What are endometrial (uterine) polyps?
Endometrial polyps, or uterine polyps, are abnormal tissue growths that occur in the endometrium, which is the lining of the uterus.
They are caused by an overgrowth of endometrial tissue and are connected to the uterine lining by a thin stalk or broad base that extends into the uterine cavity.
These polyps may be of different sizes, ranging from very small to larger growths that occupy more space in the uterus. Some women may have a single polyp, while others may have more than one polyp.
Although most polyps are benign (not cancerous), they can sometimes create problems, like fertility issues or abnormal bleeding.
Who is affected by endometrial polyps?
Endometrial polyps can occur in women of any age, but you may be more likely to develop them if you:
Are in your 40s or 50s, especially during perimenopause or menopause
Have certain health issues, such as:
Obesity
High blood pressure
Diabetes
Take hormone replacement therapy (HRT)
Have higher levels of oestrogen in your body
Have had previous uterine surgeries, like dilation and curettage (D&C) or hysteroscopy.
Although polyps are more common as you approach menopause, they can develop at any age—even in your 30s. But just because you have these risk factors doesn't mean you'll develop polyps, and not all polyps produce characteristic symptoms.
What causes endometrial polyps?
While the exact cause is not fully understood, they are believed to result from hormonal imbalances, particularly elevated oestrogen levels.
Several factors that may contribute to the formation of these polyps include:
Genetic Predisposition:
You might have certain genetic mutations that increase your likelihood of developing polyps.
Hormonal changes:
If your body produces too much oestrogen without enough progesterone to balance it, abnormal tissue growth can occur.
Obesity and metabolic conditions:
Being overweight or having metabolic disorders can affect your hormone levels, raising the risk of polyp development.
While these factors can increase your risk, it’s important to remember that not everyone with these risk factors will develop endometrial polyps. If you have concerns about your risk or symptoms, discussing them with your healthcare provider can help clarify your situation and guide you on what to monitor.
Gynaecologist in Singapore
Loading...
What are the symptoms of uterine polyps?
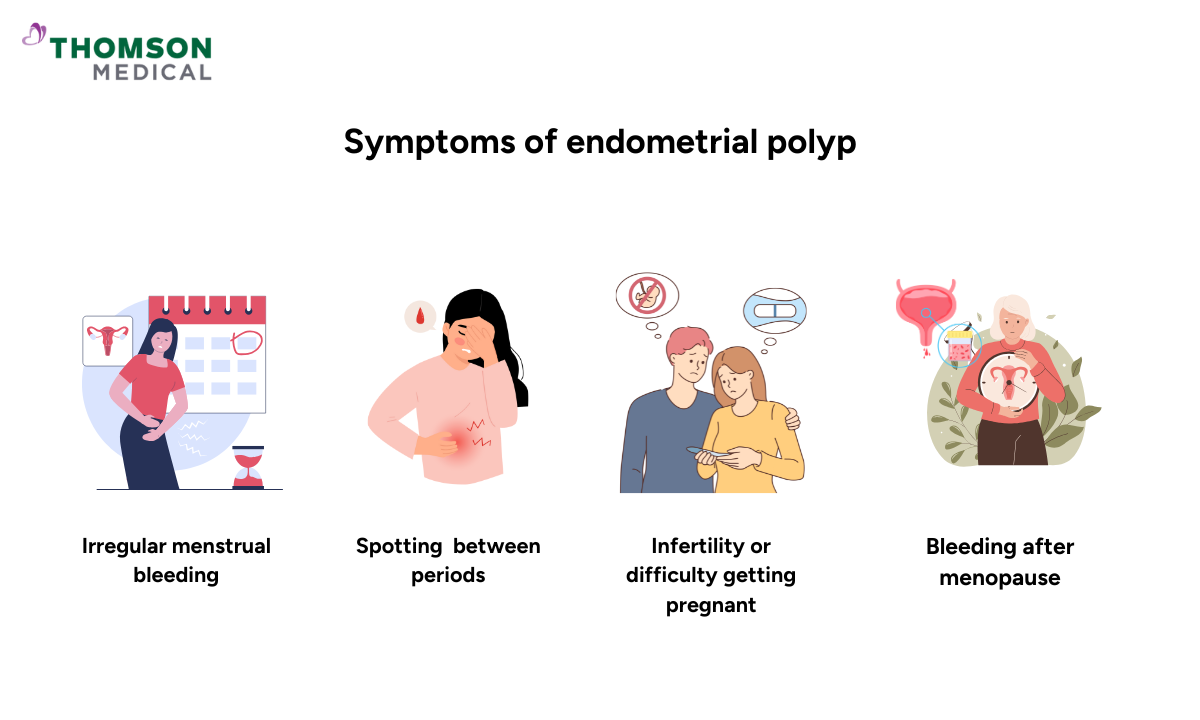
Some women have asymptomatic polyps, meaning they experience no symptoms at all. However, if symptoms do occur, they can include:
Irregular menstrual bleeding (heavy, prolonged, or frequent periods)
Spotting or bleeding between periods
Bleeding after menopause
Infertility or difficulty getting pregnant
Bleeding after intercourse
Lower abdominal or pelvic pain (less common)
If you are experiencing any of these issues, consider speaking with your healthcare provider.
