Pregnancy is often described as a time of hope and joy. Many women imagine those first baby kicks and the anticipation of holding their child for the first time. But alongside all the excitement, there are conditions that can catch mothers by surprise. One of the most important is preeclampsia in pregnancy, a complication linked to high blood pressure during pregnancy that can put both mother and baby at risk if left untreated.
The word itself can sound frightening. Yet, the truth is most women with preeclamptic pregnancies receive the care they need and go on to deliver healthy babies. Knowing the signs, risks, and taking early action can make the difference.
What is preeclampsia?
Preeclampsia is a condition that only happens in pregnancy. It usually develops after the 20-week mark in women who previously had normal blood pressure. Doctors recognise it mainly through high blood pressure levels and changes such as protein in the urine. Some pregnancies progress without major issues.
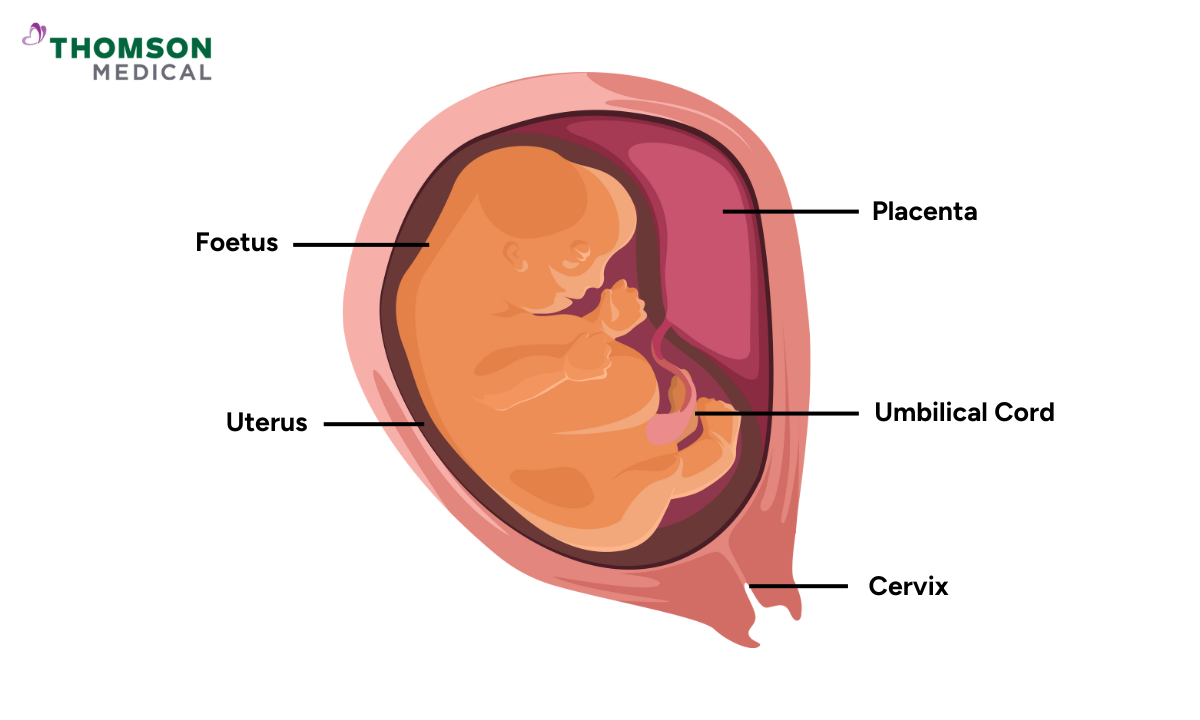
The condition is linked to the placenta, an important organ that supplies the baby with oxygen, blood and nutrients. If blood flow through the placenta becomes limited, the baby’s growth may be affected, and the mother’s organs, particularly the liver and kidneys, may come under strain. In severe cases, this can lead to placental ischaemia-induced hypertension, which requires careful medical monitoring.
What are the causes of preeclampsia?
The exact causes of preeclampsia are still not fully understood. In early pregnancy, new blood vessels are formed to help the placenta grow and work effectively. Sometimes blood vessels do not develop or function as they should, which can affect blood flow. This reduced blood flow seems to trigger the changes that lead to preeclampsia. Hypertens pregnancies with abnormal placental development will have a higher risk.
Recent research also shows that immune cells, such as peripheral blood mononuclear cells, may contribute to the inflammation observed in preeclampsia, linking the maternal immune system to heart disease risk later in life.
Other factors may also play a part, such as:
Immune system differences between mother and baby
Inflammation in blood vessels
Pre-existing hypertension or cardiovascular disease
Who is at risk of preeclampsia?
