Herpes simplex virus (HSV) is one of the most common infections that can affect anyone who is sexually active. Currently, there is no definitive cure available yet, but HSV can be managed effectively with proper care and treatment. Let’s take a closer look at what it is, how this virus spreads, what symptoms to look for, and how you can prevent the transmission.
What is HSV
HSV is a viral sexually transmitted infection (STI) that causes blisters or sores in different parts of your body, most often on the mouth or genital area.
There are two main types of HSV:
HSV-1 (Herpes simplex virus type 1):
HSV-1 causes oral herpes, commonly known as cold sores, around your lips and mouth.
It can spread to the genital area through oral intercourse, leading to genital herpes.
HSV-2 (Herpes simplex virus type 2):
HSV-2 primarily causes genital herpes with symptoms like painful sores or blisters on the genital area, anus, or thighs.
It’s usually transmitted through genital-to-genital contact, especially during unprotected sexual intercourse or with multiple partners. However, HSV-2 can also be spread to your mouth during oral intercourse.
Both types of HSV cause lifelong infections and can spread even without visible symptoms, through a process called asymptomatic viral shedding. Because of this, many people carry the virus without even realising it.
In some cases, HSV can also infect your eyes (herpes keratitis), your fingers (herpetic whitlow), and in rare cases, even your skin and nervous system.
Symptoms of HSV infection

Generally, HSV infections cause painful blisters that can break and form ulcers. These ulcers are covered by a scab as they heal.
The symptoms can vary depending on the type and the infected location:
Oral herpes (HSV-1):
You may notice small cold sores or fluid-filled blisters on or around your lips and mouth.
Before the sores appear, you can experience pain, itching, or tingling. These early warning signs are often described as a prodrome.
During your first outbreak, you may also have a fever or swollen lymph nodes.
Genital herpes (HSV-2):
Painful blisters or sores can develop on the genitals, buttocks, anus, or surrounding areas.
You can also experience vaginal itching or burning sensations and sometimes painful urination due to sores near the urethra.
Your first outbreak may resemble flu symptoms, such as fever, headache, or body aches.
Asymptomatic infection:
Many people with HSV may not have visible symptoms or may have mild ones that go unnoticed.
Knowing where HSV appears, as well as its symptoms, allows you to spot the infection and seek medical care promptly.
How HSV spreads
Understanding how HSV spreads can help you take steps to protect yourself and others. The virus is usually transmitted through direct skin-to-skin contact with infected areas, such as sores, blisters, or skin shedding. HSV can also be passed even when no visible sores are present.
HSV can spread in several ways, including:
Kissing:
HSV-1 can spread through kissing if your partner has cold sores.
Sexual contact:
HSV can be transmitted through oral, vaginal, and anal intercourse.
Mother to baby:
HSV can pass from mother to baby during childbirth, especially if the mother has an active outbreak at the time of delivery (neonatal herpes).
If you have concerns about herpes symptoms, or you just want to take a proactive approach to your sexual health, schedule an appointment with Thomson Medical for testing, diagnosis, and supportive care in a judgement-free environment.
Our sexual health specialist
Loading...
Prevention of HSV transmission
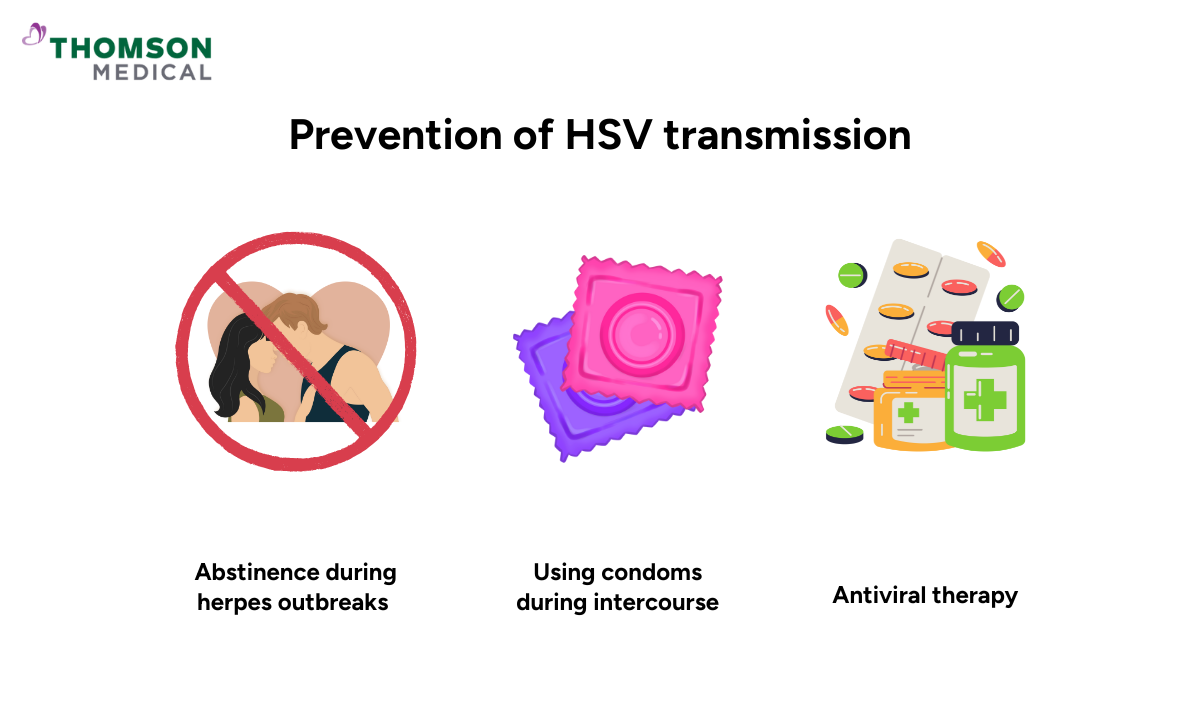
The good news is that there are effective ways to lower your chances of spreading or contracting herpes infection.
