If you've never heard the term before, hearing that you have a complex ovarian cyst can be quite concerning. Many women in this situation will naturally feel anxious and have questions about what it means for their health.
In most cases, complex ovarian cysts are not harmful and can be managed with the proper treatment. Learning what the diagnosis means and understanding when monitoring or treatment is needed can help ease uncertainty and support your peace of mind.
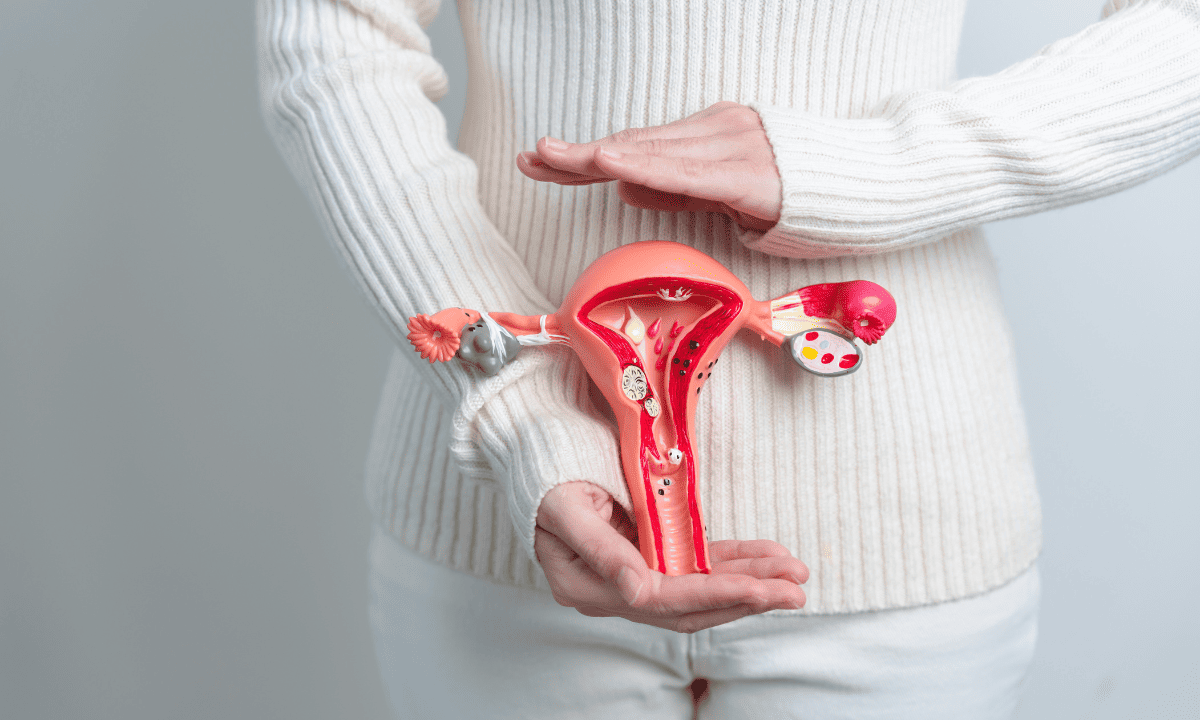
What is a complex ovarian cyst?
A complex ovarian cyst is a type of ovarian cyst that contains more than just clear fluid alone. On an ultrasound, it looks different from a simple cyst because it may contain:
Blood
Solid tissues
Thick fluid
Internal walls (septations), thin dividing walls that form inside the cyst
You may find that word “complex” concerning. However, keep in mind that many complex cysts do not cause any serious harm. Understanding these differences can help you make sense of your results and ensure you get the right level of follow-up without unnecessary anxiety.
What causes complex ovarian cysts?
There are several reasons why you may develop a complex ovarian cyst, many of which are part of your body’s normal rhythm:
Haemorrhagic cysts:
A small amount of bleeding can happen inside a cyst during your normal ovulation.
Endometriomas:
These are linked to endometriosis and contain older blood that has built up over time.
Dermoid cysts:
These are benign growths that can contain tissue like fat or hair.
They may sound worrying, but they’re usually harmless.
Natural hormonal shifts:
Changes in your hormone levels can sometimes cause a cyst to linger longer than expected.
Normal ovarian activity:
A normal cyst may develop more complex features as part of its natural life cycle.
While learning about all these different cysts may feel concerning at first glance, most of them have non-cancerous causes, especially in younger people who have naturally higher hormonal activity.
Who is at risk?
You can develop a complex ovarian cyst at any point once you begin ovulating, which usually starts after your first period between the ages of about 11 and 14. However, you are also more likely to be at risk if:
You are in your reproductive years, usually from your teens through to your late forties
Your periods are unpredictable
You are living with conditions like endometriosis or polycystic ovary syndrome (PCOS)
Your body has had ovarian cysts before
While complex cysts can show up at any age, the chance of a cancer-related cyst is very low, especially if you’re a teenager or young adult. For most people in this age group, these cysts are related to normal hormone activity rather than anything serious. In many cases, they are simply monitored and settle on their own without the need for invasive treatment.
If you happen to have any of these risk factors, you can schedule a consultation with Thomson Medical today to get a proper evaluation and personalised guidance.
What are the symptoms of a complex ovarian cyst?
