Hearing that surgery is part of ovarian cancer treatment can bring up many questions and concerns. It is common to imagine a single standard operation, but in reality, there are several types of ovarian cancer surgery, each chosen based on the stage of the cancer and your individual needs.
Some surgical approaches aim to preserve fertility, while others are more extensive and focused on removing as much cancer as possible.
Understanding the different types of surgery, how doctors decide which option is right for you, and what recovery may involve can help you feel more prepared and supported as you plan the next steps in your care.
Who is most likely to develop ovarian cancer?
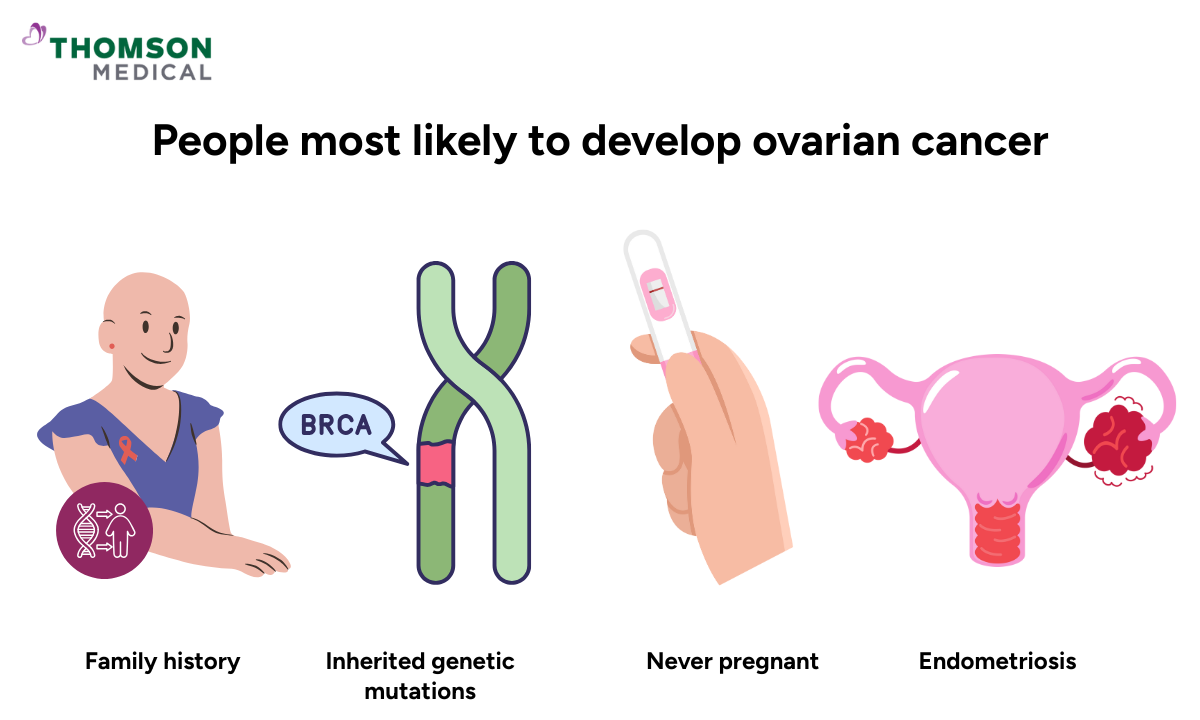
Ovarian cancer can affect anyone with ovaries, but it's most common in women over 50, particularly after menopause.
While age plays a role, these risk factors can also increase your chances:
Family history of ovarian, breast or colorectal cancer
Inherited genetic mutations (such as BRCA1 or BRCA2)
Never pregnant
Long-term oestrogen exposure
While ovarian cancer is more common in older women, it's important to know that younger women can develop it too. If you're experiencing symptoms or have concerns, don't dismiss them because of your age.
Ovarian cancer specialist
Loading...
Why is surgery needed for ovarian cancer?
Surgery does several important things when you're diagnosed with ovarian cancer. It helps confirm the diagnosis, shows doctors how far the cancer has spread, removes as much of it as possible, and can ease the symptoms you're dealing with.
For most women, surgery is the first step in treatment. The results help your medical team create a treatment plan that's right for your specific situation, giving you a better chance of recovery.
What are the main types of ovarian cancer surgery?

The type of surgery you'll have depends on your own individual circumstances. Your doctors will consider factors such as the stage of your cancer, where it has spread, and what matters most to you.
Initial surgery
If your doctor suspects ovarian cancer, you'll likely have surgery to confirm it and assess the extent. This procedure helps your doctor:
Remove suspicious ovarian masses
Take tissue samples (biopsy) to confirm whether cancer is present
Check how far any cancer cells have spread in your body
Your doctor may need to remove one or both ovaries, your fallopian tubes, lymph nodes and nearby tissue.
If your cancer is caught early and having children is important to you, it's worth talking to your doctor about fertility-sparing surgery. This can be an incredibly difficult conversation to have, but your doctor understands how much this is important to you. Whether this option is possible depends on your individual circumstances, including the stage and type of your cancer.
Debulking surgery
Debulking surgery (also called cytoreductive surgery) removes as much cancer as possible from your body. Doctors often recommend this for women with advanced ovarian cancer.
Your surgeon may need to remove:
Both ovaries and fallopian tubes
Uterus (a procedure called hysterectomy)
Omentum (a layer of fatty tissue that covers your abdominal organs)
Portions of the bowel, bladder, or diaphragm if cancer has spread to these areas
The surgery can be extensive, but removing more cancer often helps your body respond better to chemotherapy.
Chemotherapy port placement
If chemotherapy is part of your treatment plan, your doctor may recommend having a chemotherapy port placed under your skin, usually in your chest. This small device connects to a large vein and makes treatment much easier.
Having a chemotherapy port means:
You won't need repeated needle sticks for each treatment
Less discomfort during treatment
Your veins stay protected from damage over time
This is a minor procedure that may be done during your main surgery or separately, depending on your treatment plan.
Ovarian cancer surgery decisions can feel overwhelming, but you don’t have to navigate them alone. Request an appointment with Thomson Medical to discuss your surgical options in detail, understand what each procedure involves, and plan the approach that suits your diagnosis.
What happens before ovarian cancer surgery?
Before your operation, you'll go through several preparations. You'll have several tests:
Pelvic examination to check for abnormalities
CA-125 blood test to measure tumour markers
Medical clearance and anaesthesia evaluation
Before the surgery, your doctor will ask you to:
Stop certain medications such as blood thinners
Avoid eating and drinking for several hours beforehand
Arrange for someone to help you at home during recovery
Your doctors will discuss fertility preservation, recovery time and what treatment might follow. Don't hesitate to ask about anything that's worrying you, whether it's how the surgery works, what your recovery will look like, or how it might affect your daily life.
What to expect during recovery
Your recovery depends on how extensive your surgery was and whether it was done laparoscopically (through small incisions) or through open abdominal surgery.
After major surgery, you can expect to:
Stay in the hospital for several days
Receive pain management and gradually move around to aid healing
Limit lifting and strenuous activity for several weeks
Attend follow-up visits to discuss pathology results and next steps
Full recovery may take several weeks to months, especially after extensive debulking surgery. This can feel frustratingly slow, but it's completely normal. Your body has been through a lot and needs time to heal properly. Don't feel pressured to rush back to your usual routine before you're ready.
What side effects might you experience?
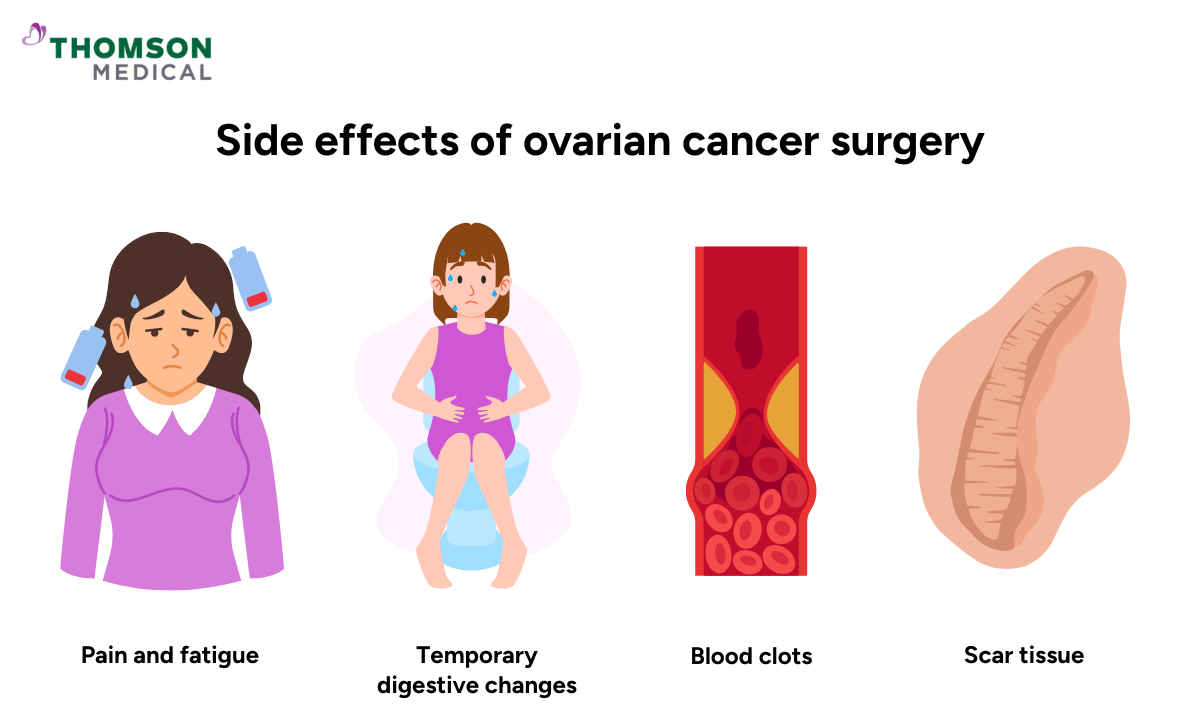