Some women face a higher risk of developing preeclampsia. You may be more at risk if you are:
A first-time mother
Carrying twins or multiples
Someone with a personal or family history of preeclampsia or coronary heart disease
Living with chronic conditions like diabetes, hypertension, or kidney disease
Mothers with autoimmune disorders
Over 35 years old
Overweight or obese before pregnancy
Knowing these risks allows doctors to give closer care and sometimes preventative treatments. High blood pressure during pregnancy is one of the most important signs doctors monitor closely.
Our O&G specialists
Loading...
What are the symptoms of preeclampsia?
One of the difficult things about preeclampsia is that it can sometimes develop quietly, without obvious warning signs. Many women feel perfectly well at the beginning, which can make it all the more unsettling. That’s why those regular antenatal checks are so important.
There are symptoms worth keeping an eye on:
High blood pressure (≥140/90 mmHg)
Detection of protein in the urine
Persistent or severe headaches
Blurred vision, flashing lights, or other changes in eyesight
Swelling of the face and hands
Pain under the ribs (often on the upper right abdomen)
Nausea or vomiting later in pregnancy
Rapid weight gain that doesn’t seem to have a clear cause
Even one of these symptoms is enough reason to contact a healthcare professional. Early review can make a real difference.
What are the complications of preeclampsia?
Without treatment, preeclampsia can progress quickly. If untreated, preeclampsia can lead to:
Preterm birth
Placental abruption
Low birth weight
Liver or kidney damage
Seizures, making this a medical emergency
HELLP syndrome (Haemolysis, Elevated Liver enzymes, Low Platelets), which requires urgent treatment
Increased risk of heart disease and cardiovascular disease later in life
Abnormalities in the preeclamptic placenta, which can affect fetal oxygen supply
What’s the difference between preeclampsia and eclampsia?
Preeclampsia can make your blood pressure rise and put extra strain on your body. If it gets worse and causes seizures, it is called eclampsia. It’s completely natural to feel worried, yet it is important to know that it is very rare.
A seizure may look like sudden shaking, twitching, or blacking out for a short time. This happens because preeclampsia can affect the brain. When this occurs, doctors treat it straight away to keep both the mother and the baby safe.
In hospital, the mother would usually be given medicine to calm the seizures and bring the blood pressure down. Sometimes, doctors may suggest delivering the baby early if that is the safest choice.
How do doctors diagnose preeclampsia?
Doctors use a number of medical tests to confirm preeclampsia, and these include:
Checks for blood pressure
Protein level in urine test
Blood test to measure platelet counts, kidney function, and liver enzymes
Doppler scans and ultrasounds to track the baby's blood flow and growth
A thorough examination of the symptoms
It is easier to manage preeclampsia and avoid serious consequences when it is diagnosed early.
If you notice any unusual symptoms during pregnancy, it is important to contact your healthcare provider and request for an appointment to ensure both your health and your baby's are closely monitored.
Treatment options for preeclampsia

The treatment depends on how far along the gestational age is and how severe the condition has become. The treatment includes:
Close monitoring
In mild cases, women may simply need more frequent visits, rest, and regular tests to keep track of blood pressure and organ function.
Medication
Doctors sometimes prescribe medicines to lower high blood pressure. In certain cases, magnesium sulfate is used to prevent seizures. If an early delivery seems likely, steroids can be offered to support the baby’s lung development.
Delivery
Ultimately, the only cure is giving birth. If preeclampsia worsens, doctors may recommend inducing labour or a caesarean section, sometimes before the gestational age has reached full term.
The reassuring point is that with modern monitoring and treatments, most women recover well, and most babies are safe.
FAQ
Can you deliver naturally with preeclampsia?
Yes, natural delivery is possible if the condition is stable. Labour is often induced, and vaginal birth may be safe. However, if the risks increase, a caesarean may be necessary.
Does preeclampsia go away after delivery?
In most cases, yes. Blood pressure and organ function usually return to normal pregnancy levels within days or weeks. Doctors will continue to watch carefully during the postpartum period.
What is postpartum preeclampsia?
Postpartum preeclampsia is a rare form that appears after birth, often within 48 hours, but sometimes up to six weeks later. It requires urgent care to prevent seizures and other complications.
Can a baby survive preeclampsia?
Yes, many babies do well and survive, especially when the condition is spotted early and treated effectively. However, the risks include preterm birth or growth problems, but medical care greatly improves outcomes.
What are the three early signs of preeclampsia?
High blood pressure, protein in the urine test, and swelling in the hands and face during pregnancy are the most common early indicators of preeclampsia.
What week of pregnancy does preeclampsia start?
It typically develops after 20 weeks of gestational age, though it can appear later or, rarely, after birth.
Is there a cure for preeclampsia?
The only cure is delivery of the baby and placenta. Until that point, doctors will manage the symptoms to keep both mother and baby safe. Careful monitoring throughout pregnancies complicated by preeclampsia ensures the best outcomes.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