In many cases, a complex cyst causes no symptoms at all. Your doctor may only identify it during a scan done for another reason. When symptoms do show up, your body may give you a few signs to pay attention to:
You may experience ongoing bloating or heaviness in your lower abdomen or pelvic area
Your periods have noticeable changes in menstrual bleeding or cycle pattern
You feel pain when you move, do exercise, or daily activity
You can also encounter sudden, severe pain if a cyst ruptures or twists (ovarian torsion)
If your symptoms start to feel different or more intense, trust what your body is telling you and reach out to a healthcare provider early. Speaking to a medical expert can help you know what is normal, rule out anything serious, and answer the questions that may be playing on your mind.
Our gynaecologic oncology specialist
Loading...
How are complex ovarian cysts diagnosed?
To give you the most accurate and reassuring diagnosis possible, your doctor will use a combination of physical assessments and clear imaging.
Medical history:
Your doctor will discuss your symptoms, cycle, and any history of hormonal or gynaecological conditions.
Pelvic exam:
You will receive a physical pelvic exam to help identify any specific areas of tenderness or thickened areas.
Pelvic ultrasound:
This is the primary test, as it provides your doctor the most detailed view of your cyst, including solid areas, septations, and the overall size and shape of your cyst.
Sometimes, your care team may arrange a follow-up scan in 6 to 8 weeks to check whether the cyst is changing or shrinking. Waiting can feel unsettling, but this approach is often taken because many cysts improve on their own over time. The scan is there to help you feel confident that your recovery is being carefully monitored.
If you suspect a complex ovarian cyst, schedule a consultation with a doctor at Thomson Medical to get an accurate diagnosis and personalised care plan.
What are the treatment options for complex ovarian cysts?

Not every complex ovarian cyst needs surgery. The right approach for you depends on your age, your symptoms, and what your ultrasound shows. Your care team will work with you to choose a plan that feels appropriate and safe for your body.
Careful monitoring (watchful waiting)
If your cyst doesn’t show signs of concern, your doctor may suggest keeping an eye on it rather than stepping in straight away.
Attend follow-up ultrasounds to help check the behavior of your cyst
Pay attention to any changes in your body, including pelvic pain or cycle changes
Apply warm compresses, heat packs, or pain relief recommended by your doctor to ease day-to-day discomfort
This approach allows your body time to settle while keeping you safe and well-supported.
Hormonal therapy
In some cases, your doctor may recommend hormonal treatment to help support your cycle and reduce the chance of new cysts forming.
Hormonal contraception may be used to help regulate your menstrual cycle
Stabilising hormone levels can lower the likelihood of cysts coming back
This approach is often considered if you are struggling with irregular periods
Hormonal therapy doesn’t shrink existing cysts in every case, but it can play an important role in preventing future complications and helping your body feel more stable over time.
Surgery
Surgery is usually considered only when your cyst is causing persistent symptoms or shows features that need closer evaluation, including:
Your cyst is large
It’s causing ongoing or worsening pain
It doesn’t shrink over time
It has features on imaging that need closer evaluation
There’s a risk of ovary twisting
When surgery is needed, it is most often done using minimally invasive techniques, with care taken to preserve as much healthy ovarian tissue as possible.
If your doctor mentions surgery, it does not automatically mean something serious. Most people diagnosed with a complex ovarian cyst do not need surgery at all, as many cysts can be safely monitored or resolve on their own.
Surgery is usually considered only in a small number of cases, such as when your symptoms are severe, the cyst is not improving, or there is uncertainty about the diagnosis. This is done to keep you safe rather than because something is wrong.
FAQ
What’s the difference between a simple cyst and a complex cyst?
A simple cyst is filled only with clear fluid, a bit like a small blister. A complex cyst has more going on inside, such as blood, thicker fluid, solid areas, or internal walls. Because of these extra features, your doctor will usually want to keep a closer eye on it, not because it’s dangerous, but to make sure it behaves as expected.
Should I worry about cancer if my cyst is called “complex”?
It’s completely normal to feel anxious when you hear the word “complex”, but in most cases, the answer is no. Most complex cysts turn out to be benign conditions like dermoid cysts or endometriomas. Your doctor will monitor them carefully simply to rule out rare problems and give you peace of mind.
What size complex ovarian cyst usually needs surgery?
There’s no single size that automatically means surgery. Doctors may start to consider removal if a cyst grows beyond about 5 to 7 cm, but size isn’t the only factor. How you’re feeling, whether the cyst is changing, and what it looks like on follow-up scans all matter just as much.
What does pain from a complex ovarian cyst feel like?
Everyone experiences it differently. You might notice a dull, heavy ache low in your abdomen or a sharper pain on one side of your pelvis. Some people feel it more around their period or during physical activity, while others only notice it occasionally.
Who is more likely to develop these cysts?
If you ovulate, you can develop an ovarian cyst. You may be more prone if your periods are irregular, if cysts run in your family, or if you live with conditions like PCOS or endometriosis that affect hormone balance.
Can a complex cyst go away on its own?
Yes, some can. Certain types, such as haemorrhagic cysts, often shrink and resolve naturally over one or two cycles. Others, like dermoid cysts, tend to stay and may eventually need surgical removal. Your care team will help you understand which type you’re dealing with and what that means for you.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment