When facing concerns about ovarian health, one common question is “Can MRI detect ovarian cancer?”
Magnetic Resonance Imaging (MRI) is an essential tool in evaluating ovarian masses, offering a level of detail that goes beyond ultrasound. It helps your doctor distinguish between benign cysts and malignant tumours, assess how far cancer may have spread, and guide treatment decisions with greater precision.
While MRI isn’t usually the first test performed, it plays a crucial role when your ultrasound results are unclear or when your doctor needs more detailed imaging for diagnosis or surgical planning.
Can MRI detect ovarian cancer?
If your ultrasound shows unclear findings on the ovaries, your doctor may recommend further testing, such as an MRI scan. An MRI can detect ovarian cancer and help distinguish between benign and cancerous tumours.
Although MRI is not the first test doctors use – ultrasound usually comes first – it provides several important advantages:
No radiation exposure (uses magnetic fields and radio waves)
Greater specificity than ultrasound in diagnosing cancer
Detailed images of internal structure and tissue composition
Better accuracy in identifying benign masses, potentially avoiding unnecessary surgery
How does MRI work to identify ovarian masses?
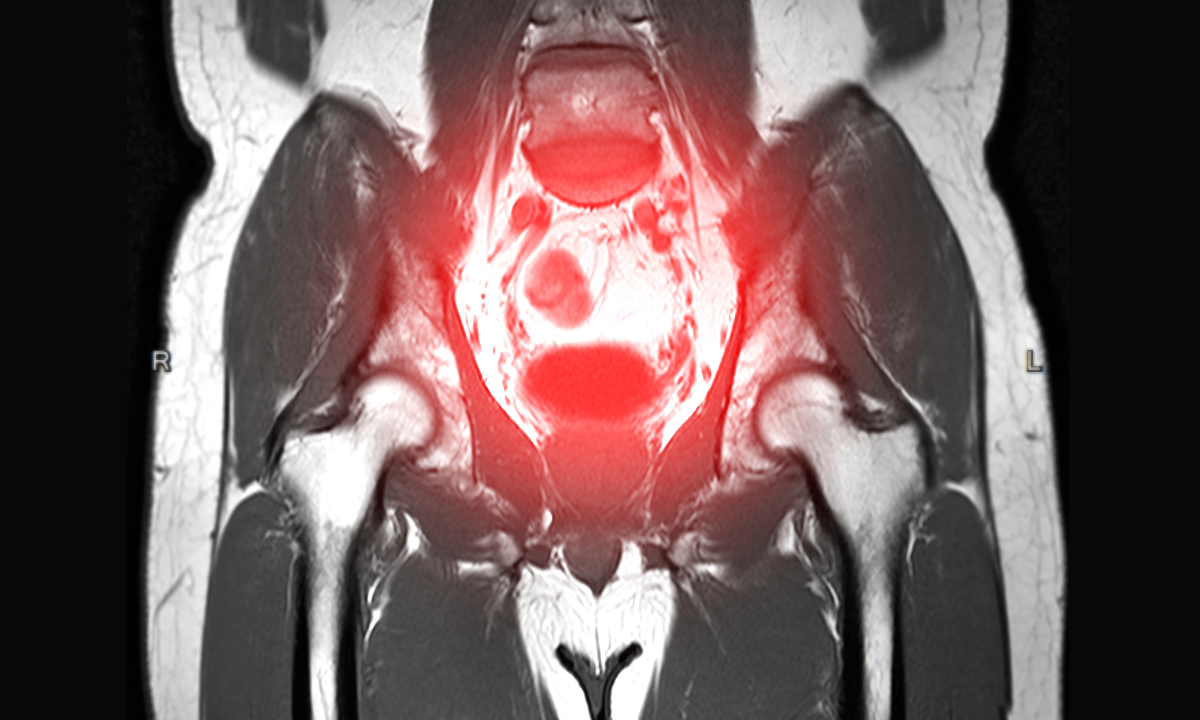
MRI uses strong magnets and radio waves to create highly detailed images of the pelvic area. This helps your doctor see soft tissues clearly and identify whether an ovarian mass is likely benign or cancerous. MRI is especially good at distinguishing between dermoid cysts, endometriotic cysts, and fibroids, which can sometimes appear suspicious on ultrasound.