If you're experiencing symptoms of an endometrial polyp, talking to a healthcare provider is a great first step. Request an appointment with Thomson Medical for a comprehensive evaluation. Our specialists may recommend an endometrialpolyp ultrasound to accurately assess your condition and create a personalised treatment plan.
How are endometrial polyps diagnosed?
To diagnose uterine polyps, your healthcare provider may use various methods, including:
Transvaginal ultrasound
A thin, handheld device is inserted into the vagina to produce sound waves that create images of the inside of your uterus.
Hysterosonography
In this test, your doctor may use sterile fluid to gently expand your uterus through a thin, flexible tube (catheter), making it easier to see polyps on an ultrasound.
Hysteroscopy
Your provider will insert a long, thin tube equipped with a lighted telescope, known as a hysteroscope, through your vagina and cervix into your uterus. This procedure enables your provider to closely examine the interior of your uterus. Hysteroscopy is often performed alongside surgical procedures to remove uterine polyps.
Endometrial biopsy
A small tissue sample is taken from the uterine lining using a suction catheter to check for cancer cells in the polyp.
Curettage
A curette, a long metal instrument with a small loop on one end, is used to remove a tissue sample from the polyp for laboratory analysis.
These diagnostic techniques help your healthcare provider determine the presence of uterine polyps and assess their characteristics.
How are endometrial polyps treated?
Endometrial polyp treatment varies based on the severity of the symptoms and the size of the polyps. The following are common ways to treat the polyps:
Watchful waiting
Your doctor may suggest monitoring the polyps with regular ultrasounds if they are small and asymptomatic, as they may resolve on their own.
Medications
Hormonal treatments, including progestin therapy, may be used to shrink polyps. Still, medication is not typically the first choice for treatment.
Surgical removal
The most common treatment for symptomatic polyps is hysteroscopic polypectomy, where a hysteroscope is used to remove the polyps from the uterus. This procedure can be done on an outpatient basis.
Dilation and Curettage (D&C)
A D&C may be performed in some cases to eliminate uterine polyps.
In females with recurrent polyps, especially if they are symptomatic, hysteroscopic resection is generally recommended to prevent their recurrence.
FAQ
How serious is an endometrial polyp?
Endometrial polyps are usually benign (not cancerous) and not serious. They may, however, lead to complications like:
Abnormal bleeding, which may affect the quality of life of a woman.
Infertility is the inability to become pregnant due to benign polyps causing disruption of implantation or blockages within the uterus.
Increased risk of uterine cancer, although it is rare, especially in postmenopausal women.
Should all endometrial polyps be removed?
Not all endometrial polyps need to be removed. Polyp removal is dependent on several factors, such as endometrial polyp size, symptoms, and suspicion of malignancy. Removal may be necessary for symptomatic or fertility-interfering polyps.
If the polyp is small and asymptomatic, it may be observed with serial ultrasounds. A healthcare provider can recommend the best course of action depending on the circumstance.
Can polyps be seen in ultrasound?
Yes, polyps of the endometrium should typically be visible on an ultrasound, especially on a kind of ultrasound called a transvaginal ultrasound, which provides a good image of the uterus. Sometimes a saline infusion sonogram (also called a hysterosonogram) is utilised to aid visibility. In other cases, a hysteroscopy (a test where a camera is placed into the uterus) will be required to obtain a closer look.
How to remove endometrial polyps naturally?
There are no conventional natural approaches to remove endometrial polyps, and medical treatment or surgery (including hormone therapy) is typically recommended. However, some women attempt to treat polyps with lifestyle changes such as maintaining normal weight, a well-balanced diet with anti-inflammatory foods, and exercise.
Although some women use natural products, such as phytoestrogens (flaxseeds and soy) or herbal supplements (turmeric and green tea), there is no scientific evidence that these can effectively remove endometrial polyps. It’s always best to speak with a health care provider for appropriate diagnosis and treatment plans.
What could be causing my symptoms of uterine polyps?
Symptoms of uterine polyps, such as irregular bleeding, spotting between periods, or pelvic discomfort, may be caused by various factors. These include hormonal imbalances, endometrial hyperplasia, fibroids, or other uterine conditions. It is important to consult a healthcare provider for an accurate diagnosis through ultrasound or other diagnostic tests.
How do you stop polyps from growing in your uterus?
Hormonal balance
Endocrine disruption, especially too much oestrogen, may result in polyp formation. A physician may recommend birth control or hormone therapy to regulate oestrogen levels.
Healthy lifestyle
Maintaining a healthy weight, regular physical activity, and a healthy diet can reduce the risk of polyps.
Monitor and manage conditions
Some conditions, such as obesity, diabetes, or high blood pressure, can place you at higher risk, so managing these can help.
Avoid excess exposure to oestrogen
It is beneficial to reduce exposure to oestrogen, especially through hormone replacement therapy.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
