Have you ever noticed itchy, red bumps appearing on your skin during particularly stressful times? You might be experiencing stress hives. While most people think of hives as an allergic reaction, stress can actually trigger these uncomfortable bumps on your skin. Learning about what stress hives are, how to identify their symptoms, and how to manage them can give you a deeper understanding of your body’s response to stress.
What are stress hives?
Stress hives or urticaria, are red, itchy, raised bumps that suddenly pop up on your skin when you're feeling overwhelmed. Most people associate hives with allergies, but stress alone can trigger them too.
Think of stress hives as your skin reacting to what's happening in your mind and body. When you're anxious or under pressure, your body releases chemicals that can cause these bumps (welts) to appear. Unlike hives triggered by allergic reactions to specific foods or medications, stress-induced hives appear in response to emotional tension rather than external allergens.
How do stress hives occur?
When you're stressed, your body goes into "fight-or-flight" mode. This natural response triggers the release of chemicals, including histamine and the stress hormone cortisol. When histamine is released, it causes tiny blood vessels under your skin to leak fluid into the surrounding tissue. This leakage leads to inflammation, swelling, and the formation of bumps, creating what we recognise as a stress rash.
It's important to note that stress doesn't just trigger new hives but it can also worsen existing hives. Fortunately, stress rashes or stress hives often settle once your stress levels come down.
What triggers stress hives?
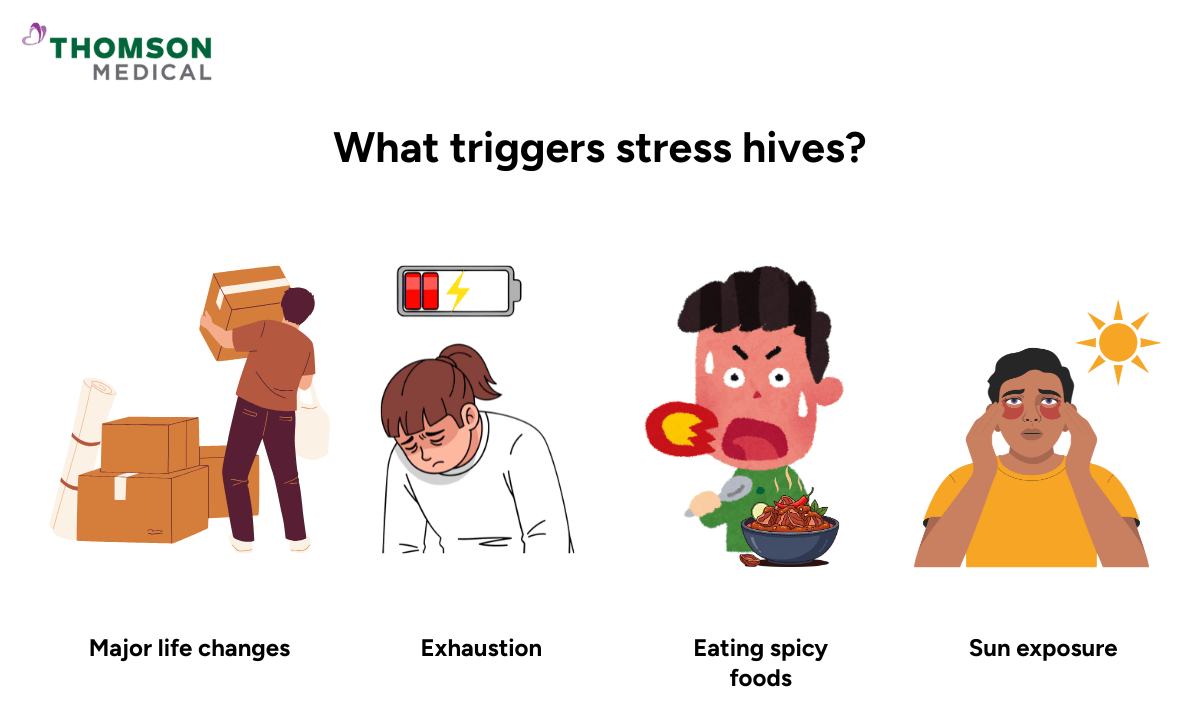
Learning what triggers your stress hives can help you manage and prevent them. Stress triggers the body to release histamine and increases cortisol levels (stress hormones), which makes the immune system more reactive and skin more sensitive.
Here are the main triggers:
Major life changes such as moving house, job changes, or relationship issues
Financial worries and ongoing anxiety
Exhaustion, poor sleep, or fighting an illness
Exercise or physical activity that increases body temperature
Hot showers, saunas, or sun exposure
Eating spicy foods
Tight clothing or physical pressure on the skin
If your hives persist, worsen, or are accompanied by other symptoms, it is important to see a doctor for proper assessment.
Our dermatologist
Loading...
What do stress hives look like?
Stress hives can be uncomfortable and sometimes concerning, but knowing what to look for helps you identify them quickly. Here's what you need to know:
Aspect | Details |
Appearance |
|
Where they appear |
|
How they feel |
|
Duration |
|
Other than the hives, you may notice other signs that your body is feeling stressed. These can include:
Tension headaches
Upset stomach
Difficulty sleeping
General anxiety or feeling overwhelmed
If you're experiencing these symptoms alongside hives, it's an indication that stress may be the underlying trigger.
How are stress hives different from allergy hives?
While stress hives and allergy hives may look very similar, understanding the differences can help you determine what's causing your symptoms.
Allergy hives usually have some clear features:
Triggered by specific allergens, such as certain foods (nuts, shellfish), medications, pollen, or insect stings
Appear within minutes to a few hours after exposure
Come back only if you encounter the same allergen again
May be accompanied by other allergy symptoms, like a runny nose, watery eyes, sneezing, or, in severe cases, difficulty breathing
If you’re unsure whether your hives are caused by stress or an allergy, request an appointment with Thomson Medical. Our specialists can help identify the trigger and recommend the suitable treatment as per your condition.
How can you manage and treat stress hives at home?
Stress hives cause discomfort, but simple home remedies can provide effective relief. Here is what you can do at home to treat hives caused by stress:
Avoid scratching and move to a cooler environment
Apply a cold compress wrapped in a towel for 10 to 20 minutes to reduce redness and swelling
Wear loose, breathable clothing made of cotton that will not rub or irritate your skin
Take over-the-counter antihistamines to reduce itching and swelling
Apply soothing creams like calamine lotion for extra relief
Avoid certain pain relievers such as aspirin or ibuprofen if they make your hives worse
Avoid alcohol when taking antihistamines
Most people notice improvement within a few hours to a few days with these simple steps. Be patient with yourself. Stress hives are your body's natural response to stress and that is completely normal.
How can you prevent stress hives?
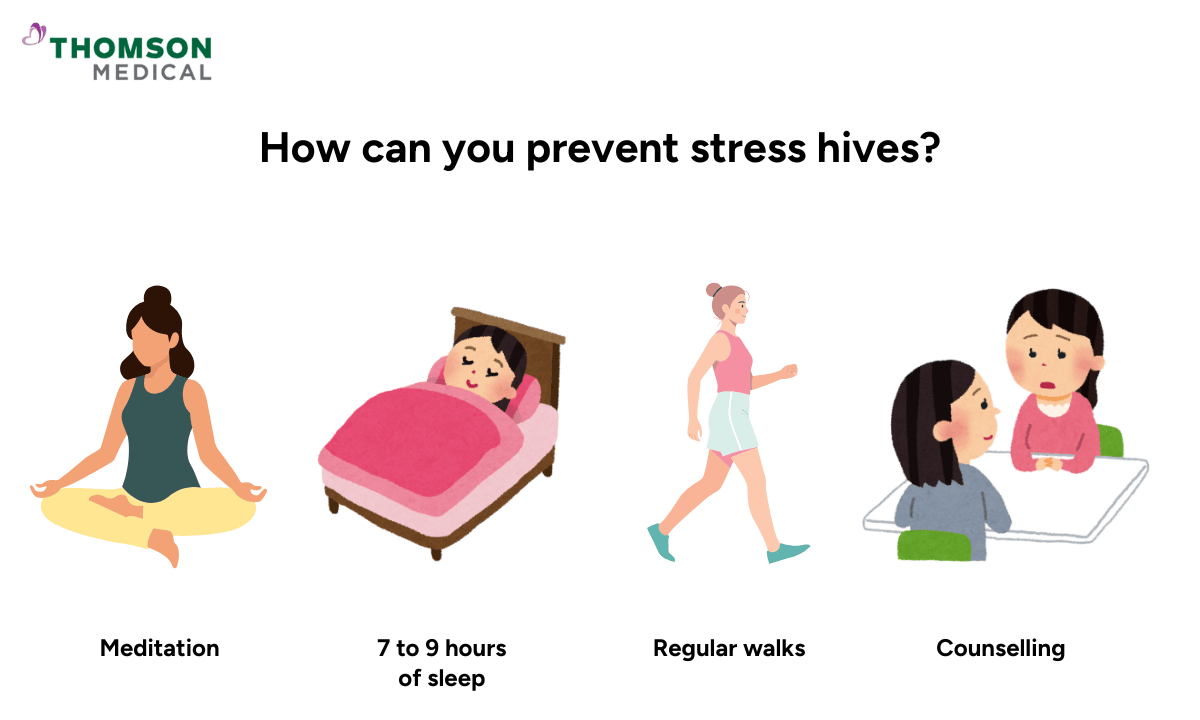
Stress hives are often caused by emotional stress. Luckily, these problems can often be avoided by dealing with stress in the first place and having a healthy lifestyle.
Here are some practical ways to prevent future outbreaks:
Practice stress management techniques such as deep breathing, meditation, or gentle stretching
Maintain healthy habits by getting 7 to 9 hours of sleep, eating balanced meals, staying hydrated, and limiting caffeine and alcohol
Stay physically active with regular walks, swimming, or other gentle exercises you enjoy
Consider counselling, therapy, or support groups if stress feels overwhelming
Talk to friends or family about what you are going through
Remember that managing stress is not always easy, but you have more control than you might think. Be patient and each positive change brings you closer to fewer hives.
When should you see a pharmacist, doctor, or emergency department?
While stress hives are usually manageable at home, there are times when professional help is needed. Knowing when to reach out can give you peace of mind and ensure you get the right care.
Talk to a pharmacist if:
You're not sure which antihistamine to try
You need advice on managing your symptoms
You want to check if you should see a doctor
Visit your doctor if:
Your hives stick around for more than a few days or are getting worse
The treatments you've tried aren't helping
Hives keep coming back regularly
They're affecting your sleep or daily life
You're feeling worried or want some reassurance
Get emergency help right away if you notice:
Swelling around your eyes, lips, tongue, or throat
Trouble breathing or swallowing
Feeling dizzy or faint
Fast heartbeat or chest tightness
These signs could mean a severe allergic reaction that needs immediate attention. This is very rare with stress hives, but it's important to know what to watch for.
If your hives persist, worsen, or are affecting your daily life, request an appointment with Thomson Medical. Our specialists can assess your symptoms, provide effective treatment options, and help you manage stress-related flare-ups safely.
FAQ
How do you know if it's stress hives?
Stress hives usually appear during or right after stressful periods. If you have not been exposed to new foods, medications, or other allergens but are experiencing stress, your hives are likely related to stress. The main indicator is timing, as they’ll show up when you're emotionally overwhelmed or physically exhausted.
How long do hives last due to stress?
A single hive usually lasts between 30 minutes and 24 hours. A stress-related outbreak often lasts a few days to a week, but new hives can keep appearing if stress continues. If your hives last longer than six weeks, it is important to see a healthcare provider, as these symptoms may indicate a condition called chronic urticaria.
What can be mistaken for stress hives?
Several skin conditions, such as heat rash, contact dermatitis, eczema, rosacea, and pityriasis rosea, can look similar to hives. If you're unsure about your skin rash, consult your doctor for proper diagnosis. These skin conditions may present similarly but require different approaches to treatment.
How do you calm down stress hives?
You can take an over-the-counter antihistamine (as per doctor advice) such as loratadine, cetirizine, or fexofenadine to help reduce itching and swelling. Apply a cold compress to the affected areas and stay in a cool, comfortable environment. Wear loose clothing and try not to scratch the hives. Practising deep breathing or other relaxation techniques can also help lower your stress and make your skin feel better.
Why do hives get worse at night?
Hives can feel worse at night for a few reasons. The cells in your skin that release histamine are more active at night, which can make itching and redness stronger. You also notice the itch more when it is quiet and there are fewer distractions. Warmth from your bed or blankets can make your physical hives worse, and stress or anxiety in the evening can trigger flare-ups.
Can stress hives come back?
Yes, stress hives can return when you face new stressful situations. Some people experience flare-ups for months or years, while others have only one-time hives. By managing stress and identifying your triggers, it can help you to reduce future outbreaks. If your hives return frequently, consult a healthcare provider to rule out other causes.
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical.Request an appointment with Thomson Medical today.
Reference:
Tomaszewska, K., Słodka, A., Tarkowski, B., & Zalewska-Janowska, A. (2023). Neuro–Immuno–Psychological aspects of chronic urticaria. Journal of Clinical Medicine, 12(9), 3134. https://doi.org/10.3390/jcm12093134
Dr Tan Hiok Hee
Dermatology (Skin)
Thomson Specialist Skin Centre (Novena Specialist Center)
English, Mandarin
.png%3Fbranch%3Dprod&w=640&q=75)
