Occasionally, a pregnancy ends before reaching full term. When this happens, the pregnancy tissue often passes naturally, but in some cases, it remains in the uterus (womb), and your doctor may recommend a medical procedure to remove it. This typically involves a D&C (dilation and curettage) or a D&E (dilation and evacuation), depending on how advanced the pregnancy was.
If you've been advised to undergo this procedure, it's natural to have questions and concerns. To help you during this difficult time, let's walk through what these procedures involve so you can feel more prepared.
What is the evacuation of the uterus?
The evacuation of the uterus is a medical procedure performed by your doctor by dilating the cervix (the neck of the womb) to allow the evacuation of pregnancy tissue post-miscarriage or abortion. This procedure is important to reduce the risk of infection and heavy bleeding and ensure that the uterus is completely empty.
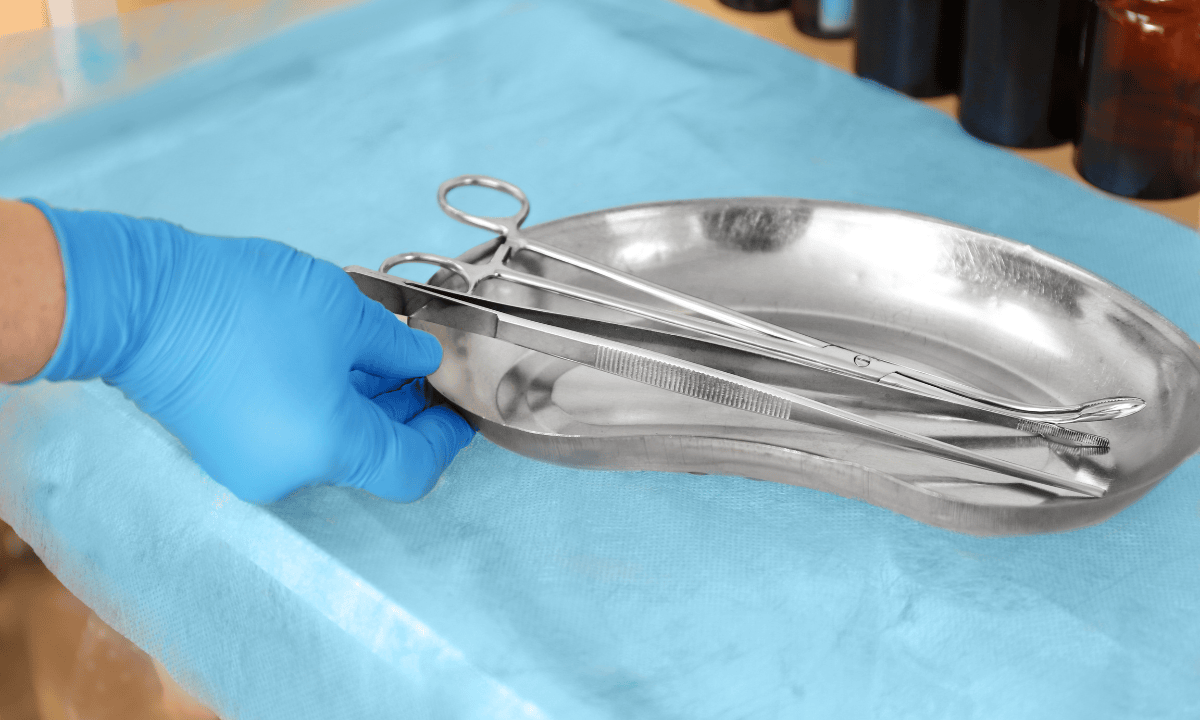
Depending on how far the pregnancy has progressed, your doctor can perform one of two procedures. If the pregnancy is approximately 12-13 weeks or less (first trimester), a procedure called dilatation and curettage (D&C) is performed. This involves dilating the cervix and inserting a thin, spoon-shaped instrument called a curette to gently remove tissue from the uterine lining.
However, if the pregnancy is in the second trimester (after 13 weeks), a procedure called dilatation and evacuation (D&E) is typically recommended. This is because as pregnancy progresses, the pregnancy tissue increases in size and volume. During D&E, the cervix is dilated more widely, and your doctor uses specialised forceps and gentle vacuum suction to carefully remove the pregnancy tissue.
When are these procedures recommended?
Your doctor may recommend a uterine evacuation if medical conditions during pregnancy lead to either pregnancy loss or pregnancy termination (abortion). Conditions that indicate the need for surgical uterine evacuation include:
Termination of pregnancy:
When a medical termination of pregnancy (MTOP) or medical abortion is performed, two medications called mifepristone and misoprostol are given to induce an artificial miscarriage.
However, sometimes the miscarriage process hasn't been completed naturally, requiring surgical evacuation.
Missed miscarriage:
This occurs when pregnancy has ended, but the tissue hasn't passed naturally, with no symptoms of miscarriage such as bleeding or pain.
Incomplete miscarriage:
This occurs when some pregnancy tissue remains in the uterus after a miscarriage has begun.
Both D&C and D&E procedures are performed under anaesthesia, so you won't feel any pain during the process. Your doctor will discuss which anaesthetic is best for you, whether regional anaesthesia (an injection to numb part of the body) or general anaesthesia (where you are fully asleep).
