What is knee osteoarthritis?
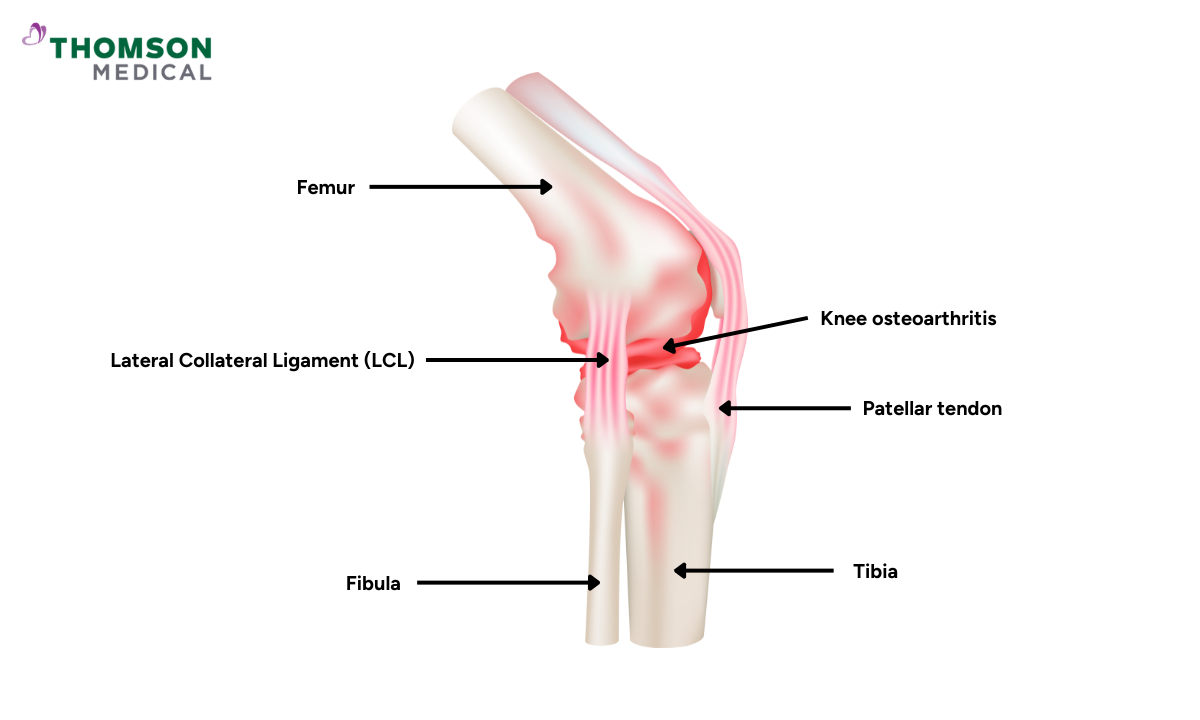
Knee osteoarthritis is a degenerative joint disease that affects the cartilage, bones, and surrounding tissues in your knees. It is the most common type of arthritis and is caused by the protective cartilage that cushions the ends of the bones being worn down over time.
This condition can lead to pain, stiffness, and reduced mobility, making daily activities difficult. Your other joints, like wrists and elbows, can also get osteoarthritis, but the knee is especially susceptible due to the weight and stress placed on it during everyday life.
While there is no cure for knee osteoarthritis, various treatments can manage symptoms and improve quality of life.
Causes of knee osteoarthritis
Biological changes, wear and tear, and injuries are the main causes of knee osteoarthritis.
Ageing
As we age, the cartilage that cushions the joints breaks down, leading to knee osteoarthritis.
Overuse and wear
Years of repeated stress on the knee joint can cause cartilage to wear out, which is common in athletes or those who do physically demanding jobs.
Injury
Knee injuries such as fractures or ligament tears can lead to the development of knee osteoarthritis later in life.
Obesity
Excess weight puts additional stress on the knee joints, increasing the risk of cartilage degeneration.
Genetics
Some people have a genetic predisposition to osteoarthritis, meaning it may run in families.
