The moment you’ve been waiting for is almost here. Whether it’s your first baby or your third, giving birth can feel both exciting and a little anxious. You may wonder what labour feels like, how long it will last, or what happens if things don’t go as planned.
Labour usually follows a natural rhythm, and your medical team will guide you every step of the way. Knowing what to expect, from your first contraction to holding your baby, can help you feel calm and ready.
What are the signs of labour?
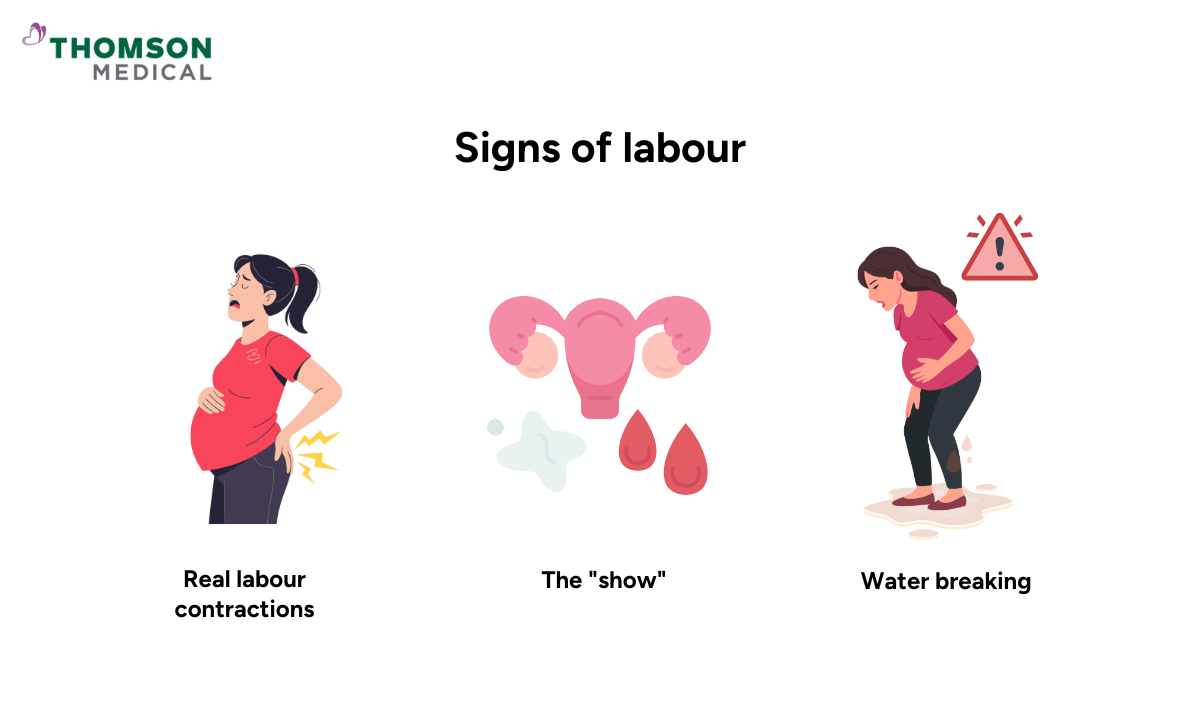
Your body gives you clear signals when it's time to meet your baby. Here's what to watch for:
Real labour contractions
Real labour contractions are not the same as practice contractions (called Braxton Hicks). Real contractions get stronger, last longer, and come closer together. They feel like strong period cramps or a tightening that comes and goes. Practice contractions are irregular and usually stop when you move or change position.
The "show"
Throughout pregnancy, your cervix (the opening to your womb) is sealed with a mucus plug. When labour starts, this plug comes out and you'll see thick, bloody mucus on your underwear. This is completely normal.
Water breaking
Your baby sits in a sac filled with fluid. When this sac breaks, you might feel a sudden gush of water or a steady trickle. This can happen before contractions start.
When to head to the hospital?
Knowing the right time to head to the hospital can feel confusing, but there are clear signs to watch for.
Head to the hospital when:
Contractions are regular, lasting about 60 seconds, and coming every 5 minutes
Your water breaks
You're vaginal bleeding heavily
Your baby is moving less than usual
You feel an intense urge to push
If you're unsure, call your hospital or doctor for guidance.
What are the three stages of labour?
Labour happens in three stages, and each has a clear purpose. Knowing what to expect can help you feel more prepared and less anxious.
Stage 1a: Early phase of labour
Your body is starting to get ready for birth. This is when cervical dilation begins. Your cervix gradually opens from 0-4 centimetres to make space for your baby to move down. You can usually stay home, rest, drink water, eat light snacks, walk, or take a warm shower.
Stage 1b: Active phase of labour
The cervix opens from 4-10 cm, and contractions become stronger, longer, and closer together. First-time moms usually spend 4-8 hours in this phase. You should be at the hospital, and the last part (7-10 cm) is called transition, which is the toughest but shortest, usually 15-60 minutes.
Stage 2: Pushing and birth
Once the cervix is fully open, you’ll feel a strong urge to push. Your baby moves down the birth canal with guidance from your doctor. You can try positions like squatting, side-lying, or hands-and-knees.
Stage 3: Delivering the placenta
After your baby is born, the placenta comes out. Contractions are mild, and this usually takes 5-30 minutes. During this stage, the umbilical cord and placenta are carefully checked to ensure everything is complete. Your doctor will stitch any tears if needed.
Our O&G specialist
Loading...
How are babies delivered?
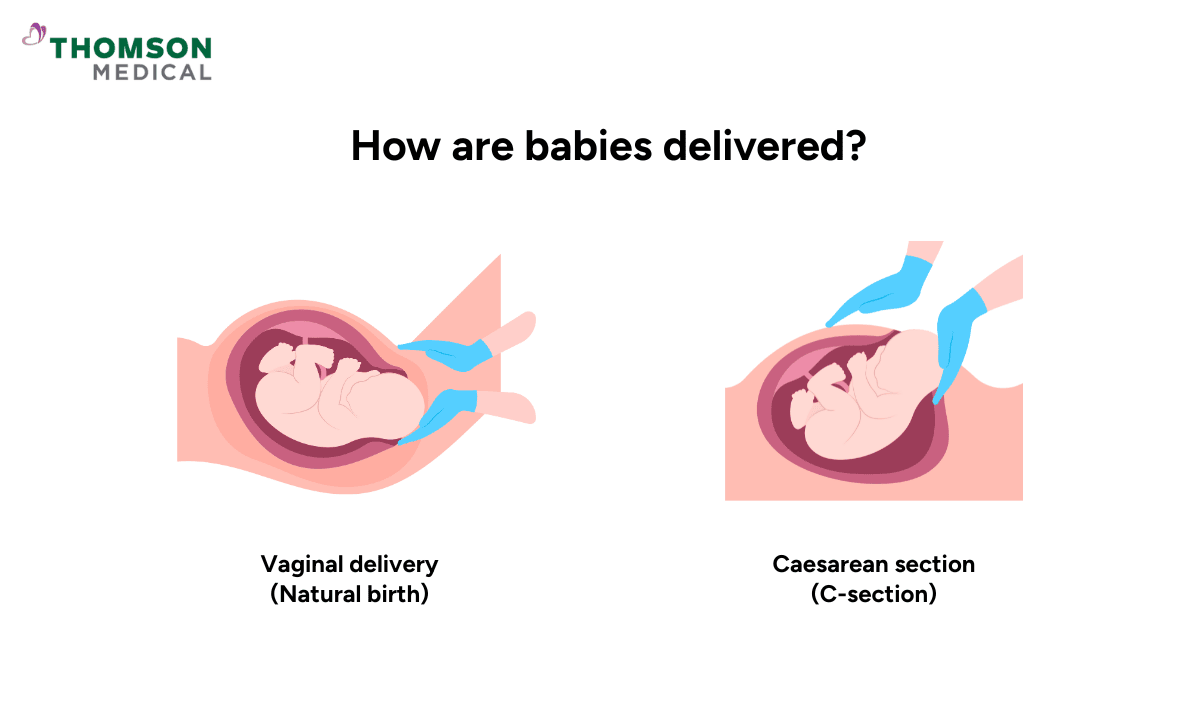
Every delivery is different, but there are two main baby delivery methods your baby can be born. Let's break down what each one involves.
| Vaginal delivery (natural birth) | Caesarean section (C-section) | |
|---|---|---|
| How it happens | The baby comes out through the birth canal. | The baby is delivered through a cut in the belly and womb. |
| Commonality | Most babies are born this way. | Less common, done either planned or in an emergency. |
| Benefits | You recover faster, stay in hospital 1-2 days, and your baby has fewer breathing problems. | Can be safer in certain situations and is planned if needed. |
| When needed | Safe for most pregnancies. | Needed if the baby is not head-down, you have twins, the placenta blocks the way, labour is slow, the baby is in distress, or there are medical issues. |
Remember that every birth is unique. Regardless of your birth plan or delivery method, what matters most is a safe and healthy outcome for both you and your baby.