It provides information not only about the size and shape of a mass but also its internal structure and composition.
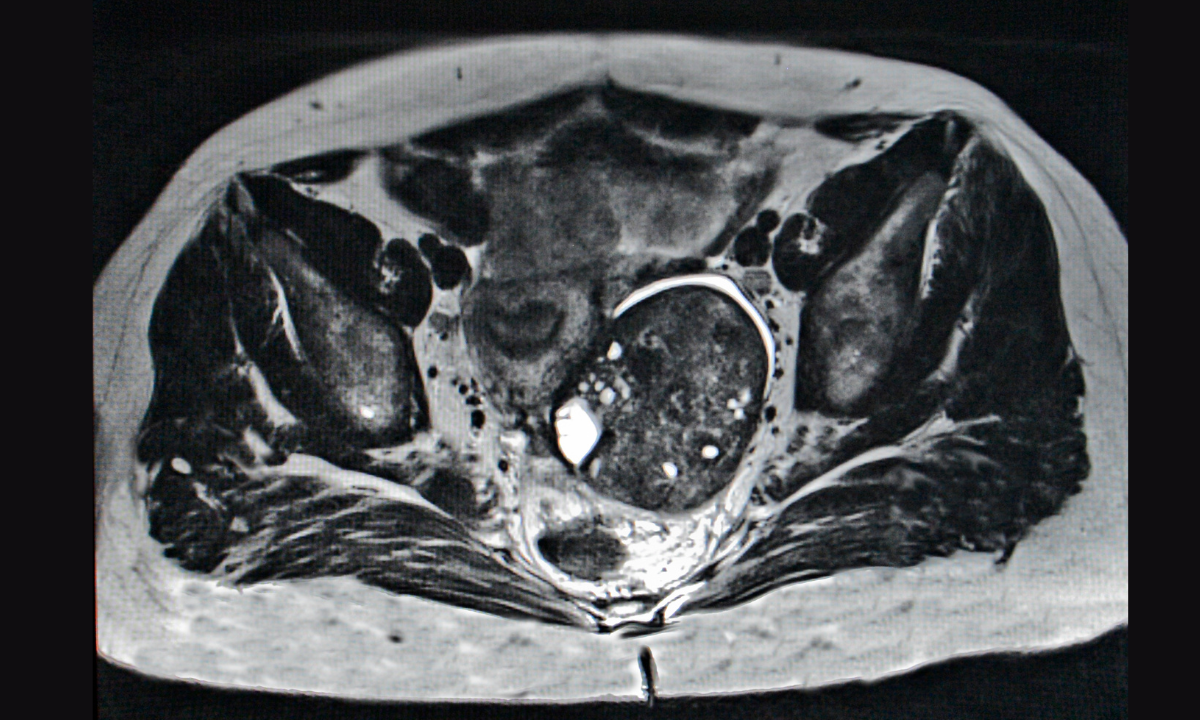
Types of MRI images used
Your MRI scan uses several imaging techniques to build a complete picture:
T1-weighted images:
Show fat or blood inside a mass.
T2-weighted images:
Highlight internal structures and fluid content.
Contrast-enhanced images:
Use a contrast dye to make details like nodules and dividing walls easier to see.
Diffusion-weighted imaging (DWI):
Tracks how water moves within tissues to help detect abnormal cell growth.
MRI vs ultrasound for detecting ovarian cancer
You might be wondering why your doctor is suggesting an MRI when you've already had an ultrasound. Each test provides different information that helps doctors make a clearer diagnosis. Key differences between MRI and ultrasound:
Sensitivity:
Both tests are good at detecting potential cancerous masses.
Specificity:
MRI is better at distinguishing between cancerous and non-cancerous (benign) masses.
Accuracy:
An MRI can more accurately identify benign conditions such as dermoid cysts, endometriotic cysts, and fibroids, which may look suspicious on ultrasound.
