Seeing rough, red patches appear on your baby's once-smooth skin can be unsettling. You might wonder whether it's something they ate, something they touched, or simply a normal part of growing up.
Baby eczema is common in infants, though the triggers and severity can differ from child to child. Knowing what to look for and when to seek help can make it easier to care for your baby with confidence.
What is baby eczema?
Eczema is a skin condition that makes the skin dry, itchy, and sometimes rashy. It’s common in babies under five. While it can look worrying, eczema is not contagious. Your baby can’t catch it from other children, and they won’t pass it to others either.
Eczema often becomes milder as children grow, and around 40% improve after puberty. If eczema starts early (before 6 months of age) and is more severe, symptoms may last longer. However, eczema can be managed, and with the right approach, you can help keep your baby comfortable.
Why does eczema happen?
If your baby has eczema, you’re probably wondering why. Eczema often runs in families. If you or your partner have eczema, asthma, or hay fever, your baby may be more likely to have sensitive skin too.
These conditions are linked to a more sensitive immune system. Your baby may have inherited genes that make their immune system more reactive. Because of this, their skin doesn’t hold moisture properly, which can lead to dryness and irritation.
What triggers eczema flare-ups?
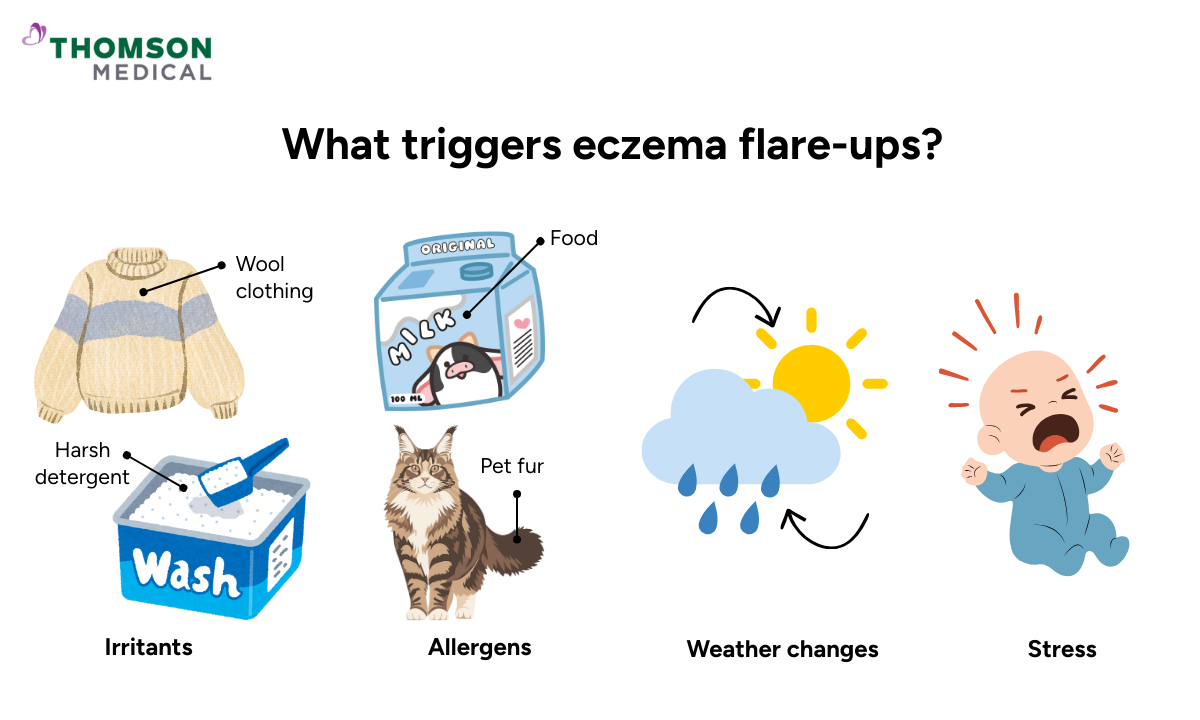
While genetics play a role in whether your baby develops eczema, certain triggers can cause eczema flare-ups even when it seems under control.
