If you have been advised to consider a hysterectomy, the thought of having your womb removed can be frightening. Knowing what the surgery involves, why it is recommended, and what to expect during recovery can help you feel more prepared going into the process.
What is a hysterectomy?
A hysterectomy is a surgical procedure to remove the uterus (womb). This procedure is often performed to treat conditions such as fibroids, endometriosis, abnormal bleeding, or certain cancers when other treatments have been unsuccessful.
Hysterectomy is one of the most common gynaecological surgeries. It can be performed through open surgery or using minimally invasive techniques.
After a hysterectomy, menstrual periods stop permanently, and pregnancy is no longer possible. In some cases, other reproductive organs – such as the cervix, ovaries, or fallopian tubes – may also be removed, depending on your condition and treatment plan.
Types of hysterectomy
There isn’t just one kind of hysterectomy. The type recommended for you depends on your medical condition, age, and treatment goals.
Total hysterectomy:
Removal of your entire uterus and cervix
This is the most commonly performed type
The ovaries may or may not be removed, depending on your condition
Partial (subtotal) hysterectomy:
Removal of your uterus while leaving the cervix in place
Less commonly performed today
If the cervix remains, regular cervical screening is still required
Radical hysterectomy:
Removal of your uterus, cervix, part of the upper vagina, and nearby tissues
Usually recommended for certain gynaecological cancers
May include removal of nearby lymph nodes as part of cancer treatment
Hysterectomy with oophorectomy:
Removal of your uterus together with one or both ovaries
May be recommended to treat ovarian conditions or reduce cancer risk
If both ovaries are removed, this leads to surgical menopause, which your doctor will discuss with you in detail beforehand
Why might a hysterectomy be recommended?
A hysterectomy may be considered if you have:
- Severe or persistent uterine fibroids
Endometriosis or adenomyosis that has not improved with other treatments
Heavy or abnormal uterine bleeding
Cervical, ovarian, or uterine cancer
Uterine prolapse (when the uterus drops from its normal position)
Chronic pelvic pain that has not responded to other therapies
In most cases, a hysterectomy is recommended only after more conservative treatment options have been explored – especially if preserving fertility is important to you.
Your doctor will discuss the benefits, risks, and alternatives to help you make an informed decision for your situation.
If you're experiencing any of these symptoms, schedule an appointment with our obstetrician and gynaecologists (O&G) at Thomson Women's Clinic. They'll assess your situation and outline personalised options, including whether hysterectomy is appropriate for you.
Our hysterectomy surgeon in Singapore
Loading...
How do you prepare for a hysterectomy?
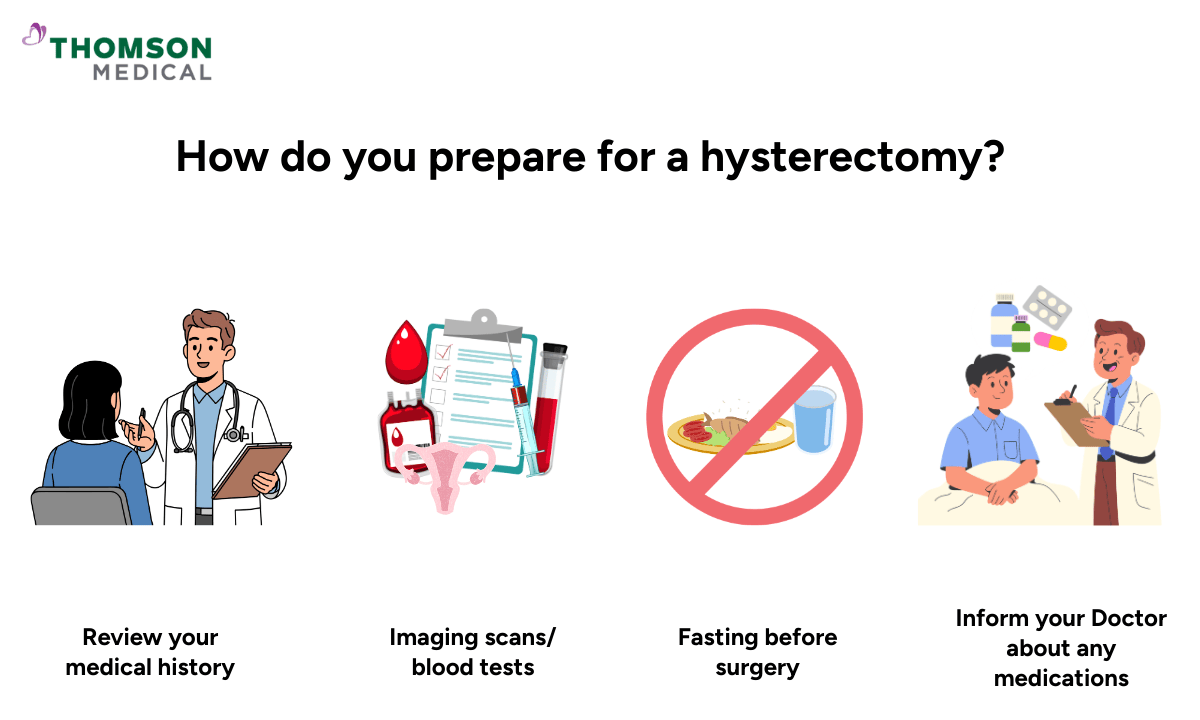
Before surgery, your doctor will review your medical history and may arrange blood tests or imaging scans to ensure the procedure is safe for you.
Once your operation is scheduled, you will receive instructions on how to prepare. In most cases, this includes fasting for several hours before surgery.