These include:
Abstinence during herpes outbreaks:
When sores or blisters are present, avoid direct skin contact, including kissing or sexual activity, with the infected area.
It’s important to remember that HSV can still spread due to asymptomatic viral shedding.
Condoms:
Using condoms during sexual activity can reduce your risk of HSV transmission. However, they don't fully eliminate it. Condoms only cover the genital areas, not other parts of the skin that may carry the virus.
Antiviral therapy:
Suppressive therapy with medications such as acyclovir, valacyclovir, or famciclovir can reduce the frequency and severity of herpes outbreaks, as well as decrease the transmission.
Treatment options for HSV
Depending on your symptoms, your doctor will recommend the most suitable treatment plan for you.
Treatment options may include:
Antiviral medications:
The same antiviral drugs used to prevent outbreaks are also used to treat active infections. They work by stopping the virus from multiplying, which helps shorten outbreaks, reduce their frequency, and lower the risk of passing it to others.
Over-the-counter treatments:
Some topical creams can help soothe pain and discomfort during an outbreak. However, they don't cure the infection.
Home remedies:
Applying cold compresses or using pain relievers, such as ibuprofen or paracetamol, can also help ease symptoms.
Treatment can manage symptoms and reduce outbreaks, but it doesn’t remove the virus from your body. HSV stays dormant and may reactivate from time to time.
Common triggers include stress, fatigue, illness, hormonal changes, or prolonged sun exposure. That’s why maintaining healthy habits and a lifestyle can make a difference in preventing recurrent outbreaks.
Without proper care, HSV can result in complications, especially if you have a weakened immune system.
When to see a doctor
While you can manage HSV on your own, you should seek medical advice if you:
Experience frequent or severe outbreaks
Have persistent pain
Have sores near your eyes
Are pregnant or plan to become pregnant
It’s best to consult your doctor if you experience any of these. Your doctor may use a blood test, a viral culture test, or a swab test to confirm the infection.
HSV is common and treatable, but that doesn’t mean you should ignore it. Seeking medical advice ensures you get the right diagnosis, treatment, and peace of mind.
Want to stay proactive about your sexual health? Schedule an appointment with Thomson Medical today, where our specialist can provide a herpes testing and personalised care to ensure your well-being.
FAQs
How long does it take for herpes symptoms to show up?
Usually, herpes symptoms appear about 2 to 12 days after exposure, most often around day 3 to 6. However, this can vary from person to person.
Does herpes go away?
No, herpes infections are lifelong. Once you are infected, the virus remains in your body in a dormant state in the nerve cells. It can be reactivated later, often triggered by stress, illness, or hormonal changes.
Can you donate blood if you have HSV?
In most cases, yes. HSV infection does not prevent you from donating blood. However, certain blood donation centres may have specific guidelines for people with active herpes lesions. It's always best to check with the donation centre.
What happens if HSV is left untreated?
Without proper treatment, HSV can lead to:
Complications:
While HSV is not typically life-threatening, untreated infections can lead to more frequent and severe outbreaks.
In some cases, it may cause complications like eye infections, urinary retention, or, rarely, meningitis (especially with HSV-2).
Emotional and psychological effects:
Living with visible herpes sores or the stigma surrounding herpes can lead to anxiety, depression, and stress.
Can you sleep with someone with HSV and not get it?
Yes, but there is still a risk of transmission. Using condoms, taking antiviral medications, and avoiding intercourse during outbreaks can help you reduce the chance of getting infected. However, these methods don't eliminate the risk. If your partner has HSV, it’s best to avoid sexual contact during outbreaks.
Can I live a normal life with HSV-1?
Yes, most people with HSV-1 live completely normal and healthy lives. The virus may occasionally cause cold sores, but you can manage outbreaks with the right care and medication. Having HSV-1 doesn’t define you, it’s a common viral infection that many people carry without it affecting their daily life.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique conditions, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
