creates detailed cross-sectional images of the knee’s internal structures by using powerful magnetic fields and radio waves.
MRI scans for meniscus tears are particularly valuable because they can:
-
Detect subtle or complex meniscus tears that are not visible on standard X-rays
-
Differentiate between various types of tears, such as horizontal, radial or bucket-handle tears
-
Reveal additional knee injuries, including ligament damage, cartilage wear or bone bruising
By providing clear, precise images, an MRI allows healthcare professionals to accurately assess the extent of a meniscus injury and plan the most appropriate treatment.
How to know if you need an MRI for a meniscus tear?
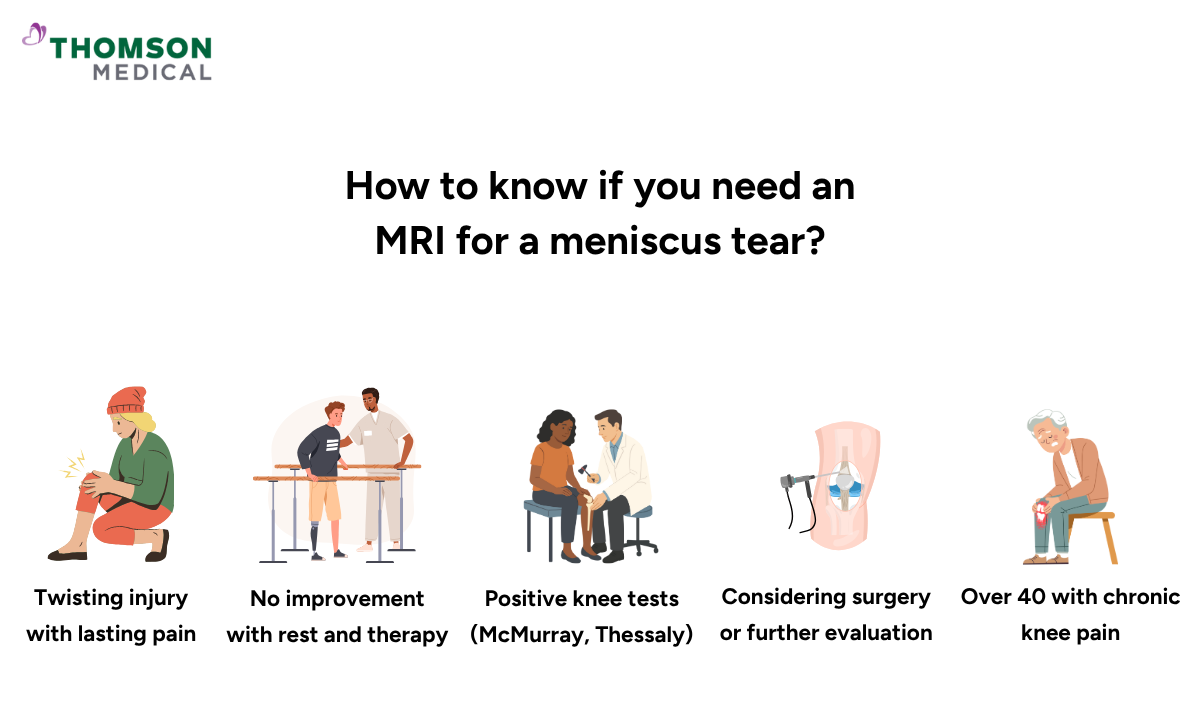
An MRI is most helpful when your symptoms are unclear or when a detailed view of the knee joint is needed to guide treatment decisions.
You may need an MRI if:
-
You have had a twisting knee injury and continue to experience pain, swelling or a feeling of instability
-
Physical examination findings (such as a positive McMurray or Thessaly test) suggest a possible meniscus tear
-
Conservative treatment, including rest, ice and physiotherapy, has not improved your symptoms
-
You are considering surgical repair or further assessment for persistent knee problems
-
You are over 40 and have chronic knee pain, where distinguishing between arthritis and a meniscus tear is important
If you’re experiencing persistent knee pain or are unsure about your symptoms, request an appointment with our orthopaedic specialist to discuss whether an MRI is right for you.
How to identify a meniscus tear on MRI?
Radiologists assess MRI images by examining multiple angles of the knee, including sagittal, coronal and axial views. A normal meniscus appears as a dark, triangular structure on the scan. A tear is usually indicated by:
-
A bright signal (white line) that extends to the surface of the meniscus
-
Disruption or distortion of the normal triangular shape
-
Gaps, fragmentation or displacement of the meniscus
-
Secondary signs, such as joint effusion (fluid build-up) or bone oedema
If you suspect a meniscus tear, request an appointment with our orthopaedic specialist to review your MRI and discuss your treatment options.
