Pregnancy is a joyful journey and full of hope. But it can also bring new challenges that you may not expect. One of these is gestational diabetes. If you’ve just heard this term, you may feel worried or uncertain. Don’t be. With the right care, most women go on to have smooth pregnancies and healthy babies. This guide will help you understand what it is, why it happens, and how you can manage it.
What is gestational diabetes?
Gestational diabetes is a type of diabetes that starts during pregnancy. It happens when your body cannot make enough insulin to keep blood sugar levels steady. Insulin is the hormone that moves sugar from your blood into your cells for energy. When insulin is not working well, sugar builds up in the blood.
Unlike type 1 or type 2 diabetes, gestational diabetes usually appears in the second trimester, between weeks 24 and 28. Most women do not have diabetes before pregnancy, and in many cases, blood sugar returns to normal after birth.
Causes of gestational diabetes
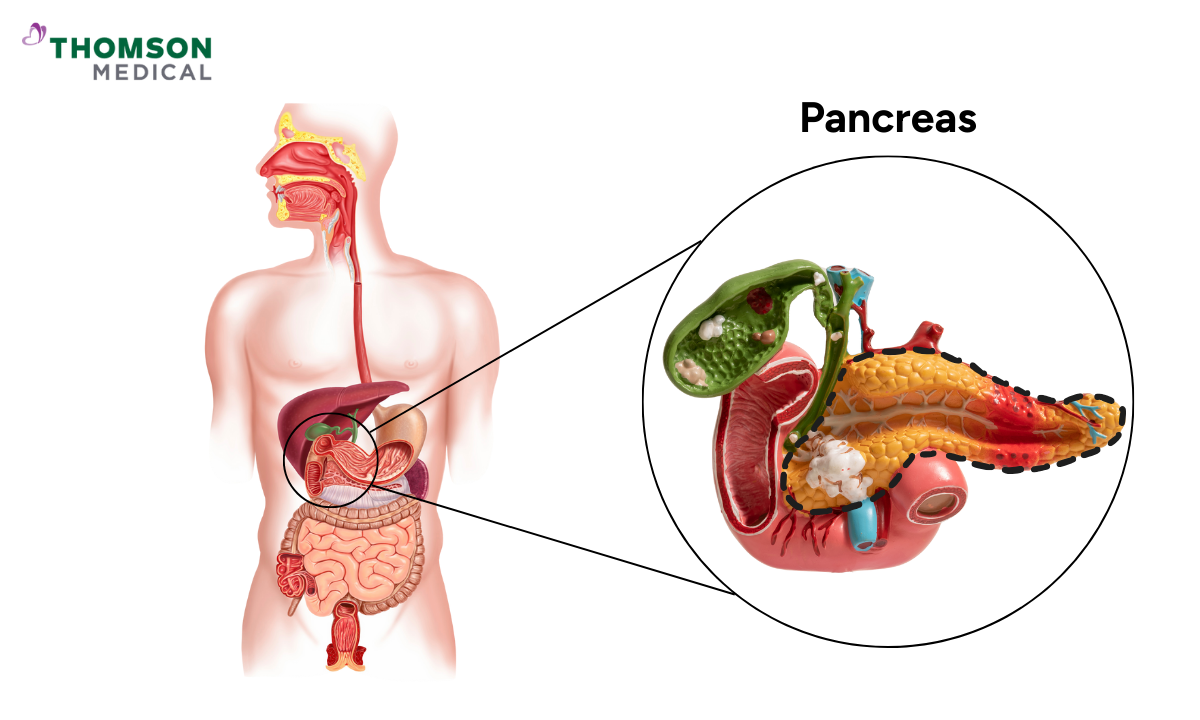
During pregnancy, your placenta produces hormones that help your baby grow. However, these hormones also make it harder for your body to use insulin properly. This is called insulin resistance.
If your pancreas can’t make enough insulin to overcome this resistance, blood sugar levels rise. That’s when gestational diabetes develops.
This doesn’t mean you had diabetes before pregnancy, and it doesn’t mean you will always have it afterwards, but it does mean you’ll need to take some steps to protect both yourself and your baby.
Who is more likely to get gestational diabetes?
Gestational diabetes can happen to anyone, but you may be more likely to get it if you have these factors:
Being over 25 years old
Being overweight before pregnancy
Having a close family member with type 2 diabetes
Experiencing gestational diabetes in a previous pregnancy
Giving birth before to a baby over 4 kg
Having polycystic ovary syndrome (PCOS)
Belonging to certain ethnic backgrounds, including African, Hispanic, Native American, South Asian, or East Asian
Having one or more of these risk factors does not mean you will definitely get gestational diabetes. This simply implies that your doctor will closely monitor your blood sugar levels.
Our specialists
Loading...
What are the symptoms of gestational diabetes?
Most women with gestational diabetes don’t notice symptoms, which is why routine testing is so important.
If you do notice signs, they may include:
Feeling unusually thirsty
Urinating more often
Feeling very tired
Blurred vision
Mild nausea
Because these signs can also be part of a normal pregnancy, regular screening is the best way to know for sure.
How can gestational diabetes affect you and your baby?
If blood sugar levels aren’t managed well, gestational diabetes can lead to the following complications:
For mothers, gestational diabetes increases the risk of:
Higher chance of preeclampsia
Possible need for a caesarean birth
Greater risk of type 2 diabetes later in life
For babies, possible risks include:
Larger birth weight, which may complicate delivery
Low blood sugar after birth
Breathing difficulties if born early
Higher risk of obesity or diabetes later on
However, careful management greatly reduces these risks. Many women with gestational diabetes go on to have healthy pregnancies and healthy babies, showing that good care really does make a difference.
