Becoming a parent brings joy, excitement, and sometimes a lot of questions, especially when it comes to feeding your baby. You may have heard the term “lactation” and wondered what it really means, how your body prepares to produce milk, or what to do if feeding does not go as smoothly as you expected.
Many parents share these worries, and it is completely normal to feel unsure at the start. Lactation is the natural process through which your body produces breast milk to nourish your baby.
While your body is designed to support this process, learning how lactation works and knowing what to expect can help you feel more reassured and supported as you begin your feeding journey.
What is lactation?
Lactation is the biological process that enables your body to make milk for your baby. It begins during pregnancy and continues after your baby is born.
Your breasts contain milk-producing glands, called mammary glands, along with tiny lactiferous ducts that carry milk to your nipples. When your baby feeds, these glands work together to provide the nutrition for your little one.
The truth is, your body starts preparing for lactation long before your baby arrives.
This preparation is guided by two hormones:
Prolactin: sends a signal to your body to make milk
Oxytocin: helps the milk flow when your baby feeds
Together, they create a natural system that responds to your baby’s needs. It also adjusts both the amount and composition of milk as your baby grows.
Stages of lactation

Lactation doesn’t happen all at once. It happens in stages. Each plays an important role in your breastfeeding journey.
Stage 1: Pregnancy (Lactogenesis I):
You might notice your breasts feeling fuller, maybe a bit tender. That's the milk-producing tissue developing.
Later in pregnancy, you may see a thick, yellowish fluid leaking from your nipples. Don't worry. That's colostrum, and it's actually a good sign that your body is getting ready to produce milk.
Stage 2: Milk coming in (Lactogenesis II):
Within two to five days after birth, your milk comes in. Your breasts become fuller, heavier, and maybe tender.
The colostrum you made earlier slowly changes into mature milk, which looks thinner and whiter. This shift happens naturally as your baby grows and needs more milk.
Stage 3: Established milk production (Lactogenesis III):
Within a few weeks after birth, your breast milk supply is established. This stage can last as long as you continue to feed your baby.
Your milk production works on a supply-and-demand basis. This means the more your baby feeds, the more milk your body makes.
Every mother’s lactation experience is unique. However, knowing what to expect at each stage helps you recognise the changes in your body during the process. It allows you to be proactive when you may need additional support and feel more prepared for your breastfeeding experience.
Common challenges of lactation
Many parents experience bumps along the way with lactation. It’s natural to worry about these challenges, but having them doesn’t mean you’re doing anything wrong. They are actually very common and manageable.
Some of the concerns you may face include:
Low milk supply worries:
Many new parents worry that they’re not producing enough milk. This concern is valid, but actual low milk supply is less frequent than you may think.
Breast engorgement:
When your milk first comes in, your engorged breasts may feel uncomfortably full and tight. However, this usually eases within a few days as your body adjusts to your baby’s feeding pattern. Frequent feeding and gentle breast massage can help you feel better.
Blocked ducts:
Sometimes a milk duct can become blocked, which then creates a tender lump in your breast. This can happen because of infrequent feeding or incomplete milk removal. Still, continuing to feed regularly and applying warm compresses can help clear the blockage.
Mastitis:
This is an inflammation of breast tissue that can sometimes involve an infection. You may experience flu-like symptoms, breast pain, and redness. If you think you have mastitis, it’s best to check with your doctor as soon as possible. It’s treatable, and catching it early can make a big difference.
You may wonder what these challenges may mean for your breastfeeding journey. Fortunately, experiencing any of these challenges doesn’t mean your body can’t produce milk successfully. With the right support and guidance, most issues resolve, and many parents go on to have positive lactation experiences.
If you're experiencing any of these lactation challenges or have concerns about your milk supply, don't hesitate to seek help. Schedule an appointment with Thomson ParentCraft Centre, and our lactation counsellors will provide personalised lactation support to help you navigate your breastfeeding journey with confidence.
Our ParentCraft trainers
Loading...
Factors that affect milk production
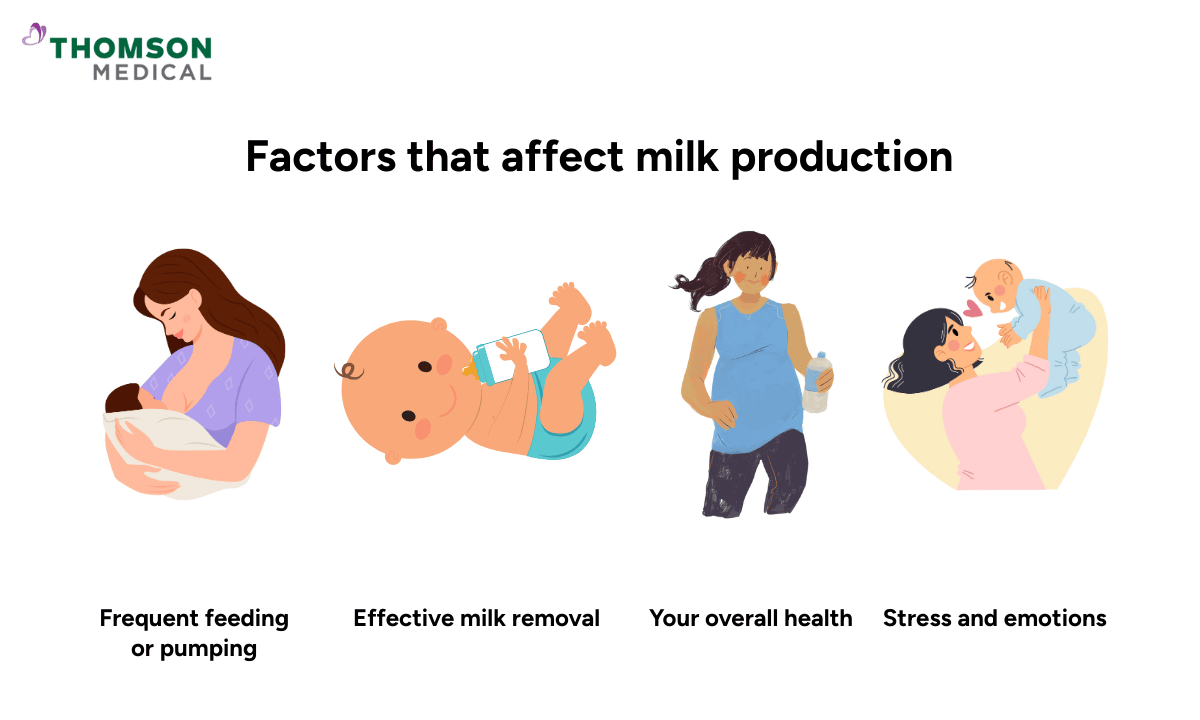
Your milk supply isn’t fixed. Instead, it responds to your baby's feeding.
