Are you experiencing persistent lower back pain that's affecting your daily life? You might assume that it's simply due to different lifestyle factors, such as incorrect posture or a sedentary lifestyle. However, it can actually be caused by lumbar disc degeneration, also known as degenerative disc disease (DDD).
Don't be alarmed by its name, though. Despite what it sounds like, DDD isn't actually a disease. It's a common condition that occurs naturally with ageing, especially if you're over 40 years old. It happens when the cushions between your vertebrae (backbone) in the lumbar spine (lower back) experience wear over time.
When these cushions deteriorate, the bones can rub together, causing pain and limiting your mobility. Your doctor can assess this condition by performing a lumbar degenerative disc disease MRI scan to pinpoint the source of your pain.
What is a lumbar degenerative disc disease MRI scan?
A lumbar DDD MRI (magnetic resonance imaging) scan is a non-invasive medical imaging technique that produces detailed images of your lumbar spine. It enables your doctor to evaluate the different structures present in this area, such as the cushions between your vertebrae (intervertebral discs or spinal discs), vertebrae, and spinal cord.
This imaging technique is the preferred option for assessing lumbar disc degeneration, as it uses strong magnets and radio waves, unlike X-rays or CT scans which use radiation. This makes it safe for repeated assessments when necessary and provides more detailed images of soft tissues than other imaging methods.
MRI scans can provide two- or three-dimensional images from multiple angles, helping your healthcare provider to diagnose, monitor, and guide treatment for various spinal conditions related to lumbar disc degeneration.
When will your doctor recommend a degenerative disc MRI?
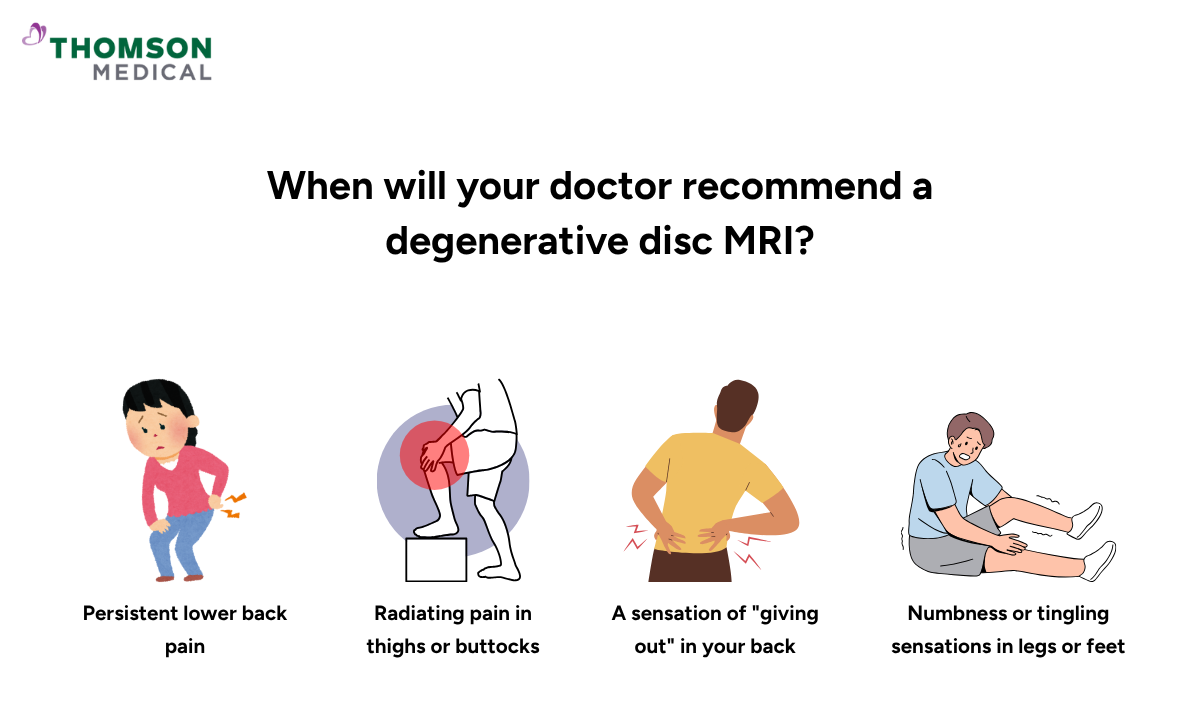
Your doctor may recommend a spine MRI scan if they suspect an issue with your lower back and require a definitive diagnosis. This type of imaging scan is essential to decide the next step of treatment when conservative treatments have not provided relief.
