Completing ovarian cancer treatment is a major milestone. Even so, it is very common for worries about recurrence to linger, especially as you begin follow-up care and adjust to life after treatment.
While no one can eliminate the risk entirely, there are practical steps that can support your long-term health. Staying connected with your care team, attending regular follow-up appointments, and understanding which factors matter most can help you feel more informed and confident as you move forward.
Why may ovarian cancer come back?
If ovarian cancer comes back, it's not because you did anything wrong, and it doesn't mean your treatment failed.
Ovarian cancer recurrence happens for biological reasons that are completely outside your control:
Tiny cancer cells can sometimes remain undetected and later grow.
Some cancer cells can adapt over time and survive chemotherapy.
Not all cancer cells behave the same way – some respond well to treatment, while others do not.
A small group of cells may have the ability to regenerate the tumour months or years later.
While the possibility of recurrence may feel concerning, it’s also a reminder of why staying connected with your doctor and tuning into what your body's telling you really matters.
What are the chances of recurrence?
This is probably one of the first questions on your mind, and it's completely understandable.
The likelihood of ovarian cancer coming back depends a lot on what stage it was when you were first diagnosed.
Stage 1: around 10–20%
Stage 2: around 30–40%
Stage 3–4: around 60–80%
These numbers are based on large groups of women, and they don't tell your individual story. Your own risk might be higher or lower depending on your tumour’s grade, your overall health, and how well you responded to treatment.
Risk factors for ovarian cancer recurrence
Certain factors may influence the likelihood of ovarian cancer recurrence, and having one or more of these does not mean the cancer will return.
Tumour-related factors:
Advanced ovarian cancer stage (3 or 4)
High-grade tumours
Extensive abdominal spread
Residual tumor after surgery
Patient-related factors:
BRCA1/BRCA2 or HRD mutations
Older age
Poor overall health or reduced immune function
Delayed diagnosis
Treatment-related factors:
Incomplete surgical debulking
Early discontinuation of therapy
Limited access to maintenance treatment
Risk factors are one part of the picture and are tools for planning care – not predictions. Many women with one or more of these factors go on to live in good health for many years.
If you recognise any of these factors and feel uncertain about what they mean for you, request a consultation with Thomson Medical. Our doctors can help you understand your individual risk and tailor a follow-up plan that feels clear and supportive.
Our ovarian cancer specialist
Loading...
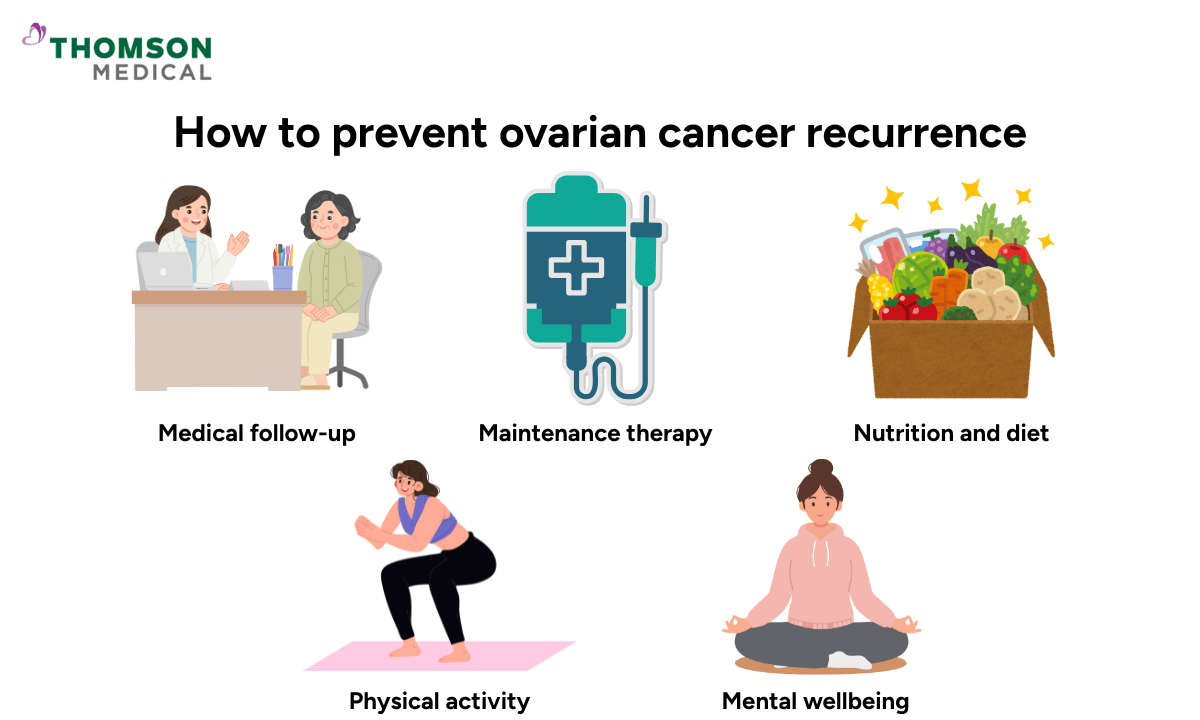
How to prevent recurrence of ovarian cancer
Living with the possibility of recurrence can be emotionally challenging, but you are not powerless. There are meaningful things you can do to lower your risk, stay on top of your health, and support your body as it continues to heal.
Medical follow-up
Regular check-ins with your doctor are an important part of your ongoing care. These follow-up appointments aren't just about watching for signs that cancer might come back. They're also about supporting your recovery, managing any lingering side effects from treatment, and giving you peace of mind as you move forward.
Your doctor will tailor your follow-up schedule based on your cancer type, stage, treatment response, and how you’re feeling.
But generally, the pattern looks something like this:
Every 3 months during the first 1–2 years after treatment
Every 6 months during years 3–5
Once a year after that
Follow-up appointments often include:
A review of any new or ongoing symptoms
Physical examination
CA-125 blood tests, if this marker was elevated at diagnosis
Imaging tests such as CT or PET scans, when you have new symptoms or blood tests raise concern
Many appointments are pretty straightforward. Your doctor listens to how you're feeling, answers your questions, and helps you address any concerns while they're still small.
Maintenance therapy
After you've been through surgery and chemotherapy, your doctor might recommend maintenance therapy. It does not cure ovarian cancer, but for many women, it can extend the time before the cancer returns.
Your doctor will likely bring up maintenance therapy if you have:
Advanced-stage ovarian cancer
BRCA1/BRCA2- or HRD-positive tumours
Responded well to initial chemotherapy
The type of maintenance therapy depends on the medication used:
PARP inhibitors:
These are pills you take at home every day – no hospital visits required.
Anti-angiogenic therapy:
It involves going to the hospital for infusions, usually every few weeks.
Immunotherapy:
Immunotherapy is offered in specific cases and is also given through an intravenous infusion at the hospital.
Whether it's right for you depends on your specific tumour biology and your overall health – it's a personalised decision you'll make together with your care team.
Nutrition and diet
Eating well after ovarian cancer treatment isn't about following strict rules or achieving some kind of perfect diet. It's about nourishing your body, supporting your recovery, and giving yourself the energy you need to heal.
Food to support cancer healing may include:
Anti-inflammatory food:
An anti-inflammatory eating pattern may help support immune function and overall health.
This includes colourful fruits and vegetables, whole grains, and lean proteins.
Omega-3 fatty acids:
Healthy fats play a role in reducing inflammation.
Omega-3 fatty acids are found in fatty fish, such as salmon, sardines, and mackerel, and in walnuts, chia seeds, and flaxseeds.
High fibre:
A fibre-rich diet supports digestion and may help regulate immune responses.
Legumes, whole grains, vegetables and fruits are good choices for you.
You don't need to eliminate anything, but it can help to enjoy certain foods in moderation rather than making them staples. This includes red and processed meats, highly processed foods, and sugary drinks or refined sweets.
And it's okay to enjoy foods you love. Eating well isn't just about what's on your plate – it's also about eating with less fear and more ease. Food should nourish you, but it can also bring you comfort and joy. Both of those things matter.
Physical activity
Regular physical activity can help reduce fatigue, support immune function, improve insulin sensitivity, and lower inflammation. All of which are important during your recovery and long-term health.
If you're feeling tired or out of shape right now, that's completely understandable – and it means starting small. Even short, gentle movements, such as walking, light household activities, or gentle stretching, can make a real difference.
As your energy starts to come back – and it will – you can gradually add in light strength work. Bodyweight exercises, yoga, Pilates, or Tai Chi are all great options that help rebuild muscle and support your bone health without overwhelming your system.
Emotional and mental wellbeing
The fear that cancer could come back can quietly follow you around – during routine check-ups, when you notice a new symptom, or even on days when everything seems to be going well.
Your emotional health plays a meaningful role in how effectively you can manage the risk of recurrence.
When anxiety, depression, or unresolved stress are left to simmer under the surface, they can affect your sleep, your immune function, and even your ability to stay engaged with your follow-up care.
In contrast, women who feel emotionally supported are more likely to:
Attend regular follow-up appointments
Notice and report symptoms early
Maintain healthy routines around diet, movement, and rest
Adhere consistently to maintenance therapy when prescribed
Mindfulness or meditation practices and support groups for gynaecologic cancer survivors can help you manage chronic stress and feel more grounded. And sometimes, psychiatric care and medication are important parts of the picture too. There's no shame in needing that support – it's a sign that you’re taking your recovery seriously.
Caring for your emotional and mental health isn't something separate from caring for your body. It's an active, essential part of staying well after ovarian cancer.
If you’d like guidance on follow-up care, maintenance therapy, or lifestyle support after ovarian cancer treatment, our O&G specialists at Thomson Medical are here to walk alongside you. Request an appointment today.
FAQ
When should I see a doctor after ovarian cancer treatment?
You should see a doctor promptly if you experience:
Persistent bloating
Abdominal or pelvic pain
Shortness of breath
New bowel or urinary changes
Sudden weight loss
Ongoing fatigue
Do not wait for your next scheduled follow-up if these symptoms appear.
Can lifestyle changes truly reduce recurrence?
Lifestyle changes cannot replace medical treatment, but they can improve your immune function, reduce inflammation, help your body tolerate treatment better, and enhance overall quality of life.
What foods may help prevent recurrence?
No food can prevent recurrence on its own, but a balanced diet may support recovery. Helpful choices include:
Cruciferous vegetables, such as broccoli and cabbage
Berries and citrus fruits
Legumes
Whole grains
Green tea
Spices like turmeric and ginger
How does stress affect recurrence?
Chronic stress can raise cortisol levels, suppress immune surveillance, and increase inflammation in the body. Managing stress is therefore an important part of preventing ovarian cancer recurrence.
Can recurrent ovarian cancer be cured?
Recurrent ovarian cancer is usually not curable, but it is often manageable as a chronic condition. With ongoing treatment and follow-up care, many women continue to live long, meaningful lives.
How do I know if I’m a candidate for maintenance therapy?
Your doctor will assess your cancer stage, response to initial treatment, and tumour biology (including BRCA or HRD status). Maintenance therapy is discussed only if the potential benefits outweigh the risks for you.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
For more information, contact us:
Thomson Fertility Centre
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Thomson Women's Clinic
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
