Singapore has one of Asia's most advanced fertility treatment systems, with multiple assisted reproductive technologies (ART) providing solutions to help you achieve pregnancy.
Among the most common fertility treatments are intracytoplasmic sperm injection (ICSI) and intrauterine insemination (IUI). While both procedures aim to enhance the chances of conception, they differ in their approach, cost, success rates, and suitability for different fertility issues.
Understanding these distinctions is crucial for making an informed decision about the best treatment option for your unique circumstances. Whether you're just beginning your fertility journey or considering the next steps, having the right information empowers you to make the best choice in consultation with your healthcare provider.
What is ICSI?

Intracytoplasmic sperm injection (ICSI) is an advanced form of in vitro fertilisation (IVF) that involves the direct injection of a single sperm into an egg to achieve fertilisation. Think of it this way: while regular IVF puts sperm and eggs together in a dish and lets them find each other naturally, ICSI is more like a matchmaker who directly introduces them. This technique is particularly beneficial for cases of severe male infertility, where natural fertilisation may be challenging.
ICSI takes place in a laboratory setting, where embryologists select a healthy sperm and inject it into a mature egg using a fine needle. The fertilised egg is then monitored and, if viable, transferred into the woman’s uterus to establish pregnancy.
Who is ICSI suitable for?
ICSI is often recommended for couples experiencing:
Severe male infertility, including low sperm count, poor motility, or abnormal morphology.
Previous failed IVF cycles due to poor fertilisation.
Unexplained infertility where conventional methods have not worked.
Situations requiring sperm retrieval through surgical procedures due to medical conditions like azoospermia (absence of sperm in ejaculate).
How does the ICSI process work?
The ICSI procedure follows several key steps:
Ovarian stimulation:
The woman undergoes hormone treatments to stimulate the production of multiple eggs.
Egg retrieval:
Mature eggs are collected from the ovaries through a minor surgical procedure.
Sperm selection:
A single, healthy sperm is chosen and injected directly into an egg using a fine microneedle.
Embryo monitoring:
The fertilised egg is monitored in the lab for several days to ensure normal development.
Embryo transfer:
A viable embryo is transferred into the uterus, where it may implant and lead to pregnancy.
Pregnancy test:
About two weeks after the procedure, a test determines whether implantation has occurred.
What is IUI?
Intrauterine insemination (IUI), also known as artificial insemination, is a fertility treatment that enhances the chances of conception by directly placing sperm into the uterus. This method helps bypass certain fertility barriers, such as cervical mucus issues or mild male infertility, allowing sperm to reach the egg more efficiently. It's like showing them a shortcut to their destination instead of making them find their own way. The sperm still need to swim to the egg and fertilise it naturally, but they have less distance to travel.
Unlike IVF or ICSI, IUI does not involve egg retrieval or fertilisation outside the body. Instead, it relies on natural fertilisation in the reproductive system. Because of its simplicity and cost-effectiveness, IUI is often the first fertility treatment recommended before moving to more advanced methods like IVF or ICSI.
Who is IUI suitable for?
IUI is a good option for:
Couples experiencing mild male infertility, such as low sperm count or motility issues.
Women with ovulatory disorders or irregular menstrual cycles.
Unexplained infertility where no specific cause has been identified.
Women with cervical issues that may prevent sperm from passing through.
Couples who prefer a less invasive and more affordable fertility treatment before considering IVF.
How does the IUI process work?
IUI is a relatively simple and quick procedure, usually involving these steps:
Ovulation tracking:
A fertility specialist monitors the woman’s ovulation cycle using ultrasound scans or hormone tests to determine the optimal time for insemination.
Sperm collection and preparation:
A sperm sample is collected from the male partner or donor. The sample is then “washed” in a laboratory to concentrate the healthiest and most motile sperm.
Sperm insertion:
The prepared sperm is inserted directly into the uterus using a thin, flexible catheter. This bypasses the cervix and increases the chances of sperm reaching the fallopian tubes.