Gender
Women, particularly those over the age of 50, are more likely to develop knee osteoarthritis than men.
Inflammation
Chronic low-level inflammation can contribute to the breakdown of cartilage.
Biomechanical factors
Poor alignment of the knee or leg bones can cause uneven stress on the knee joint, leading to osteoarthritis.
Symptoms of knee osteoarthritis
The symptoms of knee osteoarthritis typically develop gradually and worsen over time. The most common symptoms include:
Pain
Feeling pain in the knee during or after movement, which is often worsened by activity and relieved by rest.
Stiffness
Knee stiffness, particularly in the morning or after periods of inactivity, makes it difficult to move the joint.
Swelling
The knee may become swollen due to inflammation in the joint or the buildup of fluid (effusion).
Decreased range of motion
As the cartilage wears away, it becomes harder to fully bend or straighten the knee.
Grinding or cracking sensation
You may feel or hear a grinding, clicking, or popping sensation (crepitus) when moving the knee.
Joint deformity
In advanced stages, knee osteoarthritis can lead to visible deformities, such as a bowlegged (varus) or knock-kneed (valgus) appearance.
Diagnosis of knee osteoarthritis
Diagnosing knee osteoarthritis involves a combination of clinical evaluation, imaging tests, and sometimes laboratory tests.
- Physical examination
- A doctor will assess the range of motion, look for swelling, tenderness, or deformity, and evaluate your ability to move the knee.
- X-rays
- Doctors can use an X-ray to diagnose knee osteoarthritis, as it shows joint space narrowing, bone spurs (osteophytes), and cartilage loss.
- Magnetic resonance imaging (MRI)
- While not routinely needed, an MRI can provide detailed images of the knee's soft tissues, including cartilage, ligaments, and muscles.
- Joint fluid analysis
- In some cases, the doctor may remove fluid from the knee joint (joint aspiration) to check for signs of inflammation or other types of arthritis.
- Blood tests
- While there is no specific blood test for osteoarthritis, blood tests can be used to rule out other forms of arthritis, such as rheumatoid arthritis.
How to treat knee osteoarthritis?
Treatment for knee osteoarthritis focuses on relieving symptoms, improving joint function, and slowing the progression of the disease. The approach may include a combination of lifestyle modifications, physical therapies, medications, and surgical options.
Non-surgical treatments
Lifestyle changes
Weight management: Reducing body weight can significantly reduce stress on the knees, alleviate pain, and slow the progression of osteoarthritis.
Exercise: Regular low-impact exercise (e.g., swimming, cycling, or walking) strengthens the muscles around the knee, improves flexibility, and enhances joint function.
Avoiding risky activities: You can prevent joint pain by avoiding actions that place a lot of stress on your knees, such as high-impact sports or prolonged standing.
Physical therapy
A physical therapist can guide you through exercises that improve strength, flexibility, and balance, helping to reduce pain and improve joint function.
Techniques such as heat or cold therapy, ultrasound, or electrical stimulation may also provide relief.
Medications
Pain relievers: Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as Arcoxia or ibuprofen can help manage pain and reduce inflammation.
Topical creams: You can apply lotions or gels containing NSAIDs directly to the knee to relieve pain.
Corticosteroid injections: Injections of corticosteroids into the knee joint can reduce inflammation and provide temporary pain relief, but they are not recommended for long-term use.
Hyaluronic acid injections: Viscosupplementation involves injecting hyaluronic acid into the knee to provide lubrication and reduce pain.
Platelet-rich plasma (PRP) injections: PRP injections are suitable for people with early-stage osteoarthritis, with a high concentration of platelet-stimulating soft tissue healing.
Assistive devices
Using knee braces or a cane can help support your knee joint, relieve pain, and improve mobility.
Surgical treatments
For severe knee osteoarthritis, surgery may be necessary when non-surgical treatments fail to provide relief.
Arthroscopy
This minimally invasive procedure involves inserting a small camera into the knee to clean out loose cartilage or repair minor damage.
Osteotomy
This surgical procedure involves reshaping the bones to relieve pressure on the damaged part of the knee. Younger patients or those with limited cartilage damage typically undergo this procedure.
