Pelvic pain is a common health issue that affects both men and women. While it’s sometimes temporary and harmless, in other cases it may be a sign of infections, reproductive health issues, or even emergency conditions. To help put your mind at ease, let's explore the causes of pelvic pain and when you should seek help.
What is pelvic pain?
Pelvic pain is discomfort in the lower abdomen, between the belly button and the groin. While acute pain appears suddenly and goes away quickly, chronic pain usually lasts for six months or more. These pains may be a sign of various issues affecting the reproductive, urinary, digestive, or musculoskeletal systems.
What makes your pelvis hurt?

There are various causes of pelvic pain, which differ between men and women.
Common causes in women
In women, pain in the pelvic area is often linked to the reproductive system. For example:
Menstrual cramps:
Cramps during your period are one of the most common causes of pelvic pain.
Mittelschmerz:
The pain happens when your ovary releases an egg.
Endometriosis:
Tissue that is similar to the inner lining of the womb grows outside of it.
Ovarian cysts:
An ovarian cyst is a fluid-filled sacthat grows in or on the ovaries and is not cancerous.
Uterine fibroids:
A fibroid is a non-cancerous growth that develops in or around your womb.
Pelvic inflammatory disease (PID):
A PID is an infection of your reproductive organs.
Hormonal and structural changes during pregnancy can put pressure on the pelvic muscles and joints, which causes discomfort. However, some pregnancy complications can cause pelvic pain and require emergency care, including:
Ectopic pregnancy:
Ectopic pregnancy happens when a fertilised egg grows outside the womb.
Miscarriage:
Miscarriage is the loss of a pregnancy before 20 weeks.
Placental abruption:
The organ that brings oxygen and nutrients to the baby breaks away from the inside wall of your womb.
Preterm labour:
It means that your body gets ready to give birth too soon.
Stillbirth:
The loss of a pregnancy after 20 weeks.
Common causes in men
Although pelvic pain is discussed less often in men, this condition shouldn’t be overlooked. Some common causes in males include:
Prostatitis:
Inflammation of the prostate gland can cause pain in the pelvic area, testicles, or lower back.
Epididymitis:
The epididymis is the coiled tube at the back of the testicle that stores and carries sperm.
The inflammation of the epididymis can lead to pelvic discomfort.
Benign prostatic hyperplasia:
The prostate is a small gland below the bladder that helps make semen, and it often gets bigger as you get older.
An enlarged prostate can block the flow of urine out of your bladder and cause pain in the pelvis.
Other causes
Common causes of pelvic pain in both men and women include:
Urinary tract infections (UTIs):
When bacteria infect the bladder or urethra, they can lead to UTIs, which cause burning, frequent urination, and pelvic discomfort.
Sexually transmitted infections (STIs):
Chlamydia and gonorrhoea are two common STIs that can cause pelvic pain.
Kidney stones:
These hard deposits can get into the urinary tract and cause severe, wavelike pain that spreads to your back or groin.
Digestive issues:
Irritable bowel syndrome (IBS), constipation, or bowel inflammation can make your pelvic area cramp and swell.
Musculoskeletal issues:
Muscle strain, pelvic floor tension, or hernias can trigger ongoing pelvic discomfort.
Nerve pain:
Pudendal neuralgia is nerve pain in the genitals, buttocks, anus or pelvis, which may cause sharp or shooting pelvic pain, especially when sitting.
Chronic pelvic pain:
The pain lasts for six months or longer and can be caused by a combination of physical, psychological, and social factors.
Symptoms of pelvic pain
The symptoms of pelvic pain vary depending on the underlying condition or disease that’s causing it. You may experience some common symptoms, such as:
A dull ache or heaviness in the lower abdomen
A sharp, stabbing pain or cramping that comes and goes
Worsening pain during daily activities like sitting, standing for a long time, or exercising
Pain during sexual intercourse, urination, or bowel movements
Irregular periods or abnormal vaginal discharge in women
Unusual penile discharge in men
Nausea, bloating, or fatigue along with pain in the pelvic area
Fever and chills in more severe cases
When to see doctor
Not all pelvic pain needs immediate medical attention, but there are warning signs that you should not ignore. If you notice any of the following symptoms, see your doctor right away:
Severe or sudden pelvic or abdominal pain
Pain that comes with fever, vomiting, or chills
Blood in stool, urine, or unexpected vaginal bleeding
Ongoing or worsening pain that lasts more than a few days
Pain during pregnancy
Pain after a recent pelvic injury or surgery
At Thomson Medical, our specialists can help to assess your symptoms and recommend appropriate tests to identify the cause of your pelvic pain. They can also provide a personalised treatment plan to help you feel comfortable again. Request an appointment today.
Our specialists
Loading...
How is pelvic pain diagnosed?
To diagnose pelvic pain, your doctor may take a step-by-step approach to find out what’s causing your symptoms.
Medical history
Your doctor may ask about your symptoms, menstrual cycle, prior infections, sexual activity, surgeries, or chronic illnesses.This helps guide whether the pain is related to the reproductive, urinary, digestive, or musculoskeletal systems.
Physical and pelvic examination
After taking a medical history, your doctor will perform a physical and pelvic examination. During this exam, they may gently press on your belly or pelvis to identify where the pain is coming from.
Laboratory and imaging tests
To find out what’s really causing your pelvic pain, your doctor might suggest a few laboratory and imaging tests. Here are some of the tests you may be done:
Blood or urine tests to check for infection
Swabs from the vagina, or cervix to detect STIs
Ultrasound to look at the uterus, ovaries, and other pelvic organs
CT scans or MRIs to get better view of deeper tissues
Laparoscopy to look inside the pelvis for hidden issues like endometriosis
Treatment for pelvic pain
Your doctor will recommend a treatment plan based on your diagnosis and the cause of your pain. Here are some of the treatments you may be given:
Antibiotics are often given for infections like UTIs or pelvic inflammatory disease
Hormonal therapies may help manage endometriosis or menstrual pain
Pain relievers and pelvic floor physical therapy for musculoskeletal causes
Nerve blocks to help with chronic pelvic pain
Dietary changes and medication can help with digestive issues like IBS
You might need surgery if you have fibroids, ovarian cysts, or severe endometriosis
Home remedies
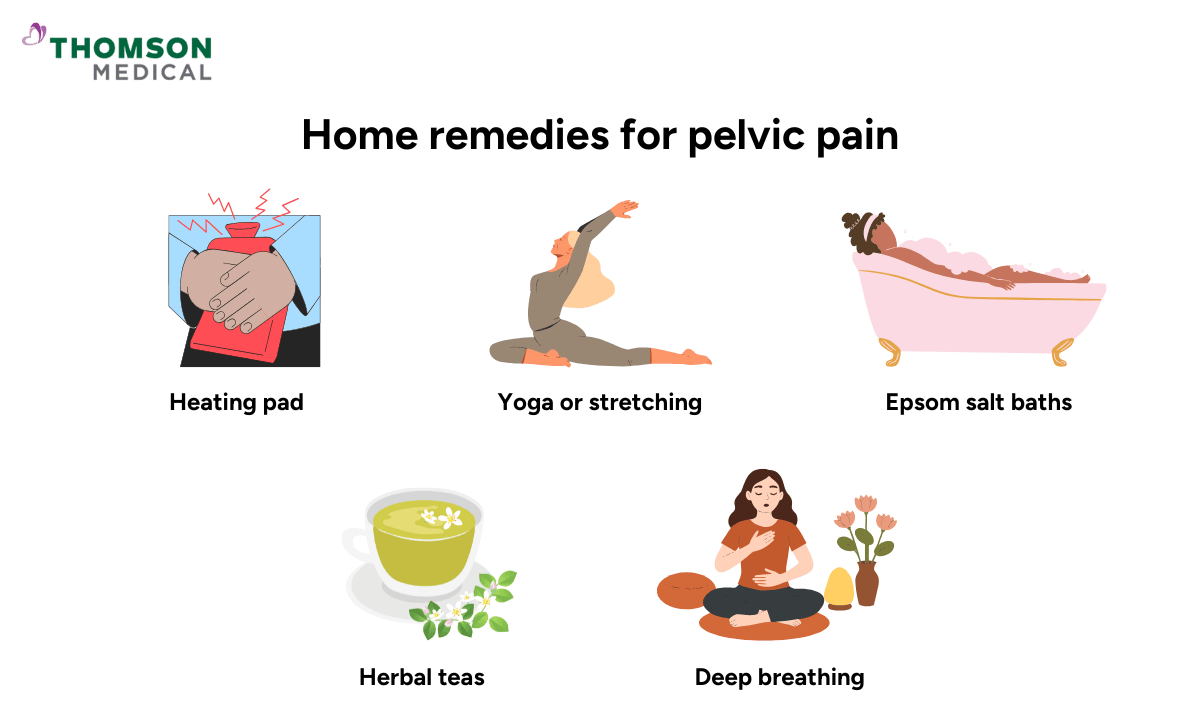
Along with medical treatments, you can try some home remedies to ease discomfort:
Applying a warm compress or heating pad to relax pelvic muscles
Doing yoga or gentle stretching to relieve tension
Taking Epsom salt baths to relax your muscles
Drinking herbal teas like chamomile or ginger to ease cramps
Practising stress-reduction techniques such as deep breathing or mindfulness
Always check with your doctor before starting any new remedy, even natural ones.
Can pelvic pain be prevented?
You can avoid some causes of pelvic pain, but not all of them. Here are some tips to help lower your risk:
Use condoms during intercourse to reduce the risk of STIs
Limit the number of sexual partners and have regular STI screenings
Avoid vaginal washing, as this can kill the beneficial bacteria
Get full treatment for STIs, UTIs, and other infections
Have regular gynaecological or urological check-ups
Strengthen your pelvic floor muscles, drink plenty of water, and eat a balanced diet to help your pelvic health
Worried about treatment plans, home remedies, or how to prevent pelvic pain? Thomson Medical is here to help.Request an appointment today to receive personalised advice.
FAQ
What does pelvic pain mean?
Infections (like UTIs and PID), reproductive issues (like ovarian cysts or endometriosis), gastrointestinal issues (like IBS), urinary problems, or even issues with the muscles and nerves can all cause pelvic pain.
What does pelvic pain feel like?
Pelvic pain can feel like a dull ache, a sharp stabbing pain, or a feeling of pressure in your lower belly. It could come and go or stay and might get worse when you move, urinate, or have sexual intercourse.
What is considered severe pelvic pain?
Severe pelvic pain is sudden, intense, and disrupts your daily activities. It could also come with a fever, nausea, fainting, or bleeding.
Can UTIs cause pelvic pain?
Yes. UTIs often cause discomfort in your lower abdomen, along with burning during urination and frequent urges to urinate.
What kind of infection causes pelvic pain?
Common infections include UTIs, PID, STIs, prostatitis in men, and yeast or bacterial vaginal infections in women.
Does pelvic pain heal on its own?
Some causes of pelvic pain are mild and may heal on their own, like menstrual cramps or ovulation pain. However, pain in the pelvis can also be a symptom of underlying issues that need medical treatment, such as an infection or an ectopic pregnancy.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical.Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
