Finding out that you are pregnant is, of course, a joyous moment, especially if you have been trying to conceive for some time. However, if you begin bleeding and experience cramps similar to menstrual cramps shortly after, this can be concerning.
When your doctor confirms low hCG levels and uses clinical terms like "chemical pregnancy" or even says you're not having a miscarriage, you may feel confused or dismissed, making your loss appear insignificant. However, understand that what you went through was a genuine loss that deserves to be acknowledged and supported.
What is a chemical pregnancy?
A chemical pregnancy is a medical term used to describe a very early miscarriage that occurs before the 5th week of pregnancy. Although the term may sound clinical or dismissive, it simply refers to the only indicator of pregnancy at this early stage, the human chorionic gonadotropin (hCG) hormone produced by the embryo and detected by a positive pregnancy test.
The exact cause of a chemical pregnancy is currently unknown. However, in general, early pregnancy loss could be due to genetic issues. If an egg or sperm contains more or fewer chromosomes (tiny structures inside cells that carry your genes) than normal, the resulting embryo will have the same abnormality, increasing the risk of early pregnancy loss.
Although a chemical pregnancy differs from a clinical pregnancy, where the foetus has grown enough to be detected by ultrasound, this doesn’t mean that your pregnancy is not real or that your grief is not justified.
Symptoms of chemical pregnancy

Because of the nature of this very early pregnancy loss, some women may not be aware they have had it if they do not miss a period or take a pregnancy test. However, there are a few symptoms you can look out for, such as:
Vaginal bleeding even after positive pregnancy test
A positive pregnancy test that turns negative in a few days
Delayed period followed by heavier bleeding than usual
Cramping similar to a period
Blood tests showing hCG dropping quickly
What is a miscarriage?
A miscarriage is defined as the unexpected loss of a clinical pregnancy before 20 weeks. This is medically different from a chemical pregnancy, which occurs before a pregnancy sac can be seen on ultrasound.
Just because it’s called a “miscarriage” does not mean that you did something wrong or that there was something wrong with carrying the pregnancy. Most miscarriages occur in the first trimester and cannot be prevented – they happen naturally due to genetic or other issues that cause the foetus to stop developing.
Symptoms of miscarriage
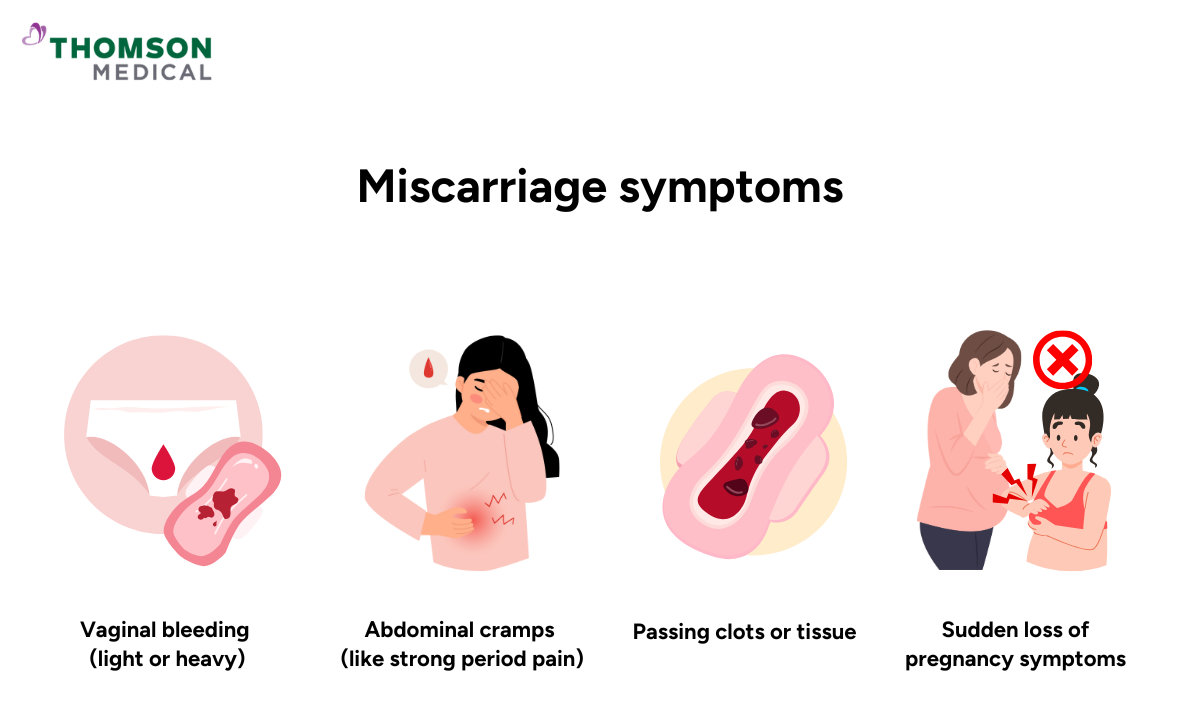
Although the foetus is able to begin developing during a clinical miscarriage, it’s difficult to determine the first signs of miscarriage because symptoms vary from person to person. Sometimes there are no signs of miscarriage, and you only find out at an ultrasound imaging that you have lost the pregnancy.
However, the most common signs of miscarriage are generally:
Vaginal bleeding (which may be lighter or heavier than normal)
Abdominal cramps that resemble strong period pain
Passing clots or tissue
Sudden reduction in pregnancy symptoms, such as breast tenderness or nausea
Although it is very disheartening going through this difficult time, remember that you don't need to blame yourself, as these conditions are out of our control. Though you are understandably grieving, it is important to contact your healthcare provider if you suspect an early or clinical miscarriage.
Regardless of when or at what stage the pregnancy loss occurred, your grief and feelings are equally valid. You also deserve compassionate care from specialists who understand your concerns. Schedule an appointment with Thomson Women's Clinic, where our obstetricians and gynaecologists (O&G) can help provide medical care and support you through this difficult time.
What's the difference between a chemical pregnancy vs miscarriage?
To help mothers better understand the difference between a chemical pregnancy and a clinical miscarriage during these difficult times, here is a table that outlines their distinctions.
| Chemical pregnancy | Clinical miscarriage | |
|---|---|---|
Time of loss | Before 5 to 6 weeks of pregnancy | Before 20 weeks of pregnancy |
Ultrasound | No pregnancy sac visible | Pregnancy sac and potentially heartbeat visible |
Detection | Positive pregnancy test followed by negative test | Positive pregnancy test with ultrasound confirmation of pregnancy or passing of tissues or blood |
Symptoms | Often absent or mild bleeding/cramping around expected period | Bleeding, cramping pain, or passing out tissues |
However, Mother needs to remember that the medical terminology and timing don't diminish the significance of your experience or your right to grieve. Whether your loss occurred at 5 weeks or 15 weeks, both represent the loss of a pregnancy you had hopes for.
Our O&G specialists
Loading...
Treatment for chemical pregnancy and miscarriage
It's understandable if a mother feels overwhelmed or anxious processing the emotional impact of pregnancy loss. But it's still beneficial for a mother to understand the treatment for miscarriage so she can make an informed decision.
Chemical pregnancy treatment
In most cases, a chemical pregnancy resolves naturally without a medical intervention. This is because the bleeding and cramping you experienced are generally similar to a normal period, and your body naturally passes the pregnancy tissue.
However, if your bleeding is heavier or more painful than normal, or if you experience recurring chemical pregnancies, you should seek medical attention from a fertility specialist.
Clinical miscarriage treatment
On the other hand, treatment for clinical miscarriage depends on the type of miscarriage, your pregnancy stage, and your comfort level, which include:
Nonsurgical treatment:
Sometimes, your body will pass the tissue naturally over a few days or weeks, and if no tissue remains, no further treatment will be necessary.
That said, your healthcare provider will usually still perform ultrasound scans to ensure everything is clear.
Surgical treatment:
If the pregnancy tissue isn't completely expelled when the foetus passes, it could cause complications, so it will need to be removed through a dilation and curettage (D&C) procedure.
The most suitable treatment for you will depend on your preferences and circumstances. Your healthcare provider will advise you on the safest and most comfortable method.
To find out more about treatment for first-trimester miscarriage and an assessment of your reproductive health, schedule an appointment with an O&G specialist at Thomson Women's Clinic that can support you during this difficult fertility journey.
Could these conditions affect my fertility?
A chemical pregnancy or clinical miscarriage usually does not affect fertility. Most women who have a miscarriage get their period around two weeks after any light bleeding or spotting stops. It's possible to become pregnant during this usual menstrual cycle immediately following a miscarriage.