Post-procedure rest:
The woman rests briefly after the procedure, but no recovery time is needed.
Waiting period and pregnancy test:
About two weeks later, a pregnancy test is conducted to determine if the treatment was successful.
Key differences between ICSI and IUI
When exploring fertility treatments, it’s essential to understand the differences between ICSI and IUI. While both procedures aim to help couples conceive, they vary in terms of complexity, cost, and suitability for different fertility issues.
Feature | ICSI (intracytoplasmic sperm injection) | IUI (intrauterine insemination) |
Procedure type | Part of IVF, requires laboratory fertilisation | Performed inside the uterus with natural fertilisation, a more simple procedure |
Invasiveness | Performed inside the uterus with natural fertilisation | Minimally invasive (catheter insertion) |
Success rates | Higher, around 50–80% per cycle (fertilisation success) | Lower, 10–20% per cycle |
Ideal for male infertility | Yes, can overcome severe sperm issues | Only for mild sperm issues |
Cost | Expensive due to lab work | More affordable |
Hormonal medication | Required | May or may not be needed |
Number of cycles required | Usually fewer due to high success rates | Multiple cycles may be needed |
For individuals seeking fertility assessment and treatment options, Thomson Medical Centre's fertility services provide comprehensive reproductive healthcare consultations.
ICSI vs IUI: Which one should you choose?
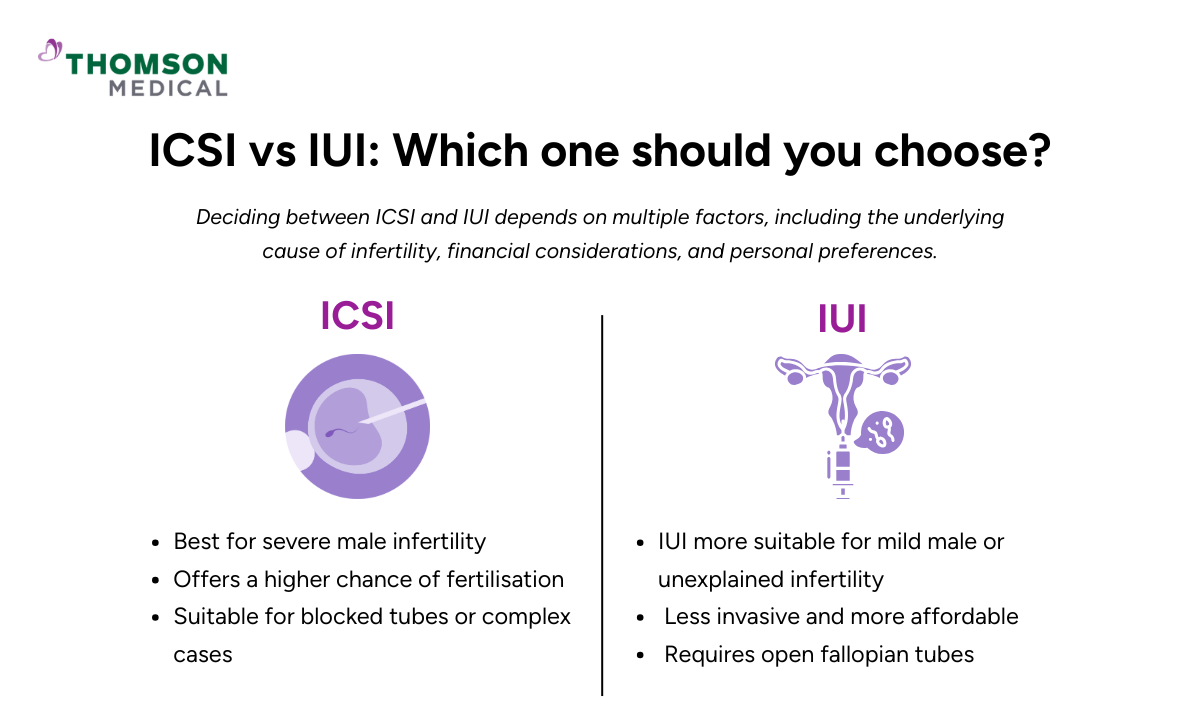
Deciding between ICSI and IUI depends on multiple factors, including the underlying cause of infertility, financial considerations, and personal preferences.