Common triggers include:
Irritants such as wool clothing, harsh detergents, or very hot or cold temperatures
Allergens including certain foods, pet fur, or dust
Weather changes, particularly cold, dry winter air or, hot, humid summer conditions
Stress or changes in routine, even in young babies
For example, your child with eczema may feel uncomfortable when going from the warm outdoors into cold, air-conditioned rooms. The sudden temperature changes can dry out their skin and make it itchy or irritated.
If you notice your baby’s eczema worsening or reacting to certain triggers, request an appointment with Thomson Paediatric Centre. Our specialists can help identify specific triggers and recommend personalised skincare to keep your baby’s skin comfortable.
What does eczema look like in babies?
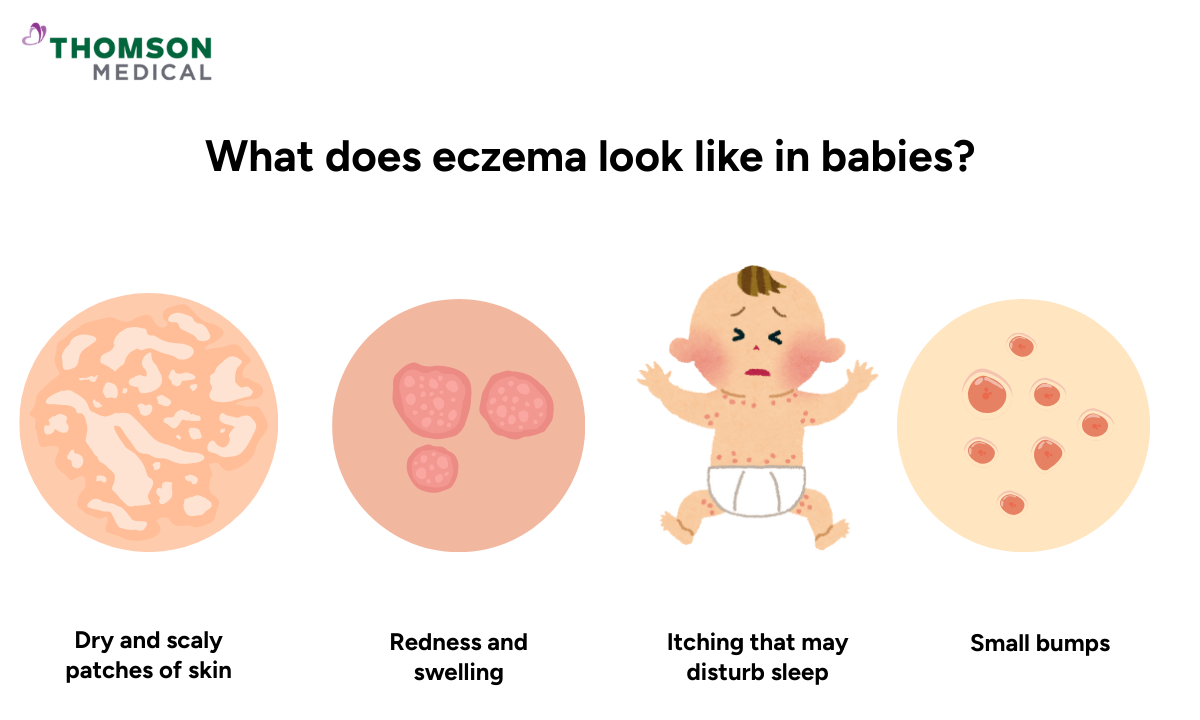
Eczema doesn't look the same on every baby, which can make it harder to recognise at first. However, there are common patterns that can help you identify it.
Common signs include:
- Dry and scaly patches of skin
- Redness and swelling
- Itching that may disturb sleep
- Small bumps that may weep or crust when scratched
You may notice your baby’s eczema most often appearing on their face, the outside of their elbows, and their knees. As your child grows, it can show up more on their hands, feet, arms, and behind their knees.
Keep in mind that not all dry skin is eczema. Cold weather, heating, air conditioning and even swimming can cause dry patches on any baby's skin.
Our paediatricians in Singapore
Loading...
How is eczema diagnosed?
If you've noticed these signs on your baby's skin, getting advice from your doctor can help you manage their eczema.
Your doctor diagnoses eczema through a simple skin examination. They will look at your child's skin and ask about their symptoms and family history of eczema or allergies.
Sometimes eczema symptoms can look similar to other skin conditions. Your doctor may want to rule out other possibilities before confirming the diagnosis.
Are allergy tests needed?
In most cases, allergy tests are not necessary for diagnosing baby eczema.
However, your doctor may suggest testing if your baby's rash covers a large area of their body or if they have digestive problems. Poor weight gain or difficulty digesting milk might suggest a cow's milk allergy, which can sometimes be linked to eczema.
Your doctor may suggest testing if:
Your baby’s rash is widespread, or they have trouble gaining weight or digesting milk. These can be signs of a cow’s milk allergy, which is sometimes linked to eczema
A milk allergy is confirmed. Your doctor will suggest a suitable formula to make sure your baby gets the right nutrition
Allergy tests come back normal. This is a good sign, as food is unlikely to be the cause
Your attention can stay on consistent skincare and following the treatment plan.
How to manage your baby's eczema
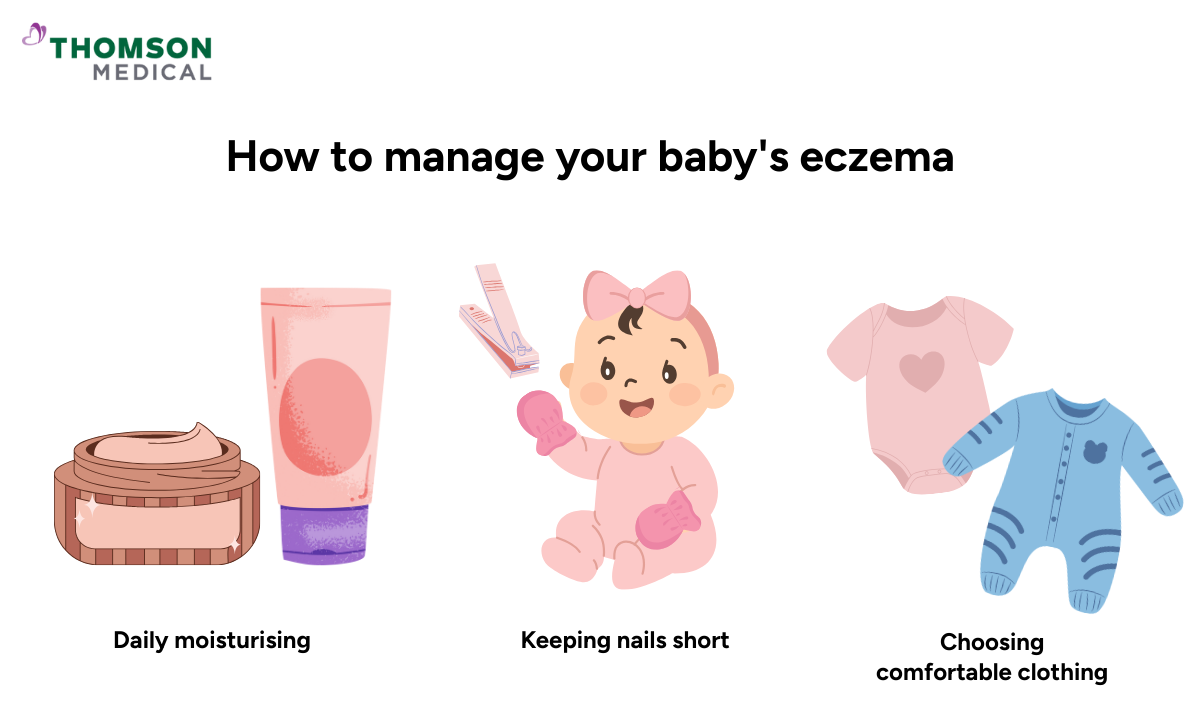
Once your doctor has confirmed eczema, the focus shifts to managing it effectively. There is no cure for eczema, but you can manage it effectively with a consistent treatment plan.
Daily moisturising
Emollients are moisturising products that soften and protect your baby's skin. They create a protective barrier over your little one's faulty skin barrier, preventing moisture loss and blocking irritants.
You can apply emollients generously and often, especially after bathing while your baby's skin is still slightly damp. By doing so, their skin can often be more moisturised and become less itchy
Keeping nails short
Your baby can often scratch itchy areas, which can further irritate their skin and lead to infection. Keeping your child's nails short and smooth can help prevent this.
