You and your loved ones are excited about welcoming a new addition to the family. However, you are concerned that your baby might inherit a genetic condition from either of you. It’s natural if you feel upset or confused, but there are fertility treatments that can help.
One such treatment is preimplantation genetic testing for monogenic disorders (PGT-M), formerly known as preimplantation genetic diagnosis (PGD). This treatment helps in the identification of embryos that are not affected by the specific single-gene condition that you are at risk of passing down, lowering the likelihood that your child will inherit the condition.
What is Preimplantation Genetic Diagnosis (PGD)?
PGD is an older term that refers to a testing option available when there is a known single-gene genetic condition in your family, such as thalassaemia, cystic fibrosis, or sickle cell anaemia. This term has now been changed to preimplantation genetic testing for a monogenic disorder (PGT-M) for a more specific classification.
When used in conjunction with in vitro fertilisation (IVF), this test can help reduce the risk of passing on genetic disorders. This is because only embryos free of specific genetic disorders are chosen for transfer to your womb during the IVF process.
PGT-M (PGD at that time) has been used worldwide since the 1990s. In Singapore, it was first introduced in 2005 as part of a pilot programme by the Ministry of Health (MOH). Following successful outcomes demonstrating its safety and effectiveness, PGT-M transitioned to a regulated mainstream clinical service in May 2021.
Who should consider PGD?
Although PGT-M is performed alongside the IVF procedure, not every couple undergoing IVF will require this genetic testing. Such testing is usually recommended in situations where there is a known risk of passing on a genetic condition. Some groups who may benefit from this treatment include:
Couples with single-gene disorders:
If you and your partner carry a genetic condition such as thalassaemia, there's a 25% chance of passing it down with each pregnancy.
PGT-M can help reduce this risk by selecting unaffected embryos.
Preventing recurrence:
Parents of a newborn affected by a single-gene abnormality may use PGT-M testing to prevent recurrence in future pregnancies.
Mothers of advanced maternal age (AMA):
While PGT-M specifically addresses single-gene conditions, mothers of advanced maternal age (35 or older) may also benefit from genetic testing. This is because chromosomal abnormalities, which happen when embryos have too many or too few chromosomes, are more likely to happen at this age.
A different test called Preimplantation Genetic Testing for Aneuploidy (PGT-A) is designed to screen for these age-related chromosomal issues. However, PGT-A is currently not permitted as a routine procedure in Singapore, except under specific circumstances approved by the Ministry of Health.
If you or your partner are concerned that either of you may carry a single-gene condition that could be passed on to your children, don't hesitate to consult a fertility specialist. Schedule a consultation with Thomson Fertility Singapore.
Which genetic conditions can be tested with PGT-M in Singapore?
The Ministry of Health (MOH) regulates which genetic conditions can be tested through PGT-M in Singapore. This ensures the procedure is used appropriately for couples at risk of passing on an inheritable disease.
Autosomal dominant conditions:
Autosomal dominant means that only one parent needs to have an abnormal gene to pass it on. This means that if one parent has an abnormal gene, there is a 50% chance that it will be passed down with each pregnancy.
Examples include Huntington's disease (a condition that causes nerve cells in the brain to degrade), myotonic dystrophy (a condition that mainly causes progressive muscle loss and prolonged muscle contractions), and hereditary breast or ovarian cancer syndromes (BRCA1 or BRCA2).
Autosomal recessive conditions:
An autosomal recessive disorder means two copies of an abnormal gene must be present in order for the disease or trait to develop. Even if there are no symptoms, there's a 25% chance that the newborn will inherit both copies.
Examples include beta-thalassaemia (a severe type of thalassaemia), sickle cell anaemia (a condition that causes red blood cells to be misshapen like a sickle), cystic fibrosis, and spinal muscular atrophy (neuromuscular disorders that cause muscles to become weak).
X-linked conditions:
This genetic mutation is carried on the X chromosome, which is a type of sex chromosome. Males are more likely to inherit the mutation because they have only one X chromosome, whereas females have two.
Examples include Duchenne muscular dystrophy (a progressive condition that causes muscles to get weaker over time), haemophilia (a blood disorder that impairs the blood's ability to clot), and fragile X syndrome (an inherited condition that affects learning and development).
Our fertility specialists
Loading...
How is PGD performed?
Since PGT-M is performed as part of your IVF cycle, the process closely mirrors standard IVF with additional genetic testing. Here's what a typical treatment cycle involves:
Ovarian stimulation:
IVF treatment begins with the administration of fertility drugs designed to increase the number of eggs produced from the usual single egg released each month.
Because not all embryos may be unaffected by the genetic condition you're concerned about, producing several eggs gives you the best chance of success.
Egg retrieval:
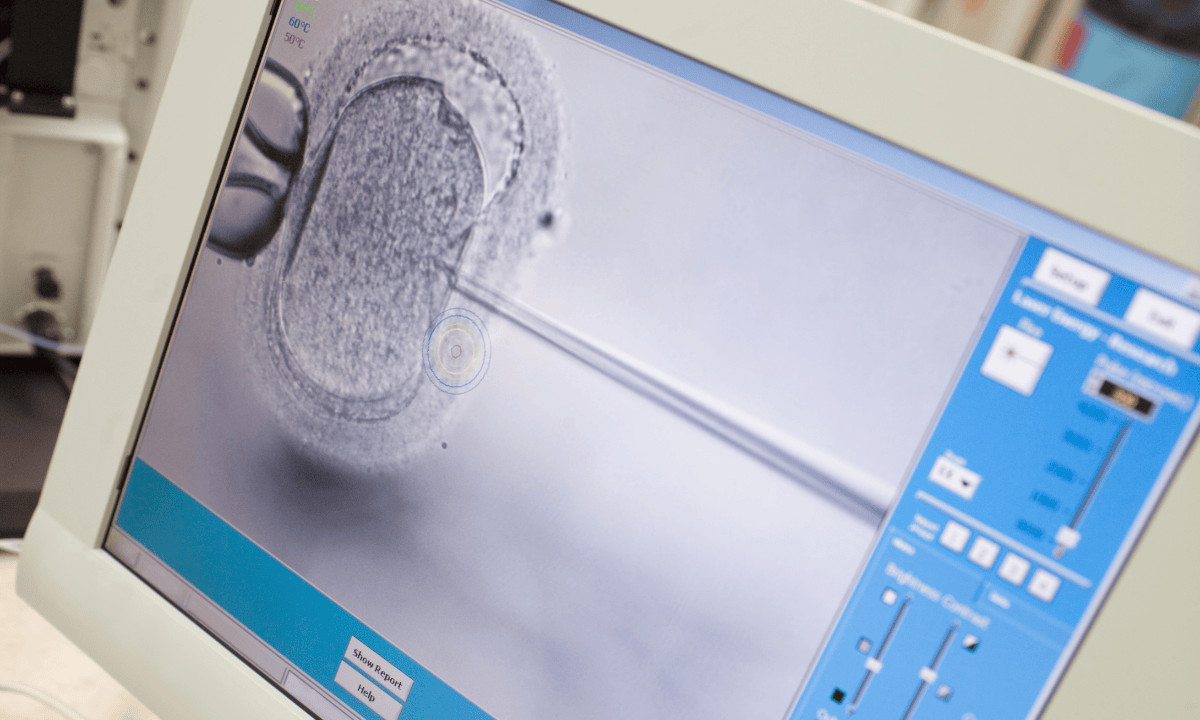
After the final shot of fertility drugs and before your natural ovulation, the eggs are retrieved from the ovaries using a procedure called transvaginal ultrasound-guided aspiration.
During this procedure, a transvaginal ultrasound is performed to direct a thin needle toward the ovaries to retrieve the eggs from the follicles. This process usually lasts 15 to 30 minutes, and anaesthesia is administered to reduce pain.
The embryologist then examines each egg to identify which ones are mature and suitable for fertilisation.
Fertilisation:
There are two common ways to fertilise eggs:
The first one is conventional insemination, where healthy sperm and mature eggs are mixed and kept in a controlled environment called an incubator.
The second procedure involves injecting a single sperm directly into the mature egg, known as intracytoplasmic sperm injection (ICSI). This method is often used for PGT-M to ensure the best possible genetic sample.
Confirming fertilisation:
The morning after fertilisation, the embryologist checks each egg to confirm that fertilisation has occurred successfully.
Embryo development and biopsy:
The fertilised embryos are cultured in a laboratory for five to six days until they develop into blastocysts, which contain approximately 100 to 150 cells.
At this stage, the embryologist will perform a trophectoderm biopsy, where they’ll remove a small sample of cells from the outer layer while leaving the inner cell mass untouched.
Genetic testing:
The biopsied cells are analysed to determine whether the embryo carries a specific genetic condition that you're at risk of passing on.
Embryo selection and transfer:
Once results are available, only embryos that are unaffected by the targeted genetic condition are selected for transfer to your womb. Typically, one embryo is transferred at a time to reduce the risk of multiple pregnancy (twins or more).
The healthy embryo is placed back inside the uterine cavity using a thin, flexible tube (catheter). A successful pregnancy occurs when this embryo implants itself into the uterine wall.
Pregnancy test:
Approximately 10 to 14 days after embryo transfer, you'll take a pregnancy test. A positive result indicates that an embryo has implanted successfully.
If the procedure is successful, your pregnancy should be unaffected by the specific genetic condition that was tested for.
Are you considering PGT-M and wondering if it is suitable for your fertility conditions? Our fertility specialists at Thomson Fertility Singapore are here to help address your concerns. Schedule a consultation today.
How safe is the procedure?
.png?branch=production)
Although the idea of removing cells from embryos can be worrying, PGT-M is generally regarded as a safe and well-established procedure that has been refined over the past three decades to minimise risks. The biopsy is most commonly performed when the embryo has reached the blastocyst stage, usually on the fifth or sixth day after fertilisation.
At this point, the embryo has developed into two parts, the inner cell mass (where the baby will develop) and the outer layer of cells (which will form the placenta). The biopsy only takes place on the outside layer, so the inner cell mass stays the same.
This approach significantly improves safety compared with earlier methods that removed cells from younger embryos.
How much does PGT-M cost in Singapore?
The cost varies depending on whether you are being tested for a common or rare genetic disorder, where you receive treatment and your specific circumstances. A complete PGT-M cycle includes the IVF procedure, an embryo biopsy, laboratory analysis and testing of embryonic cells.
Since 1 July 2022, eligible couples can receive up to 75% government co-funding for PGT-M, subject to caps. For couples where both partners are Singapore citizens, the maximum co-funding per cycle is up to SGD 17,100 for common disorders and up to SGD 31,420 for rare disorders.
Couples where one partner is a Singapore citizen and the other is a permanent resident receive 55% co-funding with lower caps, while couples where one partner is a Singapore citizen and the other is a foreign national receive 35% co-funding. Each couple is eligible for up to six co-funded PGT-M cycles.
In addition to government co-funding, couples can use their MediSave to offset costs. Withdrawals of up to SGD 6,000 are permitted for first-time IVF/PGT-M cycles, with subsequent cycles allowing for SGD 5,000 (for the second cycle) or SGD 4,000 (for the third and subsequent cycles). The lifetime limit for MediSave withdrawals is SGD 15,000 per patient.
The information provided above is intended for general reference only. To learn more about PGT-M co-funding and eligibility, please refer to the Ministry of Health (MOH) website. For a detailed cost breakdown and personalised pricing based on your specific conditions, contact our medical concierge team.
FAQ
Is PGT-A allowed in Singapore?
Preimplantation genetic testing for aneuploidy (PGT-A) is different from preimplantation genetic testing for monogenic disorders (PGT-M). PGT-A screens embryos for random chromosomal abnormalities, such as having an extra or missing chromosome, which become more common as women age.
Currently, PGT-A is not permitted as a routine procedure in Singapore, except in circumstances approved by the Ministry of Health (MOH). PGT-M, on the other hand, is permitted when there is a medical need, such as when either parent has an inherited disorder.
Can PGD be done without IVF?
No, because PGD requires embryos to be created outside the body so that cells can be safely removed and tested in a laboratory. Therefore, PGD can only be performed as part of an IVF cycle. Couples who wish to undergo PGD must first undergo ovarian stimulation, egg retrieval, and fertilisation of their eggs in a laboratory.
How is PGD performed?
After fertilisation, the embryos are cultured in the laboratory for several days until they reach a stage where a biopsy can be performed. An embryologist carefully removes a few cells, typically from the outer layer of a blastocyst (a five- or six-day-old embryo), leaving the rest of the embryo intact.
These cells are analysed using genetic techniques to determine whether the embryo carries the condition being tested for. Only those free of the genetic problem are considered for transfer to the uterus.
What is the purpose of PGD?
The main purpose of PGD is to help couples who are at risk of passing on single-gene genetic conditions to have a healthy child. By testing embryos before conception, couples can select those that are unaffected by the specific inherited condition they carry.
What are the risks of PGD?
PGD is generally considered to be safe. The biopsy process involves removing only a small number of cells, which does not usually affect the embryo's development. However, occasionally, the results may be inconclusive, or the embryos may show mosaicism, which occurs when an embryo contains a mixture of chromosomally normal and abnormal cells.
The emotional and financial aspects of IVF with PGD can also be challenges for some couples undergoing this procedure.
Can you do PGT-M without PGT-A?
Yes. PGT-M and PGT-A are separate tests that serve different purposes. PGT-M specifically tests for the single-gene condition you're at risk of passing on, while PGT-A screens for random chromosomal abnormalities (such as extra or missing chromosomes).
Most couples undergoing PGT-M only need PGT-M testing, as their primary concern is avoiding a specific inherited condition. Additionally, in Singapore, PGT-A is currently not permitted as a routine procedure except under specific MOH-approved circumstances.
Your fertility specialist will advise whether PGT-M alone is sufficient for your situation or if additional testing may be necessary.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your specific fertility conditions or needs, schedule a consultation with our specialists at Thomson Fertility Singapore.
