Starting your fertility journey can feel overwhelming; it’s like stepping into a whole new world of medical terms and timelines. If you're beginning your assisted reproductive technology (ART) journey, it’s normal to feel a little lost with all the medical terms and procedures being thrown your way.
One phrase you’ll likely come across early on is the “trigger shot”—a simple injection with a powerful purpose.
What is a trigger shot and how does it help in IUI?
A trigger shot is a common part of many IUI (intrauterine insemination) journeys. It’s an injection that contains a hormone called hCG (human chorionic gonadotropin), which helps your body release a mature egg from the ovary, something that naturally happens with a hormone called LH (luteinising hormone).
In a natural cycle, your body handles ovulation on its own. But in fertility treatments like IUI or egg retrieval for in-vitro fertilisation (IVF), timing is everything. That’s where the trigger shot comes in. It allows your doctor to control when ovulation occurs or, in IVF, when to collect the eggs before they are naturally released. Once the shot is given, ovulation typically happens within 36 to 40 hours.
Whether you're ovulating irregularly or using fertility medications to grow ovarian follicles, the trigger shot plays a helpful role in boosting your chances of conception. It takes some of the guesswork out of the process and brings you one step closer to your goal of getting pregnant.
How does the trigger shot work for IUI?
The trigger shot helps your body release a mature egg by mimicking the natural hormone surge that causes ovulation. After the injection, ovulation typically happens within 36 to 40 hours. This timing is key, as it allows your fertility team to schedule the IUI at just the right moment, when the egg is likely to be released and ready to meet the sperm in the fallopian tube.
If you're taking medications like Clomid or letrozole to help your follicles grow, the trigger shot makes sure those mature follicles actually release their eggs. During the cycle, your doctor will usually monitor your follicles using ultrasound, and once the lead follicle reaches around 18 to 22 mm, it's time for the shot. This careful timing gives you the best possible chance of success.
Who might need a trigger shot for IUI?
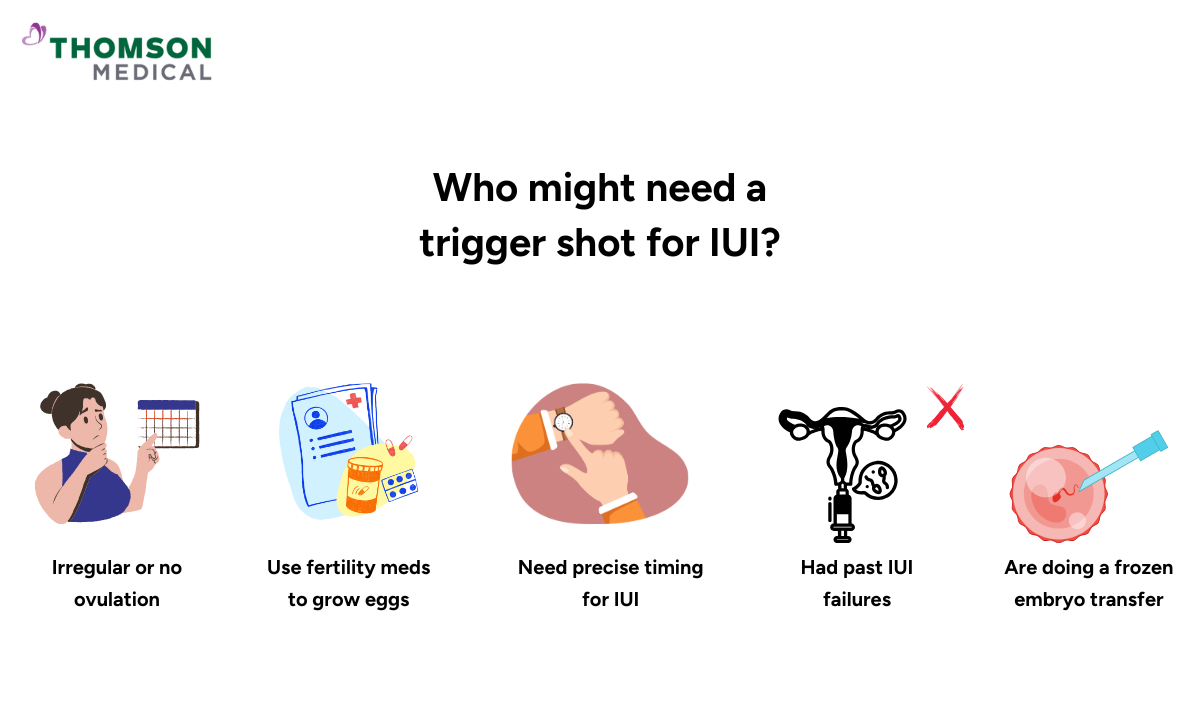
A trigger shot isn’t always necessary, but it’s often used to improve timing and success in certain IUI cycles. You may need one if:
You have irregular or no ovulation (e.g. PCOS)
You're taking fertility meds like Clomid, letrozole, or gonadotropin therapy to grow multiple follicles for IUI
Precise ovulation timing is needed for insemination
You've had previous IUI cycles that were unsuccessful
You're doing a frozen embryo transfer (FET) or other assisted procedures
By helping your doctor time ovulation more accurately, the trigger shot can increase the likelihood of a successful IUI.
Is it better to ovulate naturally or with a trigger shot?
Both natural and triggered ovulation can result in pregnancy, but a trigger shot is often preferred during fertility treatments like IUI because it gives your doctor more control over timing.
Trigger shot advantages:
More predictable ovulation timing, which helps schedule IUI precisely
Ensures the egg is released after using medications like Clomid or letrozole
Reduces the risk of missing the ovulation window
Useful for those with irregular cycles or conditions like PCOS
Natural ovulation advantages:
Fewer medications and a more natural approach
No risk of side effects from fertility drugs
What are the different types of trigger shots?
Trigger shots used in IUI and fertility treatments generally fall into two main categories:
hCG-based trigger shots (Most common):
These mimic the body’s natural LH surge and trigger ovulation within 36 to 40 hours.
GnRH agonist trigger (Less common for IUI):
Used more often in IVF or when there’s a high risk of ovarian hyperstimulation.
Leuprolide acetate (Lupron): Not typically used in standard IUI cycles unless there's a specific medical reason
Have questions about which trigger shot is right for you? Request an appointment with Thomson Medical, and our fertility specialists will recommend the most suitable option based on your cycle and individual health needs.
How is the trigger shot timed?
Timing the trigger shot correctly is one of the most important parts of an IUI cycle. Your doctor will monitor your follicles using ultrasound, and once the lead follicle reaches about 18 to 22 mm in size, which means the egg is mature, they will let you know exactly when to take the shot. The trigger shot is often done in the evening to match your body’s natural rhythm.
Ovulation typically happens 36 to 40 hours after the injection, so IUI is usually scheduled 24 to 36 hours later. This careful timing helps ensure that the sperm is already in the uterus or fallopian tubes when the egg is released, giving you the best possible chance of conception.
Our fertility specialists
Loading...
What to expect when getting a trigger shot?
The trigger shot is usually a quick and simple injection given just under the skin, typically in the lower abdomen or thigh. Most people take it at home, and it feels similar to a flu shot or an insulin jab—brief and relatively painless. If you're unsure about doing it yourself, a nurse or your partner can help with the injection.
Your clinic may ask you to note down the exact time and date you took the shot, as this helps schedule the IUI at the optimal time. After the injection, it’s common to feel mild symptoms like pelvic twinges or cramping, and these are signs that ovulation is on the way.
What are some common side effects or risks of a trigger shot?
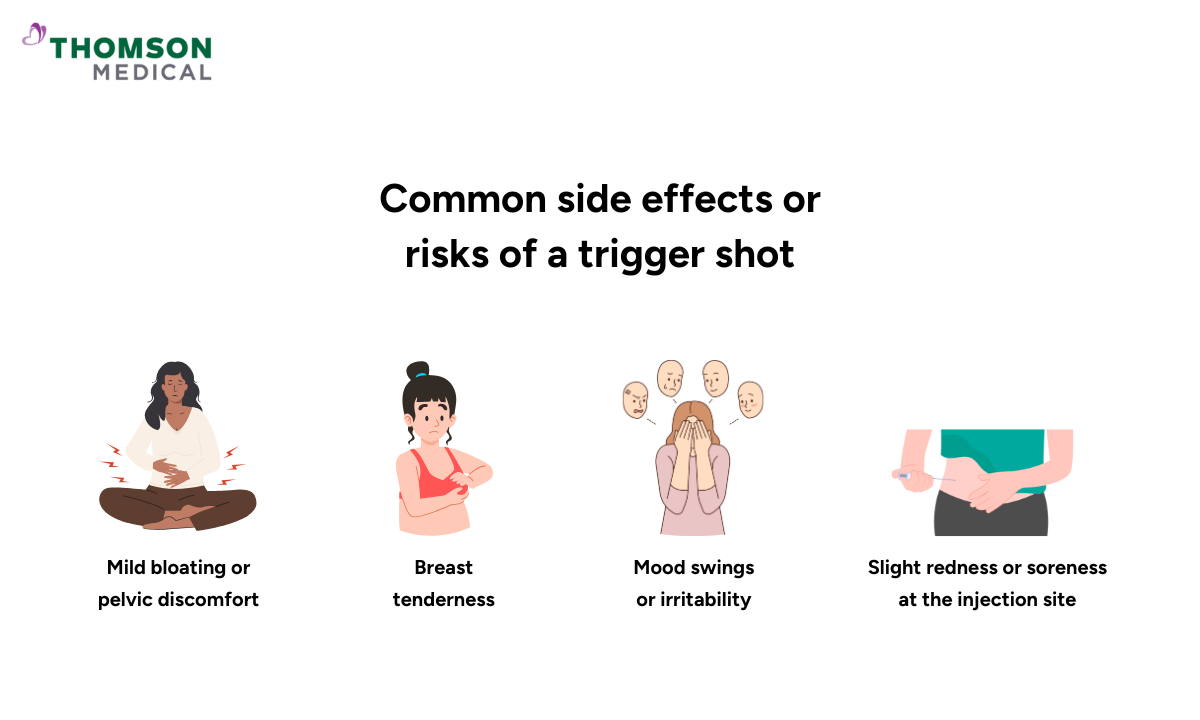
Most people tolerate the trigger shot well, but like any medication, it can cause some side effects. Here's what you might experience:
Common side effects:
Mild bloating or pelvic discomfort
Breast tenderness
Mood swings or irritability
Slight redness or soreness at the injection site
Less common risks:
Ovarian hyperstimulation syndrome (OHSS): Rare in IUI cycles but possible, especially if multiple follicles develop
Multiple pregnancy: If more than one egg is released, there's a higher chance of twins or more
False positive pregnancy test: Since the trigger contains hCG, it can stay in your system for up to 10 days and may cause a false positive pregnancy test if taken too early
Remember, you should always follow your doctor’s instructions and let them know if you have any concerns after the shot.
FAQ
How successful is the trigger shot for IUI?
The trigger shot doesn’t guarantee pregnancy, but it plays a key role in improving the success of IUI by helping time ovulation more precisely. When combined with ovulation induction and proper monitoring, it increases the chances that sperm will meet the egg at the right time.
Successful conception rates vary depending on age, fertility health, and other factors, but with the trigger shot, many IUI cycles see improved outcomes, especially in women with irregular ovulation or timing issues. Your doctor can guide you on how it fits into your overall treatment plan.
How long after a trigger shot do you have an IUI?
IUI is typically done about 24 to 36 hours after the trigger shot. This timing is carefully planned because ovulation usually happens around 36 to 40 hours after the injection. The goal is to make sure the sperm are already in the uterus when the egg is released, giving you the best chance of fertilisation.
Some clinics schedule IUI right at the 36-hour mark, while others may adjust the timing based on your unique situation, like how many follicles you have, the quality of your cervical mucus, or your response to medications. In some cases, your doctor might even recommend two IUIs spaced out over time.
Does an IUI trigger shot hurt?
The trigger shot is usually not very painful. It’s a quick injection under the skin, typically in the abdomen or thigh, and may feel like a small pinch or mild sting, similar to a vaccine. After the shot, some women may notice mild bloating, cramping, or breast tenderness due to the hormone (hCG). Serious pain or allergic reactions are rare.
Do follicles still grow after a trigger shot?
Not significantly. Once the trigger shot is given, the focus shifts from growth to ovulation. The dominant follicle is usually already mature—around 18 to 22 mm—at the time of the injection. While a tiny bit of growth (1–2 mm) may still happen, the main effect of the trigger is to help the egg fully mature and prepare for release, which typically occurs 36 to 40 hours after the shot.
How big should a follicle be before a trigger shot for IUI?
Before giving a trigger shot, your doctor will monitor the size of your follicles using ultrasound. The lead follicle should typically measure between 18 and 22 mm, which is considered mature and ready for ovulation. Once it reaches this size, the trigger shot is given to help the egg fully mature and prepare for release, allowing IUI to be timed for the best chance of success.
What should you avoid after a trigger shot?
To support ovulation and IUI success, avoid the following after a trigger shot:
Taking a pregnancy test too early (can cause false positives)
High-impact exercise or heavy lifting (risk of ovarian torsion)
Unadvised intercourse outside the recommended window
Missing your scheduled IUI appointment
Taking non-approved medications
Always follow your doctor’s timing and instructions closely.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Fertility
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Request an Appointment