How is gestational diabetes tested and diagnosed?
Most women are tested for gestational diabetes between 24 and 28 weeks of pregnancy. If you have higher risk factors, your doctor may test earlier.
The most common test is the Oral Glucose Tolerance Test (OGTT). You’ll drink a sweet liquid, and your blood sugar levels will be checked over the next few hours.
Different countries use slightly different cut-off values, but your care provider will guide you based on local practice. The table below shows the commonly used guidelines:
Guideline | Singapore Diabetes Diagnostic Criteria | WHO / IADPSG / ADA | NICE |
Fasting | ≥ 7.0 mmol/L (≥ 126 mg/dL) | ≥ 5.1 mmol/L (≥ 92 mg/dL) | ≥ 5.6 mmol/L (≥ 100 mg/dL) |
1-hour | Not used | ≥ 10.0 mmol/L (≥ 180 mg/dL) | Not used |
2-hour | ≥ 11.1 mmol/L (≥ 200 mg/dL) | ≥ 8.5 mmol/L (≥ 153 mg/dL) | ≥ 7.8 mmol/L (≥ 140 mg/dL) |
What happens if you are diagnosed?
Hearing the words “gestational diabetes” can feel overwhelming, but you are not alone, and you can manage it. With the right steps, it can be managed safely, and you’ll have support every step of the way.
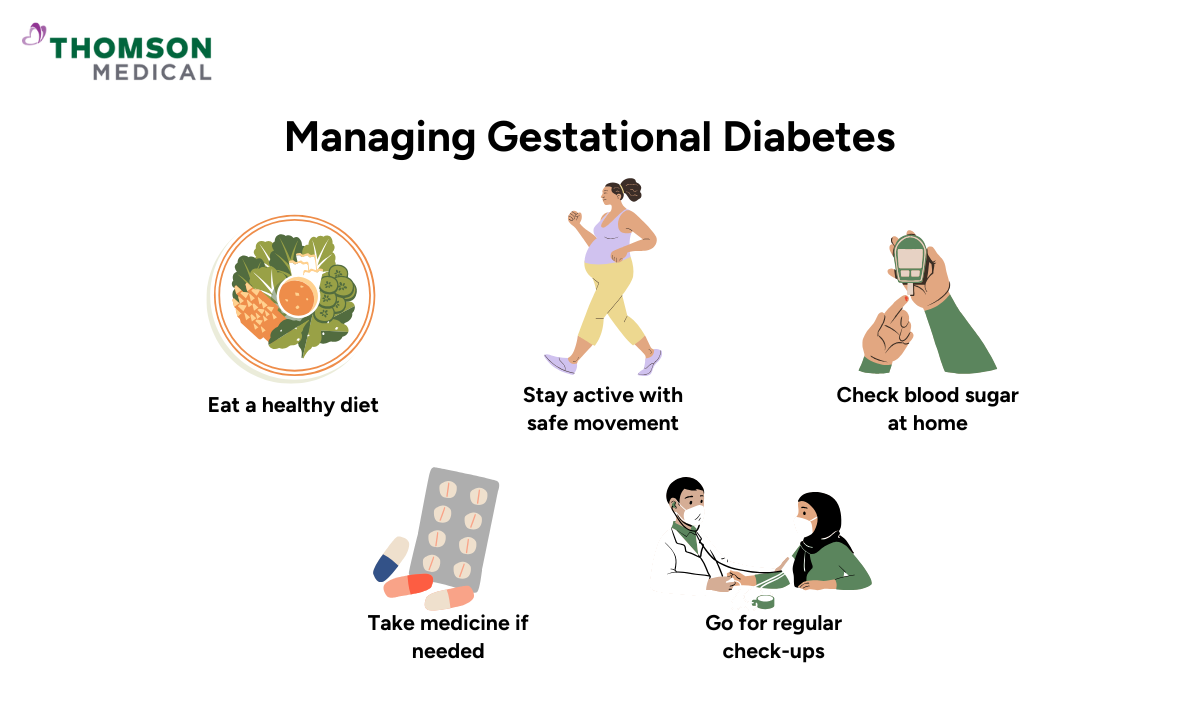
Your healthcare team will guide you to:
Adjust your eating habits
Stay active with safe pregnancy exercises
Monitor your blood sugar levels regularly
Use medication or insulin if needed
Attend regular check-ups
Most women control their blood sugar through lifestyle changes alone. With close monitoring, the outlook for both mother and baby is very positive.
You’re not alone in this journey. With regular check-ups and healthy choices, you and your baby can look forward to a safe pregnancy. If you have concerns, request an appointment with our specialist.
FAQ
How common is gestational diabetes?
Gestational diabetes is fairly common, and in Singapore, it affects about one in five pregnancies, which is higher than the global average of roughly 14%.
What foods should I avoid?
Try to limit sugary drinks, sweets, refined carbs like white bread, and large amounts of fruit juice.
Does water help lower blood sugar?
Drinking plenty of water is great for your overall health and helps keep blood sugar levels more stable, but it won’t bring high levels down on its own.
Can I still exercise safely?
Yes, you can. Choose gentle activities like walking, swimming, or yoga as these are generally safe during pregnancy, while high-impact sports or anything with a risk of falling are good to be avoided.
Can gestational diabetes be reversed?
It can’t be “reversed” during pregnancy, but lifestyle changes often keep it under control without medication.
How do I monitor my levels at home?
You can use a glucometer to check blood sugar levels at home. Most women check in the morning (fasting) and again one to two hours after meals.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical.Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