After ovarian cancer surgery, you'll likely experience some side effects. Knowing what's normal can help you feel more prepared and know when to reach out to your doctor.
Surgery affects everyone differently, but common side effects include:
Pain and fatigue
Temporary changes in your digestion such as diarrhea or constipation
Small risk of infection or blood clots
Scar tissue (adhesions) as part of the healing process
Early menopause if both ovaries are removed
Changes to your fertility and hormonal balance
If both ovaries are removed, you may experience symptoms such as hot flushes, changes in bone density and mood changes.
Most side effects ease with time, though some may need ongoing care. Your doctor can help ease these symptoms through treatment and lifestyle changes that suit you. Support is available throughout your treatment, and with the right care, many women maintain a good quality of life during and after recovery.
Recovery can look different for everyone, and support makes a real difference. Request an appointment with Thomson Medical to review your post-surgery symptoms, discuss menopause or fertility concerns, and get a personalised plan to manage side effects as you heal.
FAQ
What are the stages of ovarian cancer?
Ovarian cancer is staged from I to IV. Stage I is confined to one or both ovaries. Stage II has spread to nearby pelvic organs. Stage III involves spread to the abdominal cavity or lymph nodes. Stage IV means cancer cells have spread to distant organs like the liver or lungs.
What can I expect if I have ovarian cancer?
A diagnosis often involves imaging tests such as a transvaginal ultrasound, followed by surgery and chemotherapy. You'll also have access to emotional support and symptom management. Your treatment plan will be based on your individual situation.
What is the ovarian cancer survival rate?
Ovarian cancer survival rates depend on the stage at diagnosis. Early-stage ovarian cancer has higher survival rates. Advanced-stage disease is more challenging to treat. Modern therapies continue to improve outcomes, and early diagnosis with optimal surgery can make a real difference.
Can I prevent ovarian cancer?
There's no certain way to prevent ovarian cancer, but some may lower your risk factors. These include using oral contraceptives, pregnancy and breastfeeding, and risk-reducing surgery for people with BRCA mutations. If you have a strong family history, genetic counselling may help you understand your options.
How is the type of ovarian cancer surgery determined?
Your surgical plan depends on several factors. These include the cancer's stage and spread, the tumour type and grade, and your age and overall health. Your desire to preserve fertility and how you've responded to any prior treatments also play a role.
A gynaecologic oncologist usually leads this planning. They'll explain which treatment options are suitable for your case, outline the benefits and risks of each, and work with you to decide on the best approach for your situation.
How does ovarian cancer surgery impact fertility and hormonal health?
If both ovaries are removed, your reproductive system is affected, and you'll experience infertility and immediate menopause. In carefully selected early-stage cases, surgery may preserve one ovary and the uterus. Hormonal changes can cause symptoms like hot flushes, bone loss and mood changes. These can often be managed with medical support.
How long does it take to recover from ovarian cancer surgery?
Recovery time varies based on the type and extent of surgery. After minimally invasive surgery, you might feel better within a few weeks. More extensive operations can take several months for full recovery. Your surgical team will give you specific guidance based on your procedure.
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment