If you’re expecting a baby, you’re probably familiar with an oral glucose tolerance test (OGTT). This diagnostic assessment is often carried out between the 24th and 28th weeks of pregnancy or earlier if the mother-to-be has risk factors for gestational diabetes. Read on to find out everything you need to know about an oral glucose tolerance test.
What is an oral glucose tolerance test (OGTT)?
A glucose tolerance test (GTT), also called a glucose challenge test, is used to find out how well your body processes sugar (glucose). It helps doctors diagnose conditions like pre-diabetes and diabetes mellitus.
Glucose is a type of sugar that comes from the carbohydrates in the food and drinks you consume. It is your body’s main source of energy and is stored in the liver and muscles as glycogen for later use.
To keep your blood glucose at a healthy level, your body uses a hormone called insulin, which is made by the pancreas. Insulin helps move glucose from your bloodstream into your cells, where it is used for energy.
If you have pre-diabetes or diabetes:
Your pancreas may not produce enough insulin
Or, your body may not respond properly to insulin
This leads to higher levels of glucose in the blood, which can cause health problems over time if not managed properly.
When should I do my oral glucose tolerance test?
Doing an oral glucose tolerance test (OGTT) depends on your age, medical history, diabetes risk factors, and whether or not you're pregnant. Here are some key guidelines:
Non-pregnant adults
Type 2 diabetes screening:
If you have no known risk factors, an OGTT is unneeded. Instead, you may be recommended periodic fasting blood glucose or A1C tests starting at age 45.
Prediabetes assessment:
If you have risk factors for diabetes (e.g., obesity, family history, sedentary lifestyle) or if fasting blood glucose or A1C tests are borderline, an OGTT may be recommended to you
Diabetes diagnosis:
If fasting blood glucose or A1C tests indicate diabetes, an OGTT may be used to confirm the diagnosis.
Pregnant women
Gestational diabetes (GDM) screening:
An OGTT is performed at 24-28 weeks of gestation. This interval is the recommended time for screening gestational diabetes, but it may be done sooner in a pregnancy if you have gestational diabetes risk factors or present diabetic symptoms.
Other situations
Polycystic Ovary Syndrome (PCOS):
If you have PCOS and are at risk of diabetes and insulin resistance, you may get an OGTT.
Assessment of insulin resistance:
An OGTT may be used to assess your insulin resistance in certain situations, such as suspected metabolic syndrome or acanthosis nigricans.
If you are pregnant or at risk of developing diabetes, an oral glucose tolerance test can help ensure early detection and better management of your health. Request an appointment with Thomson Medical today to discuss whether an OGTT is right for you.
Importance of doing OGTT
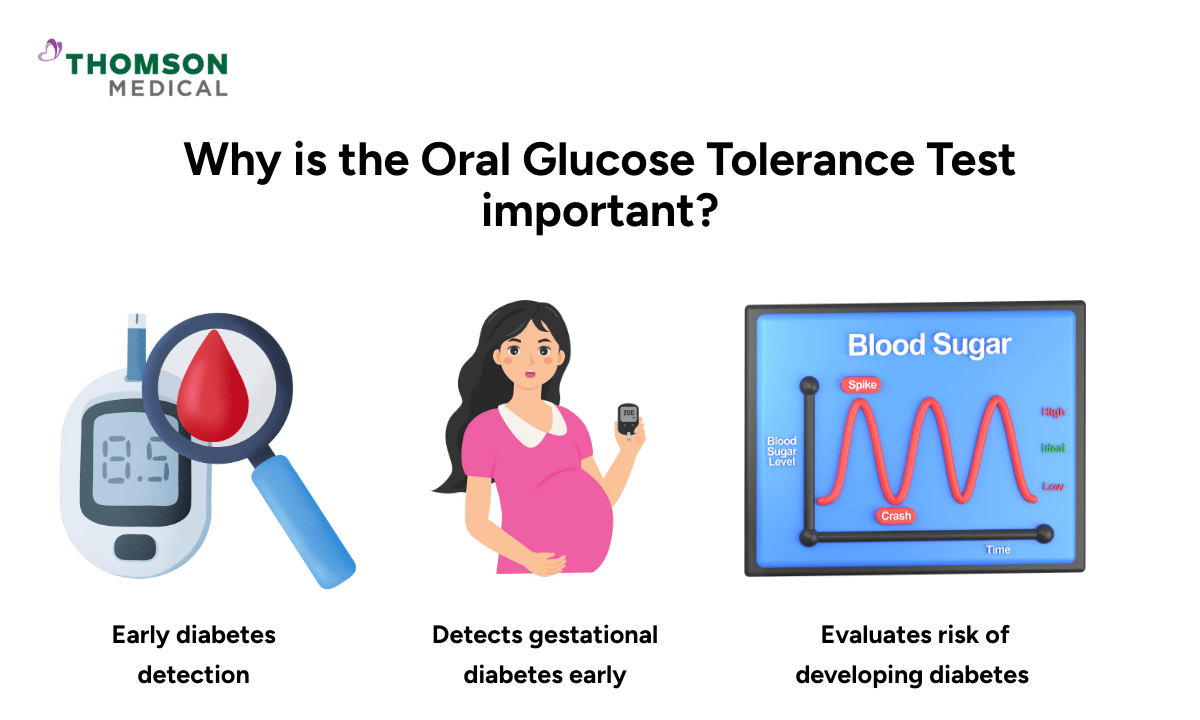
Early detection of diabetes:
OGTT can detect abnormalities in glucose metabolism before symptoms of diabetes appear, allowing for early intervention and management.
Gestational diabetes screening:
Identifying gestational diabetes early in pregnancy is crucial for reducing the risk of complications for both the mother and baby.
Personalised treatment:
The OGTT results help healthcare providers customise treatments, including lifestyle modifications, medication, and monitoring, to effectively manage diabetes.
Risk assessment:
OGTT helps assess an individual's risk of developing diabetes or other metabolic disorders, allowing for targeted preventive measures.
For pregnant women, the criteria for a diagnosis of gestational diabetes usually include meeting or exceeding one or more of the following blood glucose thresholds:
Fasting blood glucose level: 5.1 mmol/L or higher
Two-hour blood glucose level: 7.8 mmol/L or higher
How do I prepare for a glucose tolerance test?
Before your glucose tolerance test, it’s important to speak with your healthcare provider if you have any medical conditions or are taking medications or supplements that might affect the results.
To prepare for the test:
You must fast for at least 8 hours before the test. This means no food or drinks, except small sips of water.
Eat and exercise normally in the days leading up to the test.
Avoid intense physical activity just before the test, as it can affect your blood sugar levels.
Your provider will give you specific instructions based on your individual health needs.
What happens during a glucose tolerance test?
The most common version is the 2-hour oral glucose tolerance test (OGTT). Here's what to expect:
First blood sample:
A healthcare provider will draw a sample of blood from your arm to measure your fasting blood glucose level.
Glucose drink:
You’ll then be asked to drink a sweet liquid that contains 75 grams of glucose, usually dissolved in about 250 to 300 millilitres of plain water. You’ll need to drink it all within 5 minutes.
Waiting period:
You will wait for a specified time (usually two hours) without eating or drinking anything apart from water. Remain seated and avoid strenuous activity.
Second blood sample:
After the 2-hour waiting period, another blood sample will be taken to see how your body has processed the glucose over time.
The glucose dose may be different for children or pregnant women, depending on the type of test being performed.
What do the results of a glucose tolerance test mean?
The results of your glucose tolerance test show how your body responds to sugar. While reference ranges may vary slightly between laboratories, the general guidelines are:
Normal glucose tolerance
Fasting blood sugar: Below 100 mg/dL (5.6 mmol/L)
2-hour blood sugar: Below 140 mg/dL (7.8 mmol/L)
Impaired glucose tolerance (pre-diabetes)
Fasting blood sugar: 100–125 mg/dL (5.6–6.9 mmol/L)
2-hour blood sugar: 140–199 mg/dL (7.8–11.0 mmol/L)
Diabetes mellitus
Fasting blood sugar: 126 mg/dL or higher (7.0 mmol/L)
2-hour blood sugar: 200 mg/dL or higher (11.1 mmol/L)
Always refer to the reference values on your test report, and speak with your healthcare provider for a full explanation of your results and next steps.
Are there any side effects from an OGTT?
The glucose tolerance test is generally safe, but there are possible side effects associated with it:
Nausea:
Some may feel nauseous after taking the glucose solution if they have a sensitive stomach or if the solution is particularly sweet.
Dizziness or light-headedness:
Drinking a concentrated solution on an empty stomach can cause an increase in blood sugar levels, leading to feeling dizzy or lightheaded.
Blood draw discomfort:
Some may feel discomfort or bruising at the blood draw site.
Allergic reaction:
Although uncommon, some may see an allergic reaction to the glucose solution or materials used, such as the needle or tape used to fasten the IV line.
Hypoglycaemia:
In rare cases, the body may produce too much insulin, causing blood sugar levels to drop too low. This condition can result in sweating, trembling, confusion, or fainting.
False positive or false negative results:
While the OGTT is a valuable diagnostic tool, false-positive results (indicating a condition when it's not present) or false-negative results (missing a condition when it is present) can occur, leading to unnecessary worry.
If you begin to feel unwell during the test, please inform your healthcare provider immediately. These side effects typically resolve quickly once the test is complete and you're able to eat normally again.
FAQs
Where can one conduct an oral glucose tolerance test (OGTT)?
The oral glucose tolerance test (OGTT) is typically conducted in healthcare facilities, such as hospitals, clinics, or specialised diagnostic centres.
What happens if GTT is positive?
If GTT is positive, it may indicate you have pre-diabetes or diabetes mellitus. However, your healthcare provider may not make a diagnosis of pre-diabetes or diabetes mellitus based on one abnormal result. You may need to repeat another test shortly after or use another diagnostic test, such as HbA1c. It is best for you to discuss with your healthcare provider the following plan.
What are five signs that your blood sugar is too high?
Five signs of having high blood sugar are
Increased in thirst (polydipsia)
Increased in frequency and volume of passing urine (polyuria)
Frequent urination at nights (nocturia)
Feeling tiredness (fatigue)
Recurrent infections (skin infection and urinary infection)
What is gestational diabetes and why is it important to detect it?
Gestational diabetes is a temporary form of diabetes that occurs during pregnancy. It usually goes away after the baby is born, but it can increase the risk of high birth weight, premature delivery, and future health issues for both mother and child. Early detection allows for proper treatment and a healthier pregnancy.
Why is an OGTT done in pregnancy?
The oral glucose tolerance test (OGTT) is used to check for gestational diabetes, a type of diabetes that can develop during pregnancy. Most women are tested between 24 and 28 weeks, but the test may be done earlier if:
You have high sugar levels in your urine during routine prenatal check-ups
You are at higher risk of diabetes, such as having a family history, being overweight, or having had gestational diabetes in a previous pregnancy
Early detection helps ensure a healthier pregnancy for both you and your baby.
What happens if my OGTT results are abnormal?
If your results suggest gestational diabetes or another form of impaired glucose tolerance, your doctor will discuss a care plan with you. The plan may include changes to your diet, increased physical activity, and sometimes medication or insulin. Managing blood sugar helps prevent complications during pregnancy and childbirth.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
Request an Appointment_%CE%93%C3%87%C3%B4_What_do_you_need_to_know_1440x810.png%3Fbranch%3Dprod&w=3840&q=75)