If you have been advised to undergo a pelvic MRI to assess an ovarian cyst, it is natural to feel uncertain about what that means. Often, an ultrasound may show findings that require a closer look before treatment decisions are made.
Most ovarian cysts are harmless and monitored with ultrasound alone. An MRI is typically recommended when more detailed imaging is needed to better understand the nature of a cyst. Knowing how this scan supports accurate diagnosis and planning can help ease concerns and give you clearer expectations about the next steps.
What is MRI?
Magnetic Resonance Imaging (MRI) is a scan that uses strong magnetic fields and radio waves to create images of your internal organs and soft tissues. Unlike X-rays or CT scans, MRI does not involve radiation exposure.
A pelvic MRI examines organs in your lower abdomen and pelvis, including your:
Ovaries
Uterus
Fallopian tubes
Bladder
Surrounding soft tissues
The images produced by MRI allow doctors to examine tissue characteristics and anatomical structures in detail, which can be helpful when ultrasound findings require further clarification. Your doctor can use this information to discuss your results and give you answers instead of leaving you with more questions.
Our gynaecology specialist
Loading...
Why do I need an MRI scan for an ovarian cyst?
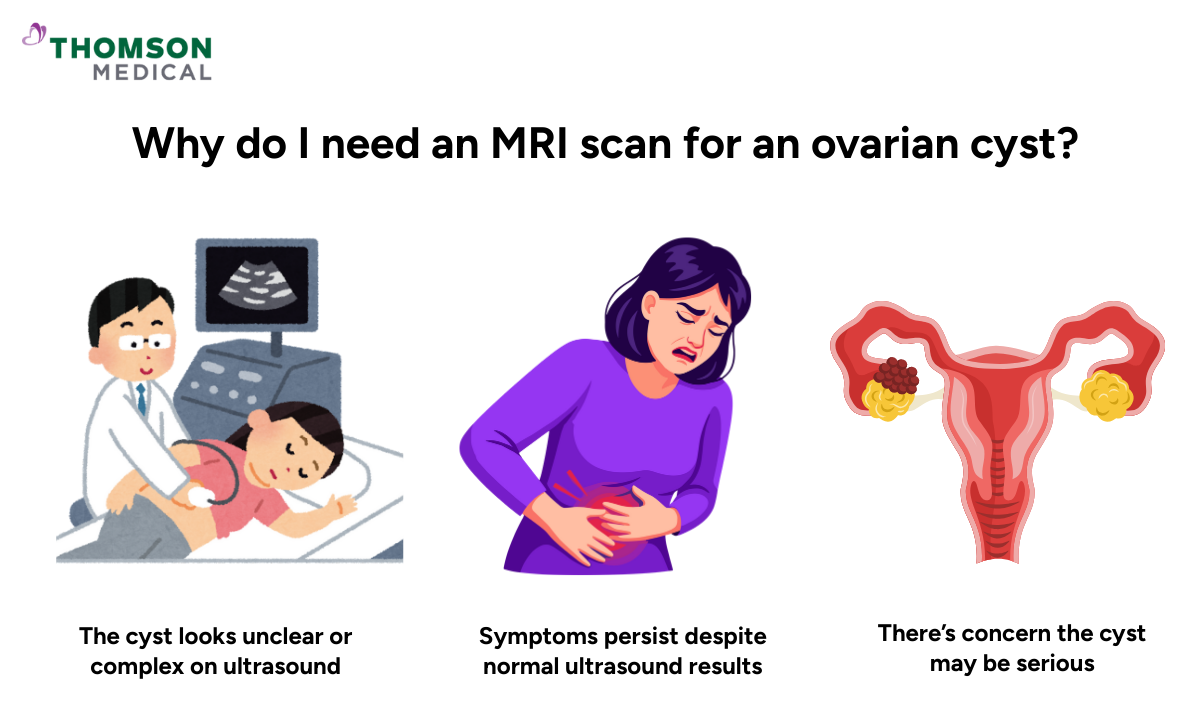
Being told you need an MRI can feel unsettling. It might seem like your doctor is looking for something serious. However, not everyone with an ovarian cyst needs an MRI. Your doctor has recommended this scan for specific reasons.
A pelvic MRI may be recommended if:
An ovarian cyst looks complex or unclear on ultrasound
The cyst has solid components or irregular features
Your symptoms like pelvic pain and changes in menstrual cycle continue despite normal ultrasound findings
There is concern about whether the cyst might be serious
Your doctor is planning surgery and needs more detailed information
MRI shows the size, type, and contents of your cyst. It can tell whether you have a simple fluid-filled cyst, one with blood, or something more complex. This helps doctors work out whether it's benign (non-cancerous) or needs further investigation. Most of the time, the scan confirms the cyst is harmless.
Advantages of an MRI scan for ovarian cysts
Pelvic MRI can provide information that may be helpful in certain clinical situations.
These include:
Soft tissue detail
Helps tell the difference between simple cysts, hemorrhagic cysts, endometriomas, dermoid cysts, and tumours
Better evaluation of complex cysts or unclear pelvic masses
No radiation exposure
More accurate assessment of cyst contents (fluid, blood, fat, or solid components)
This detail can save you from unnecessary worry or procedures. Often, something that looks suspicious on ultrasound turns out to be completely benign on MRI. Your doctor uses this information alongside your symptoms and medical history to plan the right treatment from the start or confirm you need no treatment at all.