If you have questions or concerns about these procedures, our obstetricians and gynaecologists (O&G) at Thomson Women's Clinic are here to help. Schedule an appointment to consult your options and address any concerns you may have.
Our O&G specialists
Loading...
Recovering from uterine evacuation
After a uterine evacuation procedure, you'll likely spend a few hours in a recovery room so that you can be monitored for heavy bleeding or other complications. This also gives you time to recover from the effects of anaesthesia; once you feel well and have been reviewed by the doctor, you may go home.
After the uterine evacuation procedure, you may experience side effects such as mild cramping or light vaginal bleeding. These symptoms typically last a few days but can continue for up to two weeks. To help you recover and reduce the risk of complications, here's what you can do:
Stay hydrated by drinking plenty of fluids.
Avoid sexual intercourse until the bleeding stops.
Rest when you feel tired, and ensure you get adequate sleep.
Use sanitary pads instead of tampons until your next period.
If your stomach hurts, choose bland, low-fat foods like plain rice, broiled chicken, toast, and yoghurt.
Take the full course of the prescribed antibiotics to reduce your risk of getting an infection.
If you are more than 20 weeks pregnant at the time of this procedure, you may be prescribed medication to stop your breasts from producing milk.
When to contact your doctor
After a uterine evacuation procedure, it's important to know what symptoms require medical attention. Although serious complications are uncommon, contact your doctor immediately if you experience any of the following:
Fever (38°C or higher)
Heavy bleeding (soaking through two or more pads per hour for two consecutive hours)
Severe abdominal pain that's not relieved by painkillers
Unusual or foul-smelling discharge that may indicate an infection
Passing large blood clots from the vagina
The following are potential complications that may arise from a uterine evacuation procedure, though they are uncommon:
Infection
Heavy bleeding or haemorrhage
Cervical or vaginal injury
Bowel or uterine perforation
Incomplete or failed abortion
Intrauterine adhesions or Asherman's syndrome (scar tissue that forms inside of the womb)
Most complications and other high-risk symptoms can be managed effectively if detected early. If you experience any of these symptoms, don't hesitate to schedule an appointment at Thomson Women's Clinic.
Does uterine evacuation affect my fertility?

A uterine evacuation procedure usually does not affect fertility. Ovulation can occur as soon as two weeks after the procedure, once your womb has healed. So it's possible to become pregnant during this usual menstrual cycle.
Since miscarriage or termination of pregnancy can be emotionally taxing, if you decide to try again, make sure that you're mentally and physically ready. Generally, women who miscarry go on to have healthy pregnancies. Only about 2-5% of people experience two miscarriages in a row, and 1-2% experience three consecutive losses, so don't be disheartened.
How soon can I try to conceive again?
It's generally recommended to wait at least one menstrual cycle (about 4-6 weeks) before trying to conceive again after a miscarriage. This waiting period allows your body to recover physically and emotionally.
However, don’t begin having intercourse until your healthcare provider tells you it’s safe to do so (usually about one to two weeks after the procedure). Usually it's until your cervix closes and returns to its normal size to prevent bacteria from entering your vagina and causing an infection. Your doctor will tell you when you can resume having sexual intercourse.
If there are no medical reasons to wait, it's up to you when you start trying again. But if you think you need more time to heal and mourn your loss, you can wait until you're ready. You might also think that trying again will help you deal with what happened. The timing is up to you and your partner.
FAQ
How long does an evacuation of the uterus take?
The procedure itself usually takes 10-15 minutes for a D&C and 20-30 minutes for a D&E. However, you should allow for approximately 1-2 hours at the clinic or hospital in total, including preparation time and monitoring in the recovery room after the procedure.
How can I tell if my uterus has been completely evacuated?
Your doctor will use an ultrasound scan during the procedure to make sure that all the pregnancy tissue has been removed. You will have a follow-up appointment 4-6 weeks after the procedure to confirm that your recovery is progressing well.
It's normal to experience some bleeding for up to two weeks afterwards. However, you should contact your doctor immediately if you experience heavy bleeding (soaking through two or more pads per hour for two consecutive hours), severe pain, a fever or foul-smelling discharge.
Will it be painful during an evacuation of the uterus?
You won't feel any pain during the procedure because you will be under anaesthesia. This can be either regional anaesthesia, which involves an injection in your lower back that numbs you from the waist down while you remain awake, or general anaesthesia, where you are fully asleep.
How will I feel after an evacuation of the uterus?
In the first few days after the procedure, you may experience:
- Mild cramping, similar to period cramps
- Light vaginal bleeding or spotting
- Feeling tired or drowsy (especially if you had a general anaesthetic)
These symptoms are normal and should gradually improve. Most women feel well enough to resume light activities within one to two days, although it typically takes one to two weeks to make a full recovery.
How long will I bleed after an evacuation of the uterus?
Light bleeding or spotting usually lasts for a few days to two weeks afterwards. The bleeding should gradually become lighter over time. It is normal to occasionally pass small blood clots.
How long should I rest after the evacuation of the uterus?
For the first 24-48 hours, you should rest at home and avoid strenuous activities. You are not allowed to drive or perform heavy lifting for 24 hours after receiving general anaesthesia. After one to two weeks, you can typically resume normal activities, including exercise. But you should abstain from sex until your doctor says it's safe, usually after bleeding stops and your cervix closes.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations for your specific conditions, schedule a consultation with our O&G specialist at Thomson Women’s Clinic.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