Because of this higher accuracy, MRI scans for cancer can often confirm when a mass is benign, helping many patients avoid unnecessary surgery and the stress of uncertain results.
If you’re concerned about your ovarian health or have been advised to undergo further imaging, schedule an appointment with Thomson Medical. Our specialists can help guide you through the next steps.
Our women's cancer specialist
Loading...
When doctors use MRI for ovarian cancer diagnosis
Ultrasound is usually the first test for evaluating your ovarian problems, but MRI is often used when the ultrasound results are unclear or more detailed images are needed before surgery. However, your doctor may recommend an MRI in certain cases, such as when:
Ultrasound results are unclear and could suggest either a benign or cancerous mass
You are young and fertility preservation is a concern
More detailed imaging is needed before surgery
Surgeons need to see how the mass relates to nearby organs for surgical planning
What can an MRI show about ovarian cancer?
MRI offers more detailed information than an ultrasound. It produces clear images that help doctors assess the nature of an ovarian mass and see if the cancer has spread beyond the ovaries.
Distinguishing benign from cancerous masses
One of MRI’s key strengths is helping doctors tell the difference between harmless (benign) and cancerous ovarian masses. It produces highly detailed images that allows your radiologist to spot subtle differences between conditions such as ovarian cysts, ovarian cancer, and other similar growths.
MRI can also identify several non-cancerous conditions that may appear suspicious on ultrasound, including:
Dermoid cysts (contain fat or hair)
Endometriotic cysts (contain old blood)
Fibroids (benign muscle tumors)
Functional cysts (fluid-filled sacs)
The scan shows details about the tissue structure and whether the mass is solid or fluid-filled. For instance, functional cysts typically appear as fluid-filled areas with little to no solid tissue. These distinctions help your doctor decide whether surgery or simple monitoring is the best approach.
Detecting cancer spread and staging
If cancer is present, MRI plays an important role in showing how far it has spread. It’s currently one of the most accurate imaging tools for evaluating cancer spread in the abdomen, which is crucial for treatment planning.
MRI can detect cancer spread to:
The peritoneum (lining of the abdomen)
Nearby organs like the bladder, uterus, or rectum
Lymph nodes in the pelvis and abdomen
The omentum (fatty tissue covering intestines)
Overall, MRI offers higher accuracy than many other imaging tests for detecting abdominal cancer spread. This detailed information helps your doctor determine whether surgery is possible or if chemotherapy should be done first to shrink the cancer.
Limitations of MRI for ovarian cancer detection
While MRI is a powerful imaging tool, it's important to understand its limitations. The accuracy can vary depending on where you have your scan and who reads the results, especially outside specialised medical centres.
Practical limitations include:
Cost and accessibility:
MRI has a relatively high cost and lower availability compared to ultrasound, making it less practical as a first-line test
Longer examination time:
MRI takes longer to perform than CT, increasing the chance of movement during the scan, which can affect image clarity.
Detection challenges:
MRI may have difficulty detecting very small tumour spots in your abdomen, which can be important for accurate staging
Contrast limitations:
MRI may not clearly show the bowel, which can make it harder to assess certain areas of your abdomen.
Most hospitals still use CT scans to stage ovarian cancer. CT is faster, more widely available, and well-established for treatment planning. MRI serves as a valuable complement to CT in specific situations rather than a complete replacement.
If you’re unsure which imaging test suits your situation best, request an appointment with Thomson Medical. Our doctors can guide you through your options and ensure you get the most accurate diagnosis.
FAQ
Is MRI the first test for ovarian cancer?
No. MRI is not usually the first test used to check for ovarian cancer. Your doctor typically start with an ultrasound because it’s easier to access, more affordable, and quicker to perform. MRI is used when:
Ultrasound results are unclear
More detailed information is needed before deciding on treatment
The patient is young and wants to preserve fertility
Doctors need precise details for surgical planning
Can MRI miss ovarian cancer?
Yes, MRI can sometimes miss ovarian cancer. In community settings, scans suggesting cancer may turn out to be benign. This is why your doctor relies on several tests – such as blood tests, imaging, and sometimes a surgical biopsy – to make a clear diagnosis.