If your doctor has suggested a pelvic MRI and you’re feeling unsure, getting clear guidance can make a big difference. Request an appointment at Thomson Medical to review your scan findings, understand exactly why the MRI is needed, and discuss the next steps based on clear, detailed results.
Is pelvic MRI safe?
You might be worried about whether the MRI is safe for you, especially if you have any medical devices or implants. The good news is that pelvic MRI is generally considered safe for most people when appropriate safety screening is conducted.
Key safety points include:
No radiation is used
Generally considered appropriate for repeated scans if needed
Contrast agents (a substance used in medical imaging) are well tolerated in most patients
However, MRI may not be suitable if you have certain implanted medical devices (such as older pacemakers), metal fragments in your body, or severe kidney disease (if a contrast agent is required).
Always inform your doctor about any implants, metal exposure, or pregnancy before the scan. This helps them make sure the scan is safe for you.
How to prepare for a pelvic MRI

Preparation can feel overwhelming, but the steps are straightforward.
You'll usually need to:
Wear loose, metal-free clothing or a gown
Remove jewellery, watches, and hair accessories
Fast for a few hours if contrast agent is planned
Tell staff if you are pregnant, claustrophobic (fear of confined spaces), or have any kidney problems
You may be asked to arrive early to complete screening forms. These forms help the team check for any safety concerns before your scan. It might feel like a lot of questions, but it's all to make sure the scan is safe and gives a quality scan.
What happens during an MRI scan?
Knowing what to expect can help you feel more comfortable on the day.
During the scan:
You lie on a narrow table that slides into the MRI machine
The radiographer communicates with you throughout the exam
You must remain still to get clear images
Loud tapping or thumping noises occur (ear protection is provided)
The scan typically lasts 30 to 60 minutes
If a contrast agent is used, it is injected through an intravenous line (IV) during the procedure. It helps certain tissues show up with different signal characteristics on the images. Most people don't feel anything when it's injected, though some notice a cool sensation.
What does an ovarian cyst look like on an MRI?
MRI provides information about the internal structure of ovarian cysts, which helps doctors work out what type of cyst you have.
Different cysts have different appearances:
Cyst type | What MRI shows | What it means |
Simple cysts | Smooth, thin-walled structures filled with clear fluid | Confirms it is usually harmless and need no treatment |
Haemorrhagic cysts | Distinctive signal patterns from blood products | Tells whether bleeding is recent or old, which helps doctors decide if monitoring is enough |
Endometriomas | Characteristic "shading" appearance | Helps confirm endometriosis when ultrasound findings are unclear |
Dermoid cysts | Fat, hair, or calcifications visible on the scan | Identify and differentiate from other masses |
Complex cysts | Solid components, thicker walls, or internal divisions | Shows in greater detail than ultrasound for proper assessment |
Radiologists use these features to help determine whether a cyst is non-cancerous tissue growth or requires further examination. The information helps your doctor recommend the right next steps, whether that's monitoring, medication, or treatment.
Having an MRI doesn't mean something is seriously wrong. Most scans show benign cysts that need minimal or no treatment. Knowing exactly what you're dealing with helps you and your doctor move forwards and focus on the right care for you.
It’s important to understand what that means for your care. Request an appointment at Thomson Medical to have your MRI findings explained clearly, confirm what type of ovarian cyst you have, and discuss whether follow-up, monitoring, or treatment is needed.
FAQ
Can an MRI tell if an ovarian cyst is cancerous?
Pelvic MRI cannot definitively diagnose ovarian cancer, but it can provide information about whether a cyst has features consistent with benign conditions or whether it has characteristics that require further evaluation. Most ovarian cysts are benign, and the MRI provides information that contributes to this assessment.
Is an MRI better than a pelvic ultrasound?
MRI is not always better, but it is more detailed. Pelvic ultrasound is usually the first test because it's quick, widely available, and works well for most cysts. MRI is used when ultrasound results are unclear or show complex findings that need a closer look.
When is the appropriate time to get a pelvic MRI?
Timing depends on your menstrual cycle and clinical concern. In some cases, MRI may be performed after menstruation, when cyst persistence needs confirmation, or when symptoms are ongoing. Your doctor will advise on the appropriate timing for your situation.
How much does a pelvic MRI cost?
Costs depend on location, insurance, and whether contrast is used. Without insurance, pelvic MRI costs may range from several hundred to a few thousand dollars. Insurance coverage often requires prior authorisation, so check with your provider beforehand.
How much radiation is in a pelvic MRI?
None. MRI uses magnetic fields and radio waves, not radiation. This makes it an appropriate option for repeated imaging when medically necessary, as there is no radiation exposure involved.
What not to do before a pelvic MRI?
Following these simple guidelines helps ensure your scan goes smoothly.
Before an MRI:
- Do not wear metal or jewellery
- Avoid using lotions or makeup with metallic particles
- Do not eat or drink if instructed to fast
- Do not forget to disclose implants or medical devices
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment