Bringing a baby into the world is exciting, but if this is your first time, you might feel unsure about what to expect. Knowing when to go to the hospital for labour and what might happen if things don’t go as planned can help ease your anxiety and allows you to focus on the experience itself.
What are the signs of labour?
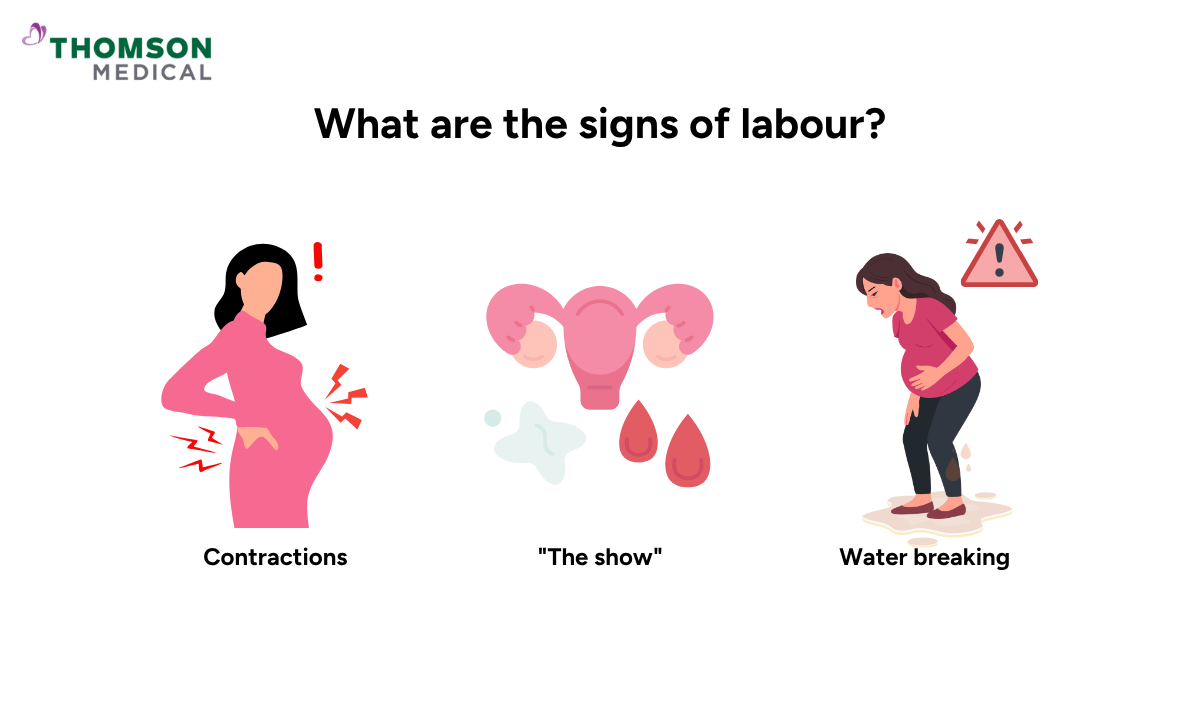
Labour doesn't just happen suddenly. Your body gives you signs that things are starting. Here's what to look out for.
Contractions
Contractions feel like a wave of muscle tightening in your uterus (womb). Some women describe them as period cramps or the sensation of needing to use the toilet. You may also feel low backache with on-off contractions.
Labour often starts with irregular, mild contractions but this is not true labour yet. However, when contractions become more regular, stronger, and closer together, last about a minute each, come every five minutes, and keep going for at least an hour, you're likely in labour.
The duration of labour varies from woman to woman and is often longer for first-time mothers.
"The show"
“The show” in labour refers to thicker vaginal discharge that looks red, brown, or pink. During pregnancy, your cervix is sealed by a mucus or jelly-like plug that protects your baby from infection. As labour approaches, your cervix (the opening to the womb) begins to soften, thin out, and dilate.
Water breaking
Water breaking feels like a gush or trickle of fluid from your vagina. This happens when the amniotic sac (also called the water bag) that surrounds and cushions your baby ruptures. The fluid is often clear or slightly cloudy in colour.
Water breaking is not painful, but you should go to the hospital once this happens, even if contractions haven't started yet, as there is an increased risk of infection once the amniotic sac ruptures. After water breaks, contractions often intensify.
How can you tell the difference between true and false labour?
Not every contraction means labour has started. Here's how to tell the difference:
| False labour (Braxton-Hicks) | Real labour |
|---|---|
Irregular timing | Regular intervals that get closer together |
Mild intensity | Strong and getting stronger over time |
Stop with rest, water, or position change | Persists even when you rest or change positions |
Don't cause cervical changes | Cause your cervix to thin and open |
Can begin weeks before delivery | Signal that labour is starting |
If you’re ever unsure whether your contractions mean labour has started, it’s always best to check in with a doctor. At Thomson Women’s Clinic, our obstetrician and gynaecologist (O&G) specialists can assess your symptoms, provide reassurance, and guide you safely through this important stage.
When is it time to go to the hospital for labour?
Once you recognise the signs of labour, timing your hospital visit correctly is important. You should go to the hospital if you experience:
Stronger, regular contractions that last for 60 seconds and occur every 5 minutes for one hour or longer
Water breaking, even if contractions haven't started
"The show" accompanied by regular contractions
Reduced baby movements (less movement than usual)
Heavy bleeding
Severe abdominal pain
If you're a first-time parent, you can follow the 3-2-1 rule, consistent contractions every 3-5 minutes, for 2 hours, lasting 1 minute or more. This indicates you're in active labour.
What to bring to the hospital?

When you're heading to the hospital for labour, here are some essentials to pack in your hospital bag:
What to pack for yourself?
Comfort items:
Loose, comfortable clothing (nightgown or large T-shirt)
Slippers or sandals
Warm socks
Nursing bra and breast pads (if breastfeeding)
Pillow from home
Music player or phone for entertainment
Birth plan and antenatal notes
Personal toiletries:
Toothbrush, toothpaste, shampoo, soap, deodorant
Lip balm, lotion
Hairbrush, hair ties
Facecloths and spray bottle (for cooling)
Food and drink:
Snacks (energy bars, crackers)
Drinks (water, isotonic drinks)
Other essentials:
Phone, and charger or powerbank
Any medications you're taking
What to pack for your baby?
Going-home outfit
Swaddles or blankets
Hats or mittens
What to expect during labour and delivery?
Labour is the process through which you deliver your baby through the birth canal, followed by the delivery of the placenta. When you arrive at the hospital, your healthcare team will be ready to support you through each stage.
What will happen when you arrive?
Your doctor or nurse will perform a series of assessments to monitor your labour progress and the well-being of both you and your baby. These include:
Checking your vital signs (blood pressure, pulse, temperature)
Monitoring foetal heart rate
Checking cervical dilation
Using cardiotocography (CTG scan) to assess uterine contractions and your baby's heart rate simultaneously
Depending on your stage and progress, various interventions may be considered such as pain management, intravenous fluids, or even a caesarean section if needed.
Stages of labour
Labour is divided into three stages, each with different characteristics.
Stage 1a: Early phase of labour
The early phase, also called the latent phase, is when your cervix thins and begins to dilate to 3-4 cm. This phase is marked by mild, irregular contractions that can last for hours or even days. You may experience the "show" and a sense of pressure in your lower abdomen or back.
What helps during early labour:
Rest as much as possible
Keep yourself hydrated
Take a warm shower, have light snacks, or try gentle massage
Stay active by walking around and changing positions
Stage 1b: Active phase of labour
Active labour typically begins when your cervix reaches 4-6 cm dilation and brings more intense and regular contractions that lead to faster cervical dilation. Your cervix continues to dilate to 10 cm, with stronger and more frequent contractions occurring every 3-5 minutes, lasting 45 to 90 seconds. This is when you should head to the hospital for delivery preparation.
Stage 2: Delivery (expulsion)
Stage 2 begins when your cervix is fully open (about 10 cm) and ends with the delivery of your baby. Strong uterine contractions combine with your efforts to push the baby out. This stage varies in length. It's often longer for first-time mothers and those with epidurals. Your doctor or midwife will guide you on how and when to push.
You may feel burning or stretching as your baby's head comes through. Once the shoulders and body follow, your baby will be placed on your chest for skin-to-skin contact, helping with bonding and keeping your baby warm.
Stage 3: Delivery of the placenta
After your baby is born, your uterus continues to contract, separating the placenta (the organ that gives the nutrients to your baby during pregnancy) from the wall of your womb. This stage lasts from 5-30 minutes, though it can sometimes extend to an hour. The placenta may be delivered spontaneously or managed actively with medication and controlled cord traction.
Your healthcare provider will monitor you closely to prevent complications like excessive bleeding after birth (postpartum haemorrhage).
Our fertility specialists
Loading...
What happens during a caesarean section?
You may need an emergency caesarean section (C-section) if you or your baby are at risk during labour. For example, if labour stops progressing or your baby shows signs of distress. A planned C-section may be needed if you have a serious medical condition, or if there are pregnancy complications.
The procedure:
You'll be awake with spinal or epidural anaesthesia. You'll feel pressure but no pain, and you can hold your baby right after birth. General anaesthesia (being put to sleep) is only used if the C-section needs to be done very urgently.
Your doctor makes a horizontal cut below your bikini line. The scar can be hidden by clothing, and this approach has a lower risk of complications in future pregnancies. Vertical incisions are rare but sometimes necessary.
Recovery from a C-section typically takes around 6 to 8 weeks, though this varies from person to person, with temporary restrictions on lifting and driving.
Types of pain relief during labour
There are non-medical and medical options for pain relief during labour.
Non-medical pain relief
Breathing exercises
Massage
Movement and position changes
Water immersion
TENS (Transcutaneous Electrical Nerve Stimulation)
TENS is a device that produces mild electric current to stimulate your nerves. Your healthcare provider will tape electrode pads on your back, connecting to a small battery-operated stimulator. The current stimulates the production of endorphins, your natural pain-relieving hormones. It's easy to use but takes 30 minutes to take effect and isn't as effective when contractions become longer and more intense during active labour.
Medical pain relief
Nitrous oxide:
Nitrous oxide is also referred to as laughing gas. It's mixed with oxygen and given through a face mask or tube held in your mouth. Nitrous oxide doesn't stop pain entirely, but it can make contractions feel easier to handle.
It doesn't interfere with labour or harm you or your baby's body. Possible side effects include nausea, disorientation, or a claustrophobic feeling from the mask.
Epidural analgesia:
Epidural analgesia is the most effective pain relief, used for both vaginal births and caesarean sections. The medication is injected into the lining of your spinal cord through your back, making you feel numb from the waist down.
Possible side effects include a drop in blood pressure, muscle weakness in the legs, and potentially a longer second stage of labour.
Opioids:
Pethidine is a pain reliever that is injected into the muscle of the buttocks. Its effects last between 2-4 hours. Possible side effects include dizziness, nausea, disorientation, and in severe cases, respiratory depression.
It's important to discuss the potential benefits and risks of each method with your healthcare provider before making a decision.
Post-labour care and support
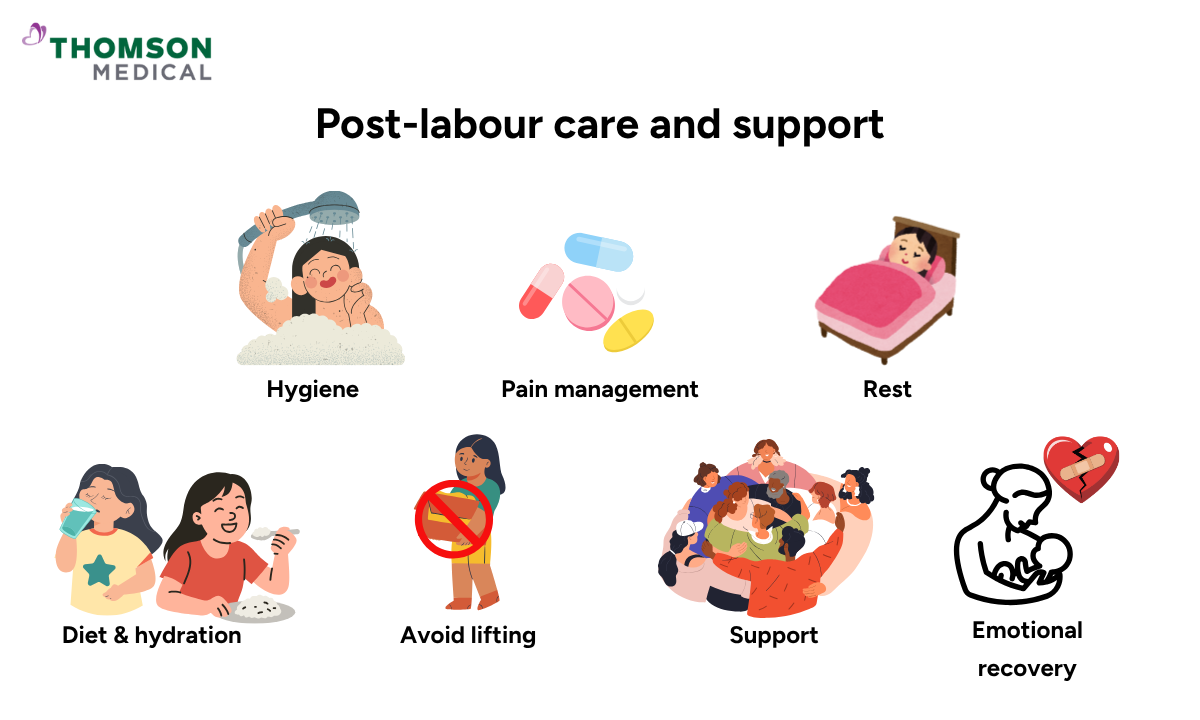