Partial knee replacement
If only one part of the knee is affected, a surgeon may perform a partial knee replacement, preserving the healthy parts of the joint (including the native ligaments) while replacing the damaged area only.
Total knee replacement (TKR)
In more advanced osteoarthritis, total knee replacement surgery can be used to replace the entire knee joint with an artificial joint (prosthesis). This surgery is highly effective in reducing pain and improving function in patients with severe arthritis.
With improved surgical technique and better anaesthesia care, patients now have significantly less pain after surgery and can recover faster. Patients have the option to have their TKR surgery performed as a day surgery procedure under the ERAS clinical pathway.
Knee osteoarthritis specialists
Loading...
Living with knee osteoarthritis
Knee osteoarthritis is a chronic condition that requires long-term management. While there is no cure, adopting certain lifestyle changes can help improve the quality of life.
Stay active
Engage in regular physical activity to maintain joint function and overall health.
Protect your joints
Use proper posture and techniques during your everyday activities, and remember to take regular breaks to avoid tiring yourself out.
Pain management
Combine treatments like exercise, medications, and physical therapy to manage pain and prevent flare-ups.
FAQ
Is it possible to cure knee osteoarthritis?
There is no cure for knee osteoarthritis, but treatment can help manage symptoms, slow the progression of the disease, and improve quality of life.
How is knee osteoarthritis different from rheumatoid arthritis?
Knee osteoarthritis is a degenerative joint disease caused by the breakdown of cartilage due to wear and tear, while rheumatoid arthritis is an autoimmune disorder that causes inflammation of the joints. Osteoarthritis typically affects only specific joints, whereas rheumatoid arthritis can affect multiple joints symmetrically.
What are the first signs of knee osteoarthritis?
The first signs may include joint pain during activity, stiffness after inactivity, and swelling around the knee joint.
Is surgery always necessary for knee osteoarthritis?
No, surgery is not always necessary. Many people with knee osteoarthritis can manage their symptoms with non-surgical treatments such as physical therapy, medications, and lifestyle changes. Surgery is usually considered when these treatments no longer provide adequate relief.
What types of exercise are best for knee osteoarthritis?
Low-impact exercises like swimming, cycling, walking, and strength training are excellent for people with knee osteoarthritis. These exercises help strengthen the muscles around the knee and improve joint flexibility without putting too much stress on the joint.
Can weight loss help with knee osteoarthritis?
Yes, weight loss can significantly reduce the stress on the knee joints and alleviate pain. Even losing a small amount of weight can make a big difference in symptom management and disease progression.
Are there any dietary supplements that can help with knee osteoarthritis?
Supplements like glucosamine, chondroitin sulphate and collagen are commonly used, but research on their effectiveness has been mixed. Always consult your doctor before taking any supplements.
How often should I see my doctor if I have knee osteoarthritis?
If you have knee osteoarthritis, you should have regular check-ups with your doctor, especially if your symptoms are worsening or if you're trying new treatments. Unless the severity of the symptoms indicates otherwise, most patients see their doctor every 6 to 12 months.
What are the risks of total knee replacement surgery?
As with any surgery, total knee replacement carries small risks such as infection, blood clots, and complications related to the prosthesis. However, it is a highly successful procedure for relieving pain and improving function in severe cases of knee osteoarthritis.
How can I prevent knee osteoarthritis from getting worse?
To slow the progression of knee osteoarthritis, maintain a healthy weight, stay active with low-impact exercises, manage pain with medications or physical therapy, and protect your knees by avoiding high-impact activities.
This information is intended for general guidance only and should not be considered as medical advice. To receive personalised recommendations and tailored advice, request an appointment with Thomson Medical. Our doctor can help provide the necessarry orthopaedic services for your specific conditions.
For more information, contact us:
Thomson Specialists (Thomson Medical Centre) — Orthopaedic
Request an AppointmentDr Jerry Chen
Orthopaedic Surgery
Thomson Specialists (Thomson Medical Centre)
English, Mandarin, Cantonese, Hokkien
Income, Great Eastern, AIA, Singlife and 4 others