Your doctor may recommend an MRI scan if you experience symptoms of DDD, such as:
Persistent lower back pain
Radiating pain that extends to your thighs, buttocks, or down your legs (sciatica)
Numbness or tingling sensations in your legs and feet
A sensation of your back "giving out"
Pain in your back that worsens when you bend, twist, or lift but improves when you lie down or change position
This diagnostic imaging test can also help to assess whether other conditions are contributing to the pain, such as fractures, nerve root compression, or other inflammatory conditions.
What can a degenerative disc MRI scan tell you?
A magnetic resonance imaging scan is used by your doctor to assess your lumbar spine and intervertebral disc condition. It can also provide valuable information about the spine condition, such as:
Disc height and hydration:
Your intervertebral discs have a soft core that contains water. That's why healthy intervertebral discs appear bright on MRI due to their fluid content. However, as you get older, they naturally lose some water.
As a result, the intervertebral discs get thinner and don't provide as much shock absorption as they used to. These degenerated discs will also appear darker during the evaluation, sometimes called "black discs".
Bulging discs:
MRI can identify disc protrusions (also known as disc herniation) that may be pressing on nearby nerves, causing pain and other symptoms.
Bone spurs:
This medical imaging test can detect small bony growths that form when the body attempts to stabilise the spine due to intervertebral disc degeneration.
Spinal stenosis:
Spinal stenosis occurs when the spinal canal narrows due to disc degeneration, bone spurs, or other causes. This makes it unable to accommodate the spinal cord and nerves, leading to nerve compression.
Although lumbar degenerative disc disease is part of the natural ageing process, some people may experience less pain than others. This is why your doctor will take into account your medical history, the results of a previous physical exam, and spine MRI scan results to make a definitive diagnosis.
If you are experiencing persistent back pain accompanied by other symptoms, such as weakness, an MRI scan can help identify the underlying cause. Schedule an appointment with Thomson Medical for an evaluation and personalised treatment plan.
How do I prepare for a degenerative disc disease MRI?
Preparing for a spine MRI scan is relatively straightforward, and your healthcare provider will give you instructions to help you prepare. This imaging test is performed by a radiology technologist, a professional who is trained and certified to operate the MRI equipment.
Here are some general guidelines to help you prepare:
Clothing:
Before the scan, you may be asked to change into a hospital gown and remove any jewellery, dentures, watches, or other metal objects that might interfere.
Metal objects:
Inform the technologist if you have any metal implants or other medical devices, such as pacemakers, as these can heat due to the magnetic fields of the MRI scanner and pose a safety risk.
Medications:
Bring a list of any medications you are taking, as some may need to be temporarily stopped before the procedure.
Contrast dye:
If your doctor orders a contrast-enhanced MRI, you may need to be injected with a contrast dye (gadolinium) to improve the visibility of the soft tissue around your lumbar vertebrae.
However, if you have a kidney condition, you should inform your healthcare provider. They may perform a blood test prior to the scan to evaluate your kidney function and assess whether it is safe to use a contrast dye.
Pregnancy:
If you are pregnant or think you might be, tell your doctor or technologist before the scan.
If you are anxious about being in enclosed spaces (claustrophobia), talk to your healthcare provider. You may be given a sedative before the procedure to help you relax during the scan.
Please don't hesitate to ask your doctor or technologist any questions you may have. They will be delighted to answer your questions and ensure that your MRI scan goes smoothly and safely, giving you peace of mind.
How does the test work?
Following the preparation stage above, the procedure will begin and usually lasts 30 to 90 minutes. During the scan, you can expect the following:
Before the scan, if a gadolinium contrast agent is needed, it will be injected into your arm vein through an IV.
You will then be asked to lie on your back on a table which slides into a large, tubular machine that looks like a tunnel.
When the scan starts, the MRI machine will make loud tapping or thumping sounds. You'll be given earplugs or headphones to wear before the procedure to protect your hearing.
During the scan, it's important to stay still to ensure clear images.
The MRI radiologist will be in another room, but you can use the intercom to contact them if there are any issues.
If you didn't have a sedative for the MRI scan, you will not need a recovery period. You can immediately return home and resume your normal activities. However, if you have had a sedative for the scan, you will need to recover from its effects before you can go home safely.
If your scan requires a contrast dye, you will usually need to drink plenty of fluids to help flush the dye out through your urine.
What to expect after the procedure
A radiologist will analyse the images and send a signed report to your doctor. Your doctor will then share the results with you and discuss everything with you.