Some parents find soft cotton mittens helpful. Wearing mittens stops your baby from scratching while they sleep. This is helpful because itching is often worse at night, when babies are harder to settle. Keeping their hands covered helps protect the skin and lowers the chance of it getting sore or infected.
Choosing comfortable clothing
The clothes your baby wears can make a real difference to their comfort. Soft, breathable fabrics are gentlest on sensitive skin.
Good clothing choices include:
Organic cotton grown without harsh chemicals, making it gentle for everyday wear
Bamboo fabric that wicks moisture away from the skin
Silk that feels smooth and soft against delicate skin
Fabrics to avoid:
Wool, which can feel scratchy and irritating
Synthetic materials like polyester and nylon, which are less breathable and can trap heat and moisture against the skin
Wash new clothes before your baby wears them to remove any manufacturing residues. Use gentle, fragrance-free detergents and avoid fabric softeners.
Does your baby's eczema need medication?
Most of the time, eczema can be managed with regular moisturising and gentle skin care. However, when your baby’s skin becomes very itchy or inflamed, medication may help the skin settle.
Steroid creams when needed
You might feel worried about using steroid creams on your baby's delicate skin. Many parents share this concern, especially with information about steroids circulating online.
When used appropriately and as prescribed, topical steroid creams are safe and effective for managing eczema flare-ups. Your doctor will recommend the right amount for each area. Mild steroids work for gentle areas like the face, while stronger steroids are needed for severe flare-ups on thicker skin areas like hands and feet.
These creams reduce inflammation and work when used exactly as your doctor prescribes.
When antibiotics might help
Eczema-affected skin can sometimes become infected with bacteria. If your doctor suspects an infection, they may prescribe antibiotics to clear the bacteria and improve the eczema.
Your baby having infections doesn't mean you've done anything wrong. Eczema skin has a weakened barrier that makes it more vulnerable to bacteria, even with excellent care.
When to see your doctor
Knowing when eczema needs professional attention versus when you can manage it at home can feel unclear, especially when you're learning what's normal for your baby.
Contact your doctor if:
The eczema is not improving with regular moisturising
Your baby seems distressed or cannot sleep due to itching
The skin looks infected with increased redness, warmth, swelling or weeping
You are unsure about how to use prescribed treatments
The eczema is affecting your baby's feeding or general wellbeing
Managing eczema can feel overwhelming at first, but with a consistent routine, it often becomes easier within a few weeks. You’ll start to notice what works for your baby’s skin, and small adjustments can make a difference.
If your baby’s eczema isn’t improving or is affecting their comfort and wellbeing, request an appointment with Thomson Paediatric Centre. Our paediatric dermatologists can assess your baby, adjust treatments, and guide you on effective skincare routines tailored to your baby.
FAQ
How can I tell baby eczema from baby acne?
Baby acne usually causes small pimples on the face. Eczema rash appears as dry, red, itchy patches, sometimes on the cheeks, arms, or legs.
Can germs make eczema worse?
Yes. Bacteria, the cold sore virus, or dirty surfaces can make your baby’s eczema worse. Keep your baby’s skin clean and watch for signs of infection.
Can a food allergy cause eczema?
Sometimes, certain foods can make eczema worse. Cow’s milk is the most common trigger in babies, but other foods can also affect your baby’s skin. If your baby has eczema along with vomiting, diarrhoea, or poor weight gain, your doctor may suggest checking for a food allergy.
How soon will treatment help?
You may see improvements within a few days, but full healing can take several weeks. Consistency with moisturisers and prescribed creams matters.
Will eczema go away as my baby grows?
Eczema often improves as your child gets older, but sensitive skin may remain. Most children outgrow severe flare-ups by school age.
Why does my baby’s eczema flare up after swimming?
Eczema can get worse after swimming because chlorinated water or hot water can dry out your baby’s skin. Salt or pool chemicals can also irritate sensitive skin. To help prevent flare-ups:
- Give your baby a lukewarm bath right after swimming
- Gently pat the skin dry
- Apply moisturiser or emollient balm within a few minutes to lock in moisture
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice for your little one's skin conditions, request an appointment with Thomson Paediatric Centre today.
Reference:
Chovatiya, R., & Silverberg, J. I. (2022). Evaluating the longitudinal Course of Atopic dermatitis: Implications for Clinical practice. American Journal of Clinical Dermatology, 23(4), 459–468. https://doi.org/10.1007/s40257-022-00697-w
