During your menstruation, you may have experienced heavy cramps alongside blood clots, which you initially thought was just a bad period. However, your menstrual bleeding doesn't stop at the expected time (around five days later), and your cycle becomes irregular; suddenly, you have the gut feeling that something is wrong.
One possible cause of these conditions is endometrial polyps, also known as uterine polyps. These benign growths can negatively affect your reproductive health and disrupt your daily activities.
What is an endometrial polyp?
Endometrial polyps are abnormal growths that attach to the inner lining of the uterus (the endometrium). They form when cells in the endometrial tissue overgrow and may show up as single or multiple growths. While typically non-cancerous (benign), in some cases they can develop pre-cancerous changes or, rarely, become cancerous.
Uterine polyps range in size from a few millimetres – no larger than a sesame seed – to several centimetres. They attach to the uterine wall with a large base or a thin stalk. They usually remain in the womb but can sometimes slip through the cervix into the vagina.
What causes endometrial polyps?
Although the exact cause of these polyps is currently unknown, it is thought that oestrogen plays a role in their development. This is because the oestrogen hormone stimulates the growth of the endometrium during the menstrual cycle to prepare for the implantation of a fertilised egg.
However, when there is an excess of oestrogen hormone, particularly when there is insufficient progesterone to balance it, the endometrial tissue can overgrow and form uterine polyps.
What are the risk factors for endometrial polyps?
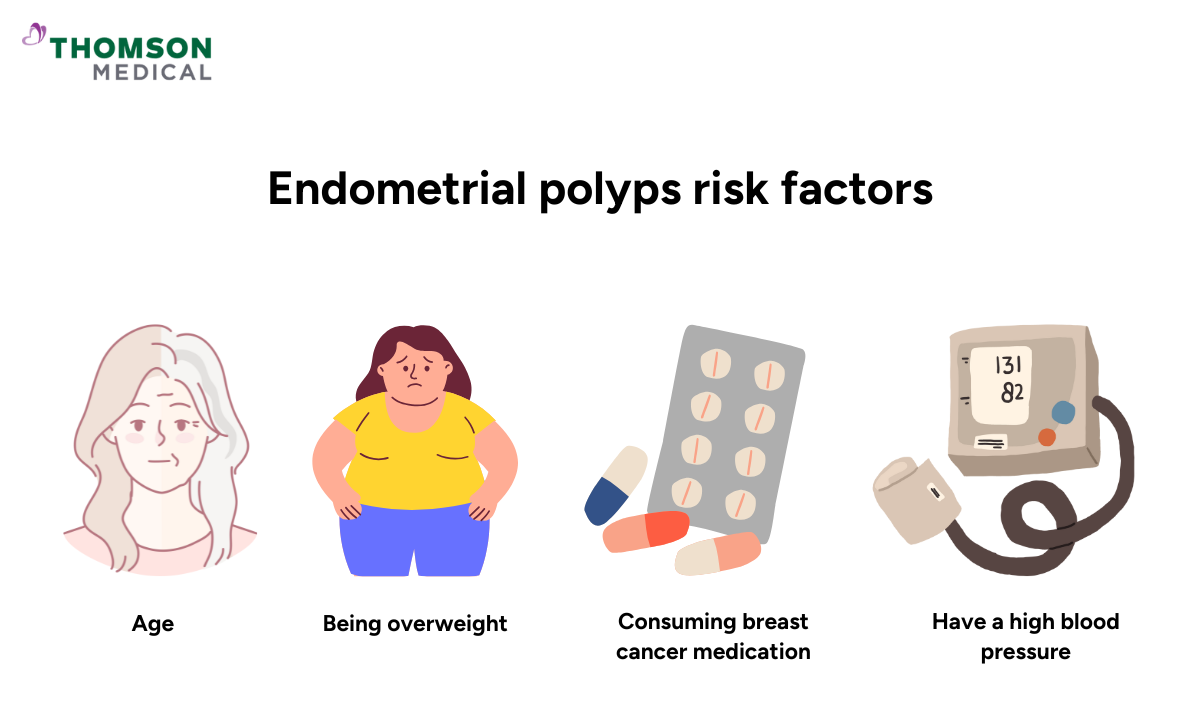
There are several factors that can increase your risk of developing endometrial polyps. Some of these factors include:
Age:
If you are in your 40s or 50s and approaching menopause (perimenopause), oestrogen levels can spike higher than normal or drop sharply from cycle to cycle, which can increase the risk of polyp growth.
Additionally, if you are postmenopausal (aged 50 or over), despite lower overall oestrogen levels, the absence of regular progesterone increases polyp risk.
Body weight:
Being overweight (BMI 25 to 29.9) or obese (BMI >30) can increase the risk of this abnormal growth.
Cancer medication:
Certain medications used to treat breast cancer, such as tamoxifen, can increase the risk of developing uterine polyps.
Hormonal therapy:
Taking a high dose of hormone replacement therapy (HRT) oestrogen for menopause without adequate progesterone can also increase the risk of these polyps.
Genetic condition:
You have a family history of Lynch and Cowden syndromes.
High blood pressure:
Having high blood pressure (hypertension) may also contribute to the development of these polyps.
If you are at risk of developing uterine polyps, timely detection can prevent these growths from worsening and protect your reproductive health. Schedule an appointment with Thomson Women's Clinic and Cancer Surgery, where our obstetrician and gynaecologist (O&G) specialists can perform further assessments and take steps to manage these growths early.
What are the symptoms of endometrial polyps?
If the polyp is small, you may not experience any symptoms. However, when symptoms do occur, they often manifest as:
Prolonged periods
Bleeding after an intercourse
Irregular menstrual periods
Abnormal vaginal discharge
Heavy menstrual bleeding during periods
- In some women, endometrial polyps may cause infertility issue
Although these symptoms may be mistaken for particularly intense menstrual periods, it is recommended that you consult an O&G if you experience postmenopausal bleeding or vaginal bleeding or spotting when you are not on your period.
This is because abnormal vaginal bleeding can be a sign of endometrial polyps, particularly if you are postmenopausal.
Our obstetrician and gynaecologist
Loading...
How are endometrial polyps diagnosed?
To diagnose uterine polyps, your healthcare provider will review your medical history, ask about any medications you are currently taking and check for any symptoms you are experiencing.
If you still have periods, they may ask about the specifics of your menstrual cycle and fertility, including how long your periods last, how often you have them and whether you have had difficulty conceiving. If you are postmenopausal, your doctor may ask if you have noticed any bleeding or spotting.
Following this, they will perform a pelvic examination and a Pap smear to check for polyps. They may also perform additional tests to confirm the diagnosis. These investigations may include:
Transvaginal ultrasonography:
During transvaginal ultrasound, your doctor inserts a handheld device called an ultrasound transducer into your vagina. The device emits sound waves that provide an image of the inside of your uterus, including any irregularities that may be present.
Sonohysterography:
After the initial transvaginal ultrasound, your doctor will inject some sterile fluid into the hollow part of the womb (uterine cavity) through a thin, flexible tube (catheter) before doing the endometrial polyp ultrasound again. The fluid causes the uterine cavity to expand to provide a clearer image of any growth in the womb.
Hysteroscopy:
Your doctor inserts a long, thin tube with a lighted telescope (hysteroscope) through the vagina and cervix to examine the inside of the womb.
Endometrial biopsy:
Your doctor inserts a thin, soft plastic instrument to collect some tissues from the inner wall of your uterus. The tissues will then be sent to the laboratory to detect any abnormal cells.
Curettage:
Your doctor inserts a long metal instrument called a curette to scrape the tissues or polyps from the inner wall of your uterus. The tissues or polyps will then be sent to the laboratory to detect any abnormal or cancerous cells.
How are endometrial polyps treated?
The treatment you receive will depend on your symptoms and other factors that may increase your risk of developing endometrial cancer. Your healthcare provider will decide which treatment approach is suitable for your condition, but in general, options include:
Watchful waiting:
If you still have regular menstrual cycles and the polyp isn’t causing any symptoms, your doctor may recommend monitoring it. This is because small polyps might resolve on their own.
Medication:
Another way to treat uterine polyps is to use hormonal medication to balance your hormones and relieve the symptoms.
Surgical removal
Uterine polypectomy is a medical procedure to remove a polyp, which is performed through hysteroscopy, which allows your doctor to insert tools that can be used to cut and remove polyps.
In cases where the polyps contain cancer cells, a hysterectomy – surgery that involves removing your uterus – may be necessary. This is typically reserved for postmenopausal women or when fertility preservation isn't required.