If a follow-up examination is required, your doctor will explain why, which may include further evaluation using different imaging methods or monitoring changes over time. Follow-up scans are often recommended to assess the effectiveness of treatment or to monitor any changes in your condition.
If you would like more information about lumbar degenerative disc disease MRI scans, schedule a consultation with Thomson Medical. Our specialists can explain this procedure to you in more detail and provide a tailored treatment plan.
What are the potential risks of this medical imaging test?
Although MRI scans are generally safe, there are some potential risks you need to be aware of:
The loud noise produced by the MRI scanner can be uncomfortable, particularly if the scan takes more than an hour
If you're someone who gets anxious in small spaces (claustrophobia), you might feel uneasy during your MRI scan.
If your scan requires a contrast agent, some people may rarely experience an allergic reaction to gadolinium. Symptoms may include nausea, a metallic taste in the mouth, and an allergic reaction such as rashes, flushed skin, and shortness of breath.
People with metal implants, pacemakers, or other devices may need special precautions or can't have an MRI.
You may feel nervous or stressed while lying still in the MRI machine for long periods of time
FAQ
Does degenerative disc disease show on MRI?
Yes, an MRI scan can clearly detect disc degeneration. It can identify various signs of degenerative disc disease, including disc thinning and dehydration (which appear as darker "black discs"), as well as bulging and disc herniation.
Associated spinal changes, such as bone spurs and spinal stenosis, can also be identified during the evaluation of the lumbar disc.
Preventing degenerative disc disease
Although disc degeneration is a natural part of ageing, you can take steps to slow its progression by adopting these healthy lifestyle habits:
Maintain an ideal body weight to reduce stress on your spine
Exercise regularly to strengthen core and back muscles that support your spine
Practice good posture when sitting, standing, and lifting
Avoid smoking, as it reduces blood flow and nutrients to your discs, which is important for maintaining disc hydration
Use ergonomic workspaces to minimise spinal strain during daily activities
What are the 4 stages of spinal degeneration?
According to current research, there are four stages that your spine goes through as degenerative disc disease progresses, which include:
Stage 1:
Your discs start to lose water and develop small tears on their outer wall, leading to mild back pain.
Stage 2:
The soft centre of your disc starts pushing against the weakened outer wall, creating a bulge. Your pain becomes more persistent and may travel down to your arms or legs.
Stage 3:
The outer layer of your disc tears open, allowing the inner material to leak out and press on nearby nerves. This can cause severe pain, and you may experience numbness or weakness in your limbs.
Stage 4:
Your discs lose significant height, your body forms bone spurs to try stabilising your spine, and you experience chronic pain with limited freedom of movement.
Remember, not everyone progresses through all four stages, and the timeline varies greatly from person to person. Your doctor can help determine which stage you're in and create the best treatment plan for your specific situation.
How do you treat degenerative disc disease?
Most people with degenerative disc disease find relief through non-surgical treatments. Treatment approaches include:
- Conservative care:
- Physical therapy to strengthen core and back muscles, improve flexibility, and reduce pain through targeted exercises
- Medicines, such as non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids and nerve pain medications
- Pain management plans such as heat/cold therapy, epidural steroid injections, and lifestyle modifications
- Surgical options (for severe cases where conservative treatments fail):
- Spinal fusion to stabilise the spine using bone grafts
- Artificial disc replacement to maintain motion while replacing the damaged disc
- Dynamic stabilisation using interspinous spacers to prevent nerve compression
Can I live with degenerative disc disease?
Yes, it is possible to live well with degenerative disc disease. With conservative treatment, lifestyle adjustments, and appropriate medical care, your pain can be managed, and your quality of life can improve.
While the timeline varies from person to person, consistent treatment and self-care can lead to noticeable symptom relief.
How serious is degenerative disc disease?
The severity of degenerative disc disease can vary from person to person. While it can cause mild to severe pain, it may also lead to complications such as spinal stenosis or nerve compression.
However, early intervention with appropriate treatment can help manage symptoms and slow their progression.
The information provided is intended for general guidance only and should not be considered medical advice. To get personalised recommendations based on your medical conditions, schedule a consultation with Thomson Medical.
For more information, contact us:
Thomson Medical Concierge
- 8.30am - 5.30pm
- WhatsApp: 9147 2051
Need help finding the right specialist or booking for a group?
Our Medical Concierge is here to help you. Simply fill in our form, and we'll check and connect you with the right specialist promptly.
Notice:
The range of services may vary between Thomson clinic locations. Please contact your preferred branch directly to enquire about the current availability.
Get In Touch