ICSI is best for severe male infertility, especially when sperm quality or count is extremely low. It offers a higher chance of fertilisation because it directly injects sperm into the egg, making it ideal for couples who have had unsuccessful IVF attempts or sperm-related fertility issues.
IUI is more suitable for mild male infertility, unexplained infertility, or cervical mucus problems. It is a less invasive and more affordable option, making it a preferred first step for many couples trying to conceive naturally.
IUI requires open and functioning fallopian tubes, whereas ICSI is performed outside the body, making it a better choice for cases involving blocked tubes or other severe fertility issues.
If a woman has ovulatory disorders, IUI can be combined with ovulation-stimulating medication to improve success rates. However, if multiple IUI cycles are unsuccessful, transitioning to ICSI or IVF may be recommended.
Both ICSI and IUI provide valuable fertility treatment options, but they serve different needs. ICSI is highly effective for severe male infertility or complex cases, while IUI is a simpler, cost-effective option for mild fertility concerns.
If you are uncertain about fertility treatment options, a consultation with a fertility specialist can help determine suitable approaches based on clinical evaluation. Request an appointment with us to review your medical history and provide a clinical evaluation to determine the most suitable treatment options for you.
FAQ
Is ICSI more successful than IUI?
Yes, ICSI is generally more successful than IUI, especially for cases involving severe male infertility. ICSI success rates range from 50–80% per cycle (fertilisation success), whereas IUI success rates are lower, around 10–20% per cycle.
What is the downside of ICSI?
The downsides of ICSI include:
Higher cost compared to IUI and conventional IVF.
More invasive procedure requiring egg retrieval and lab fertilisation.
Increased risk of multiple births if multiple embryos are transferred.
Potential genetic risks may arise as weaker sperm that may not fertilise naturally are used.
No guarantee of success, especially in cases of poor egg quality.
Does ICSI pick the best sperm?
ICSI involves manual sperm selection, where an embryologist chooses a single sperm based on its movement and shape before injecting it into an egg. However, ICSI does not guarantee the selection of the "best" sperm genetically, as it mainly relies on visible characteristics rather than advanced genetic screening. Techniques like intracytoplasmic morphologically selected sperm injection (IMSI) or genetic testing can help select higher-quality sperm.
Is ICSI painful for females?
ICSI itself is not painful for females since the sperm injection happens in a lab. However, the egg retrieval process, which is part of IVF, can cause mild to moderate discomfort. It is typically performed under sedation or anaesthesia, so pain is minimal during the procedure. Afterwards, some women may experience cramping, bloating, or mild soreness, which usually subsides within a few days.
Can you get pregnant naturally after IUI?
Yes, it is possible to get pregnant naturally after IUI. Some women conceive naturally in later cycles, especially if IUI helps improve fertility factors such as sperm placement, hormonal balance, or ovulation timing. However, the chance of pregnancy depends on the underlying fertility challenges. If IUI is unsuccessful after multiple attempts, a fertility specialist may recommend IVF or other treatments.
Can ICSI sperm be used for IUI?
No, ICSI sperm cannot be used for IUI. In ICSI, sperm is individually selected and directly injected into an egg in a lab, while IUI requires a high number of motile sperm to be placed in the uterus for natural fertilisation. Sperm used for ICSI is typically from men with severe male infertility, where sperm count or motility is too low for IUI to be effective.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
Dr Ryan Lee Wai Kheong
Obstetrics & Gynaecology (O&G)
Thomson Specialists Woodleigh (Women's Health)
English, Mandarin
Prudential, Great Eastern, Adept, MHC and 4 others