After birth, caring for yourself is just as important as caring for your baby. Here are some practical ways to help your body heal.
Hygiene:
Gently wash the perineal area with warm water (if applicable).
Pain management:
Over-the-counter pain relievers, ice packs, and sitz baths can help manage perineal pain and discomfort. These can also reduce pain from a caesarean section. If you experience significant pain that medication doesn't relieve, contact your doctor.
Get enough rest:
While uninterrupted sleep might seem impossible in the first few months, try sleeping whenever your baby sleeps. It's okay to leave household chores undone if you're exhausted from caring for your newborn.
Healthy diet and hydration:
A well-balanced diet with protein, fibre, and healthy fats will help you recover quicker. Staying hydrated is crucial, especially while breastfeeding.
Avoid lifting heavy objects:
If you've had a C-section, lifting heavy objects can strain your abdomen and uterus. Avoid doing so until your doctor gives you the go-ahead.
Seek support:
Caring for a newborn while your body heals is no easy task. Reach out to friends and family for support. Having additional help with household tasks allows you and your partner to focus on your well-being and your baby's needs.
Emotional recovery:
Labour is physically demanding and emotionally intense. Some mothers feel instant joy, while others feel tired, anxious, or overwhelmed. All these responses are normal.
If you feel persistently low, tearful, or disconnected from your baby after the first few weeks, schedule an appointment with Thomson Women’s Clinic. Our obstetrician and gynaecologist (O&G) specialists understand your concerns and can provide supportive, personalised care to help you feel at ease.
FAQ
How do you know when to go to the hospital when in labour?
You should go to the hospital if you experience stronger, regular contractions lasting 60 seconds and occurring every 5 minutes for one hour or longer, water breaking, or "show."
What is the 3-2-1 rule for labour?
If you're a first-time parent, follow the 3-2-1 rule, consistent contractions every 3-5 minutes, for 2 hours, lasting 1 minute or more. This indicates you're in an active labour.
What are the 10 danger signs during labour?
Seek immediate medical attention if you experience excessive vaginal bleeding, severe headache, convulsions, high fever, prolonged labour (over 12 hours), retained placenta, severe abdominal pain, fast or difficult breathing, baby's head not engaged or coming first, or problems with urination.
How many cm dilated to go to the hospital?
When you're 4-6 centimetres dilated, it's a good time to head to the hospital. This is when active labour begins. However, discuss with your doctor as they may recommend going in earlier or later based on your circumstances.
What if I'm 4 cm dilated but have no contractions?
It's not unusual to be 4 cm dilated without contractions, especially in late pregnancy. It simply means your cervix has begun to open, but active labour isn't necessarily imminent. Many women experience cervical dilation days or weeks before labour begins.
How to dilate faster from 2 cm at home?
There's no guaranteed way to rapidly dilate from 2 cm at home. However, gentle movement (walking or using a birthing ball), nipple stimulation, and relaxation techniques like warm baths can potentially encourage dilation and support labour progression.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