If you’re expecting and want to understand which delivery method may be safest for you and your baby, request an appointment with Thomson Women's Clinic. Our specialists can guide you through your options and help you prepare for a smooth, confident birth experience.
When assistance is needed during baby delivery?
Sometimes, babies need a bit of help during delivery, and that’s completely normal. Your doctor may step in to make sure both you and your baby stay safe.
To assist, your doctor might use forceps or a vacuum. Forceps are tools that gently guide your baby’s head out. They may leave small marks on your baby’s face, but these usually fade after a few days.
A vacuum (also called a ventouse) uses a soft suction cup to help your baby move down as you push. Your baby’s head might look slightly cone-shaped for a day or two, but it quickly returns to normal. Both methods are safe when used by experienced doctors and are only done when truly necessary to help ensure a safe delivery for you and your baby.
What pain relief options are available during Labour?
Labour can be painful, but there are many ways to make it easier. You don’t have to go through it alone or without help.
Non-medical comfort options
Breathing and relaxation techniques, warm showers, gentle massages, or changing positions can help you stay calm and comfortable. Listening to music or having your partner’s support also helps you cope with contractions.
Medical pain relief options
If you need more relief, your doctor or midwife can offer safe medical options. The most common is an epidural, which reduces pain in the lower body while keeping you awake. Some women also use laughing gas (Entonox), which helps take the edge off during contractions. In certain cases, medication may be given through an injection or drip to ease the pain.
What to expect during postbirth recovery
Recovery during postbirth looks different for everyone, but giving your body time to heal is just as important as caring for your newborn.
If you had a vaginal birth, you’ll likely be able to move around within a few hours. Most mums stay in the hospital for a day or two and may feel sore for a week or two. Light activities are fine after a few days, but it’s best to wait around six weeks before returning to exercise or sex.
If you had a C-section, recovery takes a little longer. You’ll usually stay in the hospital for three to five days and may need help moving around at first. The incision can feel sore for a couple of weeks, and full recovery can take up to eight weeks.
If you feel persistently sad, anxious, or overwhelmed, you don’t have to go through it alone. Request an appointment with specialists at Thomson Medical. Our specialists can support your recovery, monitor your healing, and provide guidance to help you adjust to life after giving birth.
FAQ
Can I eat or drink during labour?
Many doctors allow clear liquids and light snacks during early labour. Once active labour begins, you may be restricted to ice chips or clear liquids to prevent complications in case anaesthesia or surgery becomes necessary.
How soon can I resume normal activities after childbirth?
Recovery times vary. Most women can resume light activities within a few days to weeks. Strenuous exercises and heavy lifting should wait 4-6 weeks or longer. Follow your doctor's guidance and listen to your body.
Can I have a vaginal birth after a caesarean section (VBAC)?
In many cases, yes. A vaginal birth after the previous C-section is possible and safe, but it depends on factors like why you needed the previous C-section and your current health. Discuss VBAC with your obstetrician.
What's the hardest part of labour?
The transition phase, when the cervix fully dilates from 7-10 centimeters, is often considered the most challenging. Contractions are very intense and close together.
What is more painful, C-section or natural birth?
Pain perception varies for everyone. Natural birth involves labour pain during delivery, while C-section involves postoperative pain during recovery. Both have different pain experiences.
How many hours is normal labour?
Labour duration varies. For first-time mothers, normal labour typically lasts around 12 to 18 hours from start to finish. For second or later babies, it's usually faster (5-12 hours).
How long should you push for the first baby?
Pushing for your first baby can last from a few minutes to several hours. The average is 1 to 2 hours, but it can go up to 3 hours and still be considered normal.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Dr Ryan Lee Wai Kheong
Obstetrics & Gynaecology (O&G)
Thomson Specialists Woodleigh (Women's Health)
English, Mandarin
Prudential, Great Eastern, Adept, MHC and 4 others