Endometrial polyp treatment at Thomson Medical

If you have any concerns about endometrial polyps, or if you are experiencing symptoms such as irregular bleeding or a prolonged period, it is important to seek a proper evaluation. Early detection and monitoring can help prevent growth progression and ensure appropriate treatment.
To support you, Thomson Women's Clinic and Cancer Surgery offer a 4-in-1 women's screening package designed to detect uterine (endometrial) abnormalities, which include:
Consultation & examination:
A one-to-one session with an O&G specialist to review your health history and assess your current concerns.
ThinPrep Pap test (Pap smear):
A Pap smear is a screening test that examines cells from the cervix to check for precancerous or abnormal changes.
HPV test:
The HPV test identifies high-risk Human Papillomavirus (HPV) strains associated with cervical cancer.
An imaging test that provides an internal view of the uterus, ovaries, and surrounding structures.
If you would like more information about these screening options, schedule a consultation with our O&G specialist at Thomson Women's Clinic and Cancer Surgery.
You are not alone
Experiencing symptoms like irregular bleeding or discovering you have endometrial polyps can feel overwhelming, but remember – you are not alone. At Thomson Women's Clinic and Cancer Surgery, our specialist provides thorough support, from diagnosis to treatment and follow-up care.
We also offer comprehensive procedures to help diagnose and treat endometrial polyps and related gynaecological conditions, which include:
Uterine polypectomy:
Polypectomy procedures cost between SGD 767 and SGD 4,300 for inpatient surgeries, depending on whether you choose a public or private hospital.
During a polypectomy, hysteroscopy is used to visualise and safely remove the polyps from your womb.
Hysteroscopy:
A hysteroscopy cost can range from SGD 696 to 10,905, depending on if the procedure is performed on an outpatient or inpatient basis.
However, additional charges may arise for expenses such as pre-surgery consultations, imaging tests (e.g., X-rays or CT scans), medications, and post-surgery follow-up appointments.
Fortunately, there are several programmes in Singapore that can help lower the total cost, such as MediSave, MediShield Life, and Integrated Shield Plans. Each of these offers different levels of coverage depending on your eligibility and insurance arrangements.
This price was last updated in June 2025. Therefore, prices may have changed since then. For more information, contact our medical concierge, who can provide detailed guidance based on your specific situation.
FAQ
Could my endometrial polyp turn into cancer?
In most cases, endometrial polyps remain benign. Recent research shows that about 2.5–3% of endometrial polyps may develop into cancerous polyps, with the risk higher in postmenopausal women (potentially around 5%).
Can I prevent myself from getting an endometrial polyp?
Currently, there is no proven way to completely prevent endometrial polyps. However, you can reduce your risk by keeping a healthy weight, managing conditions such as high blood pressure and maintaining healthy hormone levels through your lifestyle choices.
Should I worry about endometrial polyps?
While most endometrial polyps are benign and manageable, it's important not to ignore any symptoms, particularly if you are in a higher-risk group. This includes being postmenopausal, being overweight, or taking certain medications such as tamoxifen.
What is the best treatment for endometrial polyps?
The most appropriate treatment depends on your individual situation, including your symptoms, age and whether you wish to conceive. For small polyps that are not causing any symptoms, a watchful waiting approach may be recommended, as some polyps resolve naturally.
Hormonal medications can help to balance your hormones and reduce symptoms. If surgery is necessary, hysteroscopic polypectomy is the preferred option – a minimally invasive procedure that enables your surgeon to remove polyps through a thin, lighted scope.
Can endometrial polyps be removed without surgery?
Yes, there are several non-surgical options available, particularly for smaller polyps. Hormonal treatments, such as progesterone therapy and the levonorgestrel intrauterine system, can help to shrink polyps and prevent them from coming back.
What is the difference between a polyp and a fibroid?
Although both are benign (non-cancerous) uterine growths, they are quite different. Endometrial polyps grow from the inner lining of the womb and are usually quite small, ranging from a few millimetres to a few centimetres in size. They are often attached by a slender stalk and can sometimes pass through the cervix.
Fibroids, on the other hand, grow from the muscle wall of the womb, can become much larger and typically remain embedded in the wall. Fibroids almost never turn cancerous, whereas polyps carry a small risk (about 2–3%) of developing into cancer over time, particularly after the menopause or if there is abnormal bleeding.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations for your specific conditions,schedule a consultation with our O&G specialist atThomson Women's Clinic and Cancer Surgery.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525