However, since miscarriage can be emotionally taxing, if you decide to try again, make sure that you are both mentally and physically ready. Generally, women who miscarry go on to have healthy pregnancies. Only about 2-5% of people experience two miscarriages in a row, and 1-2% experience three consecutive losses, so don't be disheartened.
How soon can I try to conceive again?
It is generally recommended to wait at least one menstrual cycle (about 4-6 weeks) before trying to conceive again after a miscarriage. This waiting period allows your body to recover physically and emotionally. However, some healthcare providers suggest waiting up to three months.
If there are no medical reasons to wait, it's up to you when you start trying again. You may need more time to heal and grieve for your loss. Alternatively, you may feel that trying again will help you come to terms with what's happened. The timing is up to you and your partner.
How to cope with these fertility challenge?

It’s normal to feel disheartened after a miscarriage, which can leave you with a range of emotions and many questions. Emotional healing from a miscarriage often takes longer and is more difficult than physical healing.
Take time to grieve and care for your mental and physical health, as this will improve your well-being. Here are a few things you could do to help you get through this difficult time:
Seek emotional support:
Experiencing a pregnancy loss can be disappointing. To help you cope, allow yourself to grieve and seek support from loved ones, a therapist, or a support group.
It is normal to experience grief on this fertility journey, and you don't need to face it alone. This is because your mental health plays a significant role in your overall well-being during your fertility journey.
Maintain a healthy lifestyle:
To support a healthy pregnancy after miscarriage, it is recommended that you adopt a healthy lifestyle. This includes eating a balanced and nutritious diet, maintaining a healthy weight, reducing alcohol intake, staying hydrated, and exercising regularly.
Communicate with your partner:
During this difficult time, it's important to talk openly and honestly with your partner. This will help you both to work together and support each other. Talk about your feelings openly and discuss your hopes and fears about future pregnancy.
Open communication can help you feel less isolated and frustrated, as well as more connected to your partner.
Manage stress:
Create a calm, stress-free environment and practise stress management techniques such as meditation, maintaining a positive attitude, or doing breathing exercises to help manage your stress levels.
Take adequate rest:
You should aim for 7-9 hours of sleep each night, as a good night's rest can help maintain your regular menstrual cycle. Not getting enough sleep can cause your body to produce more cortisol, a stress hormone, which can affect your reproductive health.
To help you cope with these challenging times, consider consulting with an O&G specialist who can provide a tailored recommendation for your condition.
FAQ
How is a chemical pregnancy confirmed?
A chemical pregnancy is usually confirmed using a combination of pregnancy tests, blood tests, and ultrasounds. It is characterised by an initial positive pregnancy test result, followed by a negative result or a drop in hCG levels, which indicates that the pregnancy ended before it could be seen on an ultrasound scan (clinical pregnancy).
Is every early miscarriage considered a chemical pregnancy?
Not all early miscarriages are considered chemical pregnancies. While there are many types of miscarriage, most that occur before the fifth or sixth week of pregnancy are chemical pregnancies.
Can I be 5 weeks pregnant and still test negative?
Yes, it is possible to be 5 weeks pregnant and still get a negative result on a home pregnancy test. Although pregnancy tests are generally accurate, they detect the pregnancy hormone hCG.
Some tests may not detect levels of this hormone sufficiently, especially in the early stages of pregnancy. You could wait a few days and take another test.
How can I tell if I experienced a miscarriage or just a late period?
You may have miscarried if you experience any of the following:
Bleeding less than two weeks after your expected period
Bleeding that is heavier than usual
Bleeding that lasts longer than usual
Accompanied by clots or tissues that you do not usually see during your period
If you are concerned about your bleeding or any other symptoms, you should always consult your healthcare provider.
Does a chemical pregnancy mean I am fertile?
Yes, it can be considered a positive sign that conception is possible. Many people who have experienced a chemical pregnancy go on to have successful pregnancies.
Can stress cause a chemical pregnancy?
While some studies suggest a link between extreme or chronic stress and miscarriage, stress is not a direct cause of a chemical pregnancy. Most pregnancy losses, including chemical pregnancies, are caused by chromosomal (genetic) abnormalities in the developing embryo.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, schedule an appointment at Thomson Women’s Clinic.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