How to read different types of meniscus tears on MRI
There are several types of meniscus tears, each with distinct MRI characteristics:
-
Horizontal tear:
-
Appears as a horizontal white line splitting the meniscus in half
-
Common in degenerative tears, especially in older adults
-
-
Vertical (longitudinal) tear:
-
Appears as a vertical line running perpendicular to the tibial surface
-
May progress to a bucket-handle tear over time
-
-
Radial tear:
-
Short tear extending from the inner edge outward
-
Disrupts the ring-like shape of the meniscus and can be difficult to see
-
-
Complex tear:
-
Combination of two or more tear patterns
-
Often seen in severe or chronic injuries
-
-
Bucket-handle tear:
-
A displaced longitudinal tear creating a central fragment
-
Often leads to locking or restricted movement of the knee
-
FAQ
How do I tell what grade my meniscus tear is?
Meniscus tears on MRI are often graded by how far the bright signal extends into the knee cartilage:
-
Grade 1:
-
A small, round bright spot within the meniscus that does not reach the surface. Usually not a true tear.
-
-
Grade 2:
-
A linear bright area that still does not contact the surface. Often seen in degeneration.
-
-
Grade 3:
-
A bright line extending to at least one surface of the meniscus. This is a true tear.
-
Your radiology report should state the grade and describe the tear pattern. If you’re unsure, you should ask your doctor or radiologist to explain the findings in detail and how they relate to your symptoms.
Is reading a meniscus tear on MRI difficult?
Yes, interpreting a meniscus tear on MRI can be challenging, even for experienced radiologists. Although MRI provides highly detailed images of the knee’s soft tissues, subtle tears, such as small radial tears or root tears, can be difficult to spot. Accurate interpretation requires a thorough understanding of knee anatomy, careful assessment in multiple viewing planes and the ability to distinguish normal age-related changes from true injury. For this reason, MRI scans are usually reviewed by musculoskeletal radiologists who specialise in identifying meniscus tears and related problems.
What are the most common mistakes in reading MRI for meniscus tears?
Some common pitfalls include:
-
Mistaking normal variants, such as meniscal flounce or blood vessels in children, for tears
-
Missing small or complex tears that don’t show obvious signal changes
-
Overcalling tears in degenerated menisci with increased signal but no surface disruption
-
Ignoring associated injuries like ACL tears or bone bruises that affect treatment decisions
Accurate diagnosis always requires combining MRI findings with the patient’s history and physical examination.
What do bright white spots on a knee MRI mean?
Bright white spots on a knee MRI usually indicate areas where there is increased fluid or changes in the tissue. In the meniscus, a bright line or spot can suggest a tear if it reaches the surface of the cartilage. Other causes of bright signals include inflammation, joint effusion (fluid build-up), bone bruising or degenerative changes.
What level of meniscus tear requires surgery?
Not all meniscus tears need surgery. Surgery is often considered if:
-
The tear causes the knee to lock or catch (such as a bucket-handle tear)
-
You have persistent pain or swelling despite physiotherapy and rest
-
The tear is large, unstable or in an area with poor blood supply (which limits healing)
-
The tear is associated with other injuries, such as an ACL tear
Small, stable tears—especially in the outer edge of the meniscus—may heal without an operation. Your doctor will recommend appropriate treatment based on the type of tear, symptoms, and activity level.
Can all types of meniscus tears be seen on MRI?
Most meniscus tears can be seen on a high-quality MRI, but not all are easy to detect. Some factors that may limit detection include:
-
Small or incomplete tears that don’t show a clear signal
-
Poor image quality due to movement or artefact
-
Advanced degeneration, which makes the tissue look irregular
-
Post-surgical changes that can obscure the anatomy
If symptoms persist despite a normal MRI, further evaluation by a specialist may be needed.
How reliable is MRI compared to other diagnostic methods for detecting meniscus tears?
MRI is considered the most accurate non-invasive test for diagnosing meniscus tears. It has a sensitivity of about 85–95% and a specificity of 85–90% for detecting significant tears. MRI offers detailed images of soft tissues without radiation, making it the preferred first-line imaging method.
Compared to other techniques:
-
X-rays:
-
Cannot show soft tissue injuries like meniscus tears
-
-
Ultrasound:
-
Limited in assessing deep structures inside the knee
-
-
Arthroscopy:
-
The gold standard for diagnosis but invasive and mainly used when surgery is planned
-
If MRI results are unclear but symptoms persist, your doctor may recommend further assessment or arthroscopy.
What should I expect after an MRI diagnosis?
After an MRI confirms a meniscus tear, your healthcare provider will explain the type, size and location of the tear and recommend the most suitable treatment. Options may include:
-
Conservative care:
-
Rest, physiotherapy and anti-inflammatory medicines
-
-
Activity modifications:
-
Avoiding movements that worsen symptoms
-
-
Injections:
-
Such as corticosteroids to reduce inflammation
-
-
Surgical intervention:
-
Often advised for large, displaced or persistent tears
-
Your treatment plan will depend on your age, activity level, tear pattern and overall knee health.
What are the pros and cons of MRI for meniscus tear diagnosis?
Pros:
-
Non-invasive and painless
-
Provides highly detailed images of cartilage, ligaments and bone
-
No radiation exposure
-
Can detect other knee injuries at the same time
Cons:
-
May miss very small or degenerative tears
-
Can be misinterpreted without proper clinical context
-
Not suitable for some patients with metal implants or devices
-
More expensive and less accessible than X-rays
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