Who should get an MRI for ovarian cancer evaluation?
MRI isn’t needed for everyone with ovarian concerns. It’s most useful in specific cases, especially for younger women or when blood tests aren’t helpful. Your doctor may order an MRI if:
The ultrasound shows a mass that’s difficult to classify
Fertility preservation is your concern
More details are needed for surgical planning
The mass appears complex or unclear on ultrasound
Is MRI safe during pregnancy if ovarian cancer is suspected?
MRI can be safely performed during your pregnancy and should not be avoided if it’s needed to diagnose a serious condition. It’s considered a safe option for evaluating ovarian masses when ultrasound results are unclear. However, contrast dye is usually avoided during pregnancy and used only when absolutely necessary.
What is the biggest indicator of ovarian cancer?
The main warning signs are ongoing stomach pain, persistent bloating, frequent or urgent urination, and feeling full quickly when eating. If these symptoms occur more than 12 times a month, they should be checked by your doctor. A blood test measuring CA-125, a protein that’s often elevated in ovarian cancer, may also be used – but high levels can happen in non-cancerous conditions too.
What test confirms ovarian cancer?
A surgical biopsy is the only test that can confirm ovarian cancer. Imaging tests like ultrasound, MRI, and CT scans can show suspicious areas but can’t make a definite diagnosis. During surgery, your doctor will remove tissue samples or the entire mass for lab testing under a microscope.
How accurate is MRI at detecting early-stage ovarian cancer?
An MRI is highly accurate at detecting ovarian tumours and it can correctly identify cancer in most cases. However, very small tumours can sometimes be missed, and early-stage ovarian cancer often causes few or no symptoms. When ovarian cancer is found early, most patients have a high chance of living more than five years after diagnosis.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situation, please consult a specialist at Thomson Medical. Schedule an appointment with Thomson Medical today.
Citations
MRI scan. (n.d.). Tests and Scans | Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/tests-and-scans/mri-scan
Sohaib, S. a. A. (2007). MR imaging in ovarian cancer. Cancer Imaging, 7 (Special Issue A), S119–S129. https://doi.org/10.1102/1470-7330.2007.9046
Themes, U. (2019, November 8). Role of magnetic resonance imaging in the evaluation of gynecologic disorders. Obgyn Key. https://obgynkey.com/role-of-magnetic-resonance-imaging-in-the-evaluation-of-gynecologic-disorders/
Lin, R., Hung, Y., Cheng, J., & Suh-Burgmann, E. (2022). Accuracy of magnetic resonance imaging for identifying ovarian Cancer in a Community-Based setting. Women S Health Reports, 3(1), 43–48. https://doi.org/10.1089/whr.2021.0106
Wagner, E., Leonardo, D., & MyOvarianCancerTeam. (2023, October 12). Ovarian Cyst vs. Ovarian Cancer: Differences on MRI Scans. MyOvarianCancerTeam. https://www.myovariancancerteam.com/resources/ovarian-cyst-vs-ovarian-cancer-differences-on-mri-scans
Hassan, F. a. M., Megally, H. I., & Moubark, M. (2025). Role of magnetic resonance imaging in characterization of superficial soft tissue masses. The Egyptian Journal of Radiology and Nuclear Medicine, 56(1). https://doi.org/10.1186/s43055-025-01487-0
Peritoneal carcinomatosis - Diagnosis and treatment - Mayo Clinic. (n.d.). https://www.mayoclinic.org/diseases-conditions/peritoneal-carcinomatosis/diagnosis-treatment/drc-20585172
Horga, G., Kaur, T., & Peterson, B. S. (2014). Annual Research Review: Current limitations and future directions in MRI studies of child‐ and adult‐onset developmental psychopathologies. Journal of Child Psychology and Psychiatry, 55(6), 659–680. https://doi.org/10.1111/jcpp.12185
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Dr Wang Junjie
Obstetrics & Gynaecology (O&G)
Thomson Women's Clinic & Cancer Surgery
English, Mandarin
Prudential, Alliance MediNet