It is important to inform your doctor about any medications, vitamins, or herbal supplements you are taking. Some medicines – particularly blood thinners – may need to be adjusted or stopped temporarily.
You may also be advised to arrange help at home for the first few days after surgery.
What can you expect during a hysterectomy surgery?
A hysterectomy is usually performed under general anaesthesia, which means you will be asleep during the procedure.
During the surgery
The type of hysterectomy and surgical approach will depend on your condition. It may be performed:
Through an incision in the abdomen (abdominal hysterectomy)
Through the vagina (vaginal hysterectomy)
Using minimally invasive techniques such as laparoscopy
The procedure typically takes one to three hours, depending on the complexity of the surgery and whether additional organs, such as the ovaries or fallopian tubes, need to be removed.
After the surgery
You may stay in the hospital for a few days, depending on the type of surgery performed and your overall health.
It is normal to experience some pain or discomfort after the procedure. This will be managed with medication.
You will be encouraged to start moving gently as soon as it is safe to do so, as this helps prevent blood clots and supports recovery.
Your healthcare team will provide detailed instructions about wound care, activity levels, and follow-up appointments before you go home.
What are the risks and complications of a hysterectomy?
A hysterectomy is a commonly performed and generally safe procedure. However, like all major surgeries, it carries some potential risks. Your doctor will assess your individual health factors and take steps to reduce these risks as much as possible.
Common surgical risks may include:
Bleeding during or after surgery
Infection
Pain or discomfort around the surgical site
Blood clots in the legs or lungs
Reactions to anaesthesia
Less common but more serious complications include:
Injury to nearby organs such as the bladder, ureters, or bowel
Urinary difficulties
Wound healing problems
Rare separation of the vaginal incision (vaginal cuff complications)
Conversion from minimally invasive surgery to open surgery if needed for safety
If both ovaries are removed, you will experience surgical menopause, which may cause symptoms such as hot flushes, mood changes, or vaginal dryness.
Most women recover without serious complications. Your doctor will explain warning signs to watch for and provide clear guidance on recovery.
Recovery after a hysterectomy
Recovery period depends on the type of surgery performed.
Abdominal hysterectomy might takes approximately 6-8 weeks
Vaginal or laparoscopic hysterectomy takes approximately 3-4 weeks
While external healing occurs within weeks, full internal recovery may take longer.
What to expect during recovery
You may experience light abnormal vaginal bleeding or discharge for several weeks after surgery. Using sanitary pads (not tampons) is recommended during this time.
To support healing:
Get plenty of rest, while taking short walks daily to improve circulation
Avoid heavy lifting and strenuous activity for at least 6 weeks
Do not insert anything into the vagina (including tampons or douches) until your doctor advises it is safe
Avoid sexual intercourse for about 6 weeks, or as recommended
Take prescribed medications as directed
Your doctor will provide personalised guidance based on your surgery type and overall health.
Cost of hysterectomy surgery in Singapore
The cost of a hysterectomy in Singapore varies depending on the type of procedure, hospital, and complexity of your case.
You can expect these procedures to range from around SGD 25,800 to SGD 53,300, or more, depending on the surgical approach and other factors.
For a detailed cost breakdown, you may refer to our hysterectomy surgery cost in Singapore article.
What affects the cost?
Several factors influence how much you may pay:
Type of hysterectomy (open, vaginal, or laparoscopic)
Length of hospital stay
Surgeon and anaesthetist fees
Ward class (e.g., subsidised vs private)
Additional procedures such as ovary removal or lymph node dissection
Pre- and post-surgery consultations and tests
Insurance and savings support
Singapore residents may be able to use MediSave, MediShield Life, and Integrated Shield Plans to help cover part of the costs. Coverage varies by plan, procedure, and eligibility, so it’s best to check with your insurer and healthcare team.
Please note that insurance panel coverage may vary by doctor. To confirm whether your preferred doctor is on your insurance panel and check your eligibility, schedule an appointment with the doctor directly. If you require further information about insurance availability or claims processing, contact our medical concierge for assistance.
FAQ
How long does hysterectomy surgery take?
Most hysterectomy procedures take about 1 to 3 hours, depending on the surgical approach and the complexity of the case.
Is hysterectomy surgery painful?
While some discomfort is to be expected after surgery, the pain can generally be managed effectively with medication. Minimally invasive procedures generally cause less postoperative pain compared to open surgery.
Can I get pregnant after a hysterectomy?
No. Once the uterus is removed, pregnancy is no longer possible.
What alternatives are there to a hysterectomy?
Alternatives depend on the underlying condition. Options may include medications, lifestyle adjustments, uterine artery embolisation for fibroids, endometrial ablation for heavy bleeding, or minimally invasive surgery to remove fibroids or endometrial tissue.
Your doctor will discuss all available options to help you choose the most appropriate treatment for your situation.
Can you still have menstrual symptoms after a hysterectomy?
After a total hysterectomy (removal of the uterus and cervix), menstrual periods stop completely.
If you have a partial (subtotal) hysterectomy, where the cervix is left in place, some women may experience light cyclical spotting. This happens because a small amount of endometrial tissue can remain in the cervical canal.
If your ovaries are preserved, you may still experience hormonal symptoms around the time your period would have occurred, such as:
Bloating
Breast tenderness
Mood changes
However, you will not have menstrual bleeding once the uterus has been removed.
Do ovaries still ovulate after a hysterectomy?
Yes. If one or both ovaries are preserved, they can continue to function normally and produce hormones until natural menopause occurs.
Although ovulation may still occur, pregnancy is not possible because the uterus has been removed.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, schedule an appointment with Thomson Women’s Clinic today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