This means that when your baby feeds frequently, your body receives the signal to produce more milk.
However, when feeding is less frequent, your body naturally adjusts and makes less milk. This responsive system proves your body is completely capable of providing what your baby needs throughout their growth and development.
However, your milk production can be influenced by some factors, including:
Frequent feeding or pumping:
The more your baby needs, the more your body produces. In the first few weeks, feeding eight to twelve times in 24 hours is typical and helps establish a strong supply.
Effective milk removal:
It involves how well the milk is being removed, not just how often you feed. When your baby latches well and feeds effectively, this sends strong signals to your body to keep producing milk.
Your overall health:
Your body needs energy to make milk. That’s why having a healthy lifestyle, such as drinking enough water, eating nutritious foods, and getting adequate rest, can support your lactation.
Stress and emotions:
Occasional stress is normal, but high stress levels can sometimes affect your milk let-down reflex and make it harder for milk to flow. Giving yourself time to rest or finding moments to relax can ease stress and support milk flow.
Some mothers can produce milk easily, while others may need additional support, and that’s normal. If you’re concerned about your milk supply, it’s helpful to know that there are effective ways to improve and boost production. Your doctor can evaluate your condition and create personalised guidance based on your specific situation.
How to support healthy lactation
Supporting lactation isn’t complicated. Still, it requires some attention to your body and your baby’s needs.
Here are some practical ways you can try to support healthy lactation:
Feed responsively and frequently:
Feeding your baby frequently, especially in the early weeks, is one of the best ways to establish your milk supply. You can watch for early hunger cues from your little one, such as rooting or bringing hands to mouth, and respond promptly.
Take care of your nutrition:
Your body is doing incredible work producing milk, so it’s important to support it with good nutrition. Make sure to add protein, healthy fats, fruits, and vegetables to your diet.
Prioritise rest when possible:
Lack of sleep is a real challenge with a newborn, but rest is important for hormone balance and milk production. Try to nap when your baby naps if you can. Caring for yourself is caring for your baby, too.
Manage stress and seek support:
The first few weeks of parenthood can feel overwhelming, so don’t hesitate to reach out for support, whether from your partner, family, friends, or people who have experience. This can help ease stress and create a more positive lactation experience.
Know when to ask for help:
If you’re experiencing nipple pain or concerns about your milk supply, consulting your doctor or a lactation consultant is the right move to make.
As first-time parents, it’s normal to have questions and moments of uncertainty about lactation. Remember, your body is learning too. Lactation is a gradual, responsive process that adapts over time with care and patience. With the right support, both you and your baby will find your rhythm together.
If you need support with lactation or have questions about your breastfeeding journey, schedule an appointment with Thomson ParentCraft Centre. Our lactation consultants will provide personalised support tailored to your needs.
FAQ
Does breast size affect milk production?
No, breast size doesn't determine how much milk you can produce. Instead, it depends on your mammary gland tissue, not the amount of fatty tissue in your breasts. Women who have smaller breasts can produce just as much milk as those with larger breasts.
What if I can't produce enough milk?
If you're concerned about low milk supply, there are strategies to help, including:
More frequent feeding or pumping
Ensuring effective milk removal
Medication or supplements
Can breast surgery affect lactation?
It depends on the type of surgery you had and whether it affected your milk ducts or nerves. Some people can lactate successfully after breast surgery, while others may experience reduced milk production. Discussing your specific situation with your doctor and a lactation consultant before your baby arrives can help you plan ahead.
How long does it take for milk to come in?
Most people experience their milk coming in within two to five days after giving birth. In the meantime, your body produces colostrum, which is perfectly designed for your newborn's tiny stomach and provides essential nutrients and immune protection.
Can I increase my milk supply naturally?
Yes, in most cases. The most effective method is frequent feeding or pumping, about eight to twelve times in 24 hours. Beyond that, it’s also important to stay hydrated, eat well, manage stress, and ensure your baby is latching well
Why does one breast produce more milk than the other?
This is completely normal and very common. Most people have one breast that produces slightly more milk than the other, often because it has more milk-producing tissue or better milk flow. As long as your baby is growing well and you're not uncomfortable, there's no need to worry about this difference.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
