Choosing intrauterine insemination (IUI) is a significant step in your fertility journey, and knowing the factors that influence its success can help you decide if it’s right for you. Whether you have ovulation issues, mild male infertility, or unexplained challenges, this article explains who benefits most from IUI and what the process involves.
What is intrauterine insemination (IUI)?
IUI is a type of assisted reproductive technology (ART). In this treatment, sperm is gently placed directly into the uterus around the time you ovulate. This increases the number of motile sperm that reach your fallopian tubes, which improves your chances of fertilisation.
Because it is less invasive and more affordable than in vitro fertilisation (IVF), IUI is often one of the first treatment options doctors suggest for certain types of infertility.
Who is a good candidate for IUI?
IUI can be a helpful option for many people, but before considering it, your doctor will check a couple of basics. At least one of your fallopian tubes should be open, and your uterus should have a healthy lining to support pregnancy.
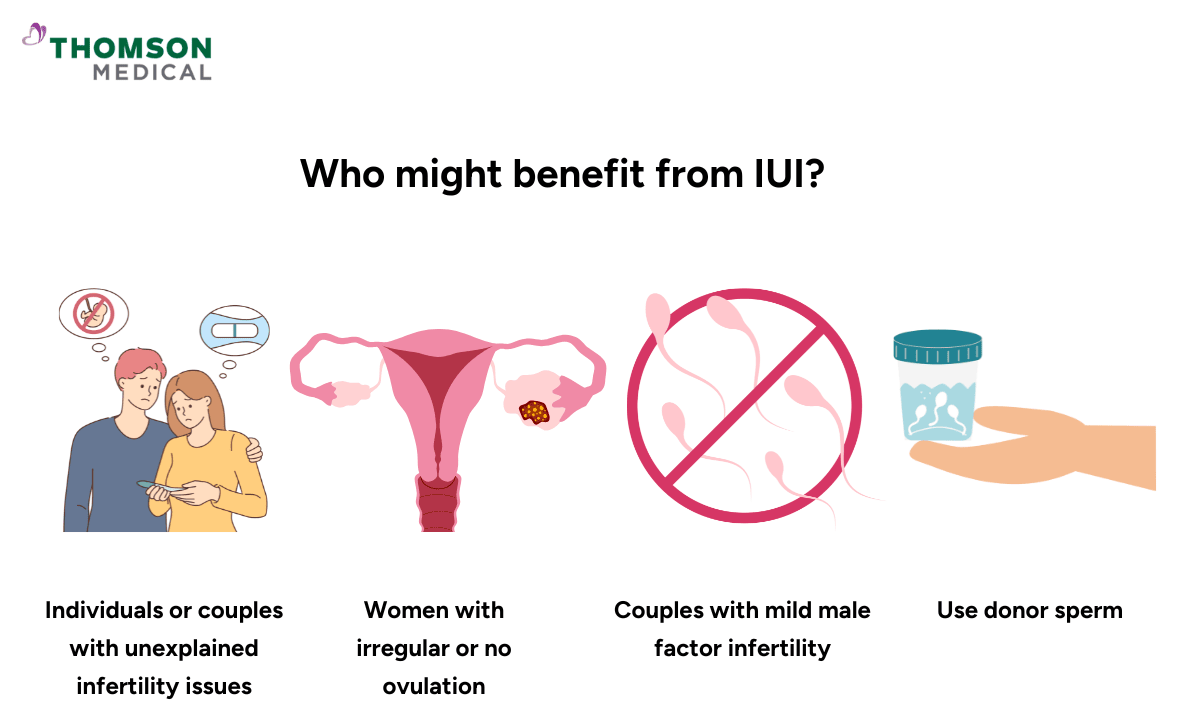
Your fertility specialist might suggest IUI if:
Unexplained infertility, which means you’ve been trying for 6–12 months with normal test results but no pregnancy
There’s a mild male factor, like slightly low sperm count or reduced motility
You have irregular or absent ovulation, such as with polycystic ovary syndrome (PCOS)
Your cervical mucus makes it hard for sperm to pass through
You or your partner experience sexual difficulties that make intercourse challenging.
You’re using donor sperm — for example, if you’re a single woman or in a same-sex female couple
You have mild endometriosis and are also using ovulation induction
If you're in one of these situations, IUI may not be your only option, but it could be a gentle next step to discuss with your doctor.
Fertility issues that intrauterine insemination (IUI) cannot address
While IUI can be a beneficial choice for certain fertility issues, it is not the right option for every situation. In particular, it may not be suitable for cases such as blocked fallopian tubes or severe male factor infertility. Your doctor may recommend exploring other treatments in the following situations:
Blocked or damaged fallopian tubes:
If both fallopian tubes are blocked or scarred, IUI cannot help since sperm and egg cannot meet.
Severe male factor infertility:
Very low sperm count, poor motility, or abnormal morphology often require IVF with ICSI (intracytoplasmic sperm injection).
Advanced endometriosis:
More severe forms of endometriosis may require IVF for better success rates.
Low ovarian reserve:
If a woman has diminished ovarian reserve or a poor response to fertility medications, IVF may be more effective.
Genetic concerns:
If there’s a need for preimplantation genetic testing, IVF is the appropriate treatment.
For more personalised information about whether IUI is the right fertility treatment for you, and to discuss your unique situation, consider consulting a fertility specialist. You can contact Thomson Medical to arrange a consultation and receive expert guidance tailored to your fertility needs and treatment options.
Our fertility specialists
Loading...
Factors that influence candidacy

Several factors determine if IUI is a good fit and its potential success. Your doctor will usually look at:
Age:
Women under 35 tend to see higher success rates with IUI. Fertility naturally declines over time, especially after the age of 40, but every person's journey is unique.
Ovarian reserve:
This value measures the number of eggs that may still be present in your ovaries. It is checked through Anti-Müllerian Hormone (AMH) and Follicle Stimulating Hormone (FSH) blood tests, as well as an ultrasound count of tiny resting follicles. A healthy reserve can improve your chances.
Sperm quality:
After the sperm is "washed" and prepared, ideally there should be more than 5-10 million moving (motile) sperm for the best odds.
Tubal patency:
At least one open and functioning fallopian tube is needed so that sperm and egg can meet naturally.
Uterine health:
A healthy uterine cavity and a thick, receptive lining make it easier for an embryo to implant.
Lifestyle factors:
Habits like smoking, unmanaged health conditions, or carrying excess weight can sometimes lower success rates, while a balanced lifestyle may help.
Remember, these aren’t “pass or fail” rules. Many people still conceive despite challenges in one or more of these areas. Your fertility team will look at the whole picture to guide you toward the best options for you.
How does the IUI process work?
If you’re considering IUI, here’s what the process usually looks like, step by step:
Tracking or stimulating ovulation:
Your fertility team will monitor your natural cycle using ultrasounds and blood tests. Alternatively, they may give you medications (like clomiphene, gonadotropins, or letrozole for IUI) to help your ovaries release one or more eggs.
The trigger shot (if needed):
In cases where natural ovulation timing is uncertain, a hormone injection—often hCG—is given to prompt ovulation at just the right time.
Sperm collection and preparation:
A sperm sample is provided by your partner or a donor. In the lab, it’s “washed” to remove fluids and concentrate the healthiest, most active sperm.
The insemination itself:
The prepared sperm is gently placed into your uterus using a thin, flexible catheter. It’s usually quick (just a few minutes) and either painless or only mildly uncomfortable.
After the procedure:
Your doctor may prescribe progesterone to help support your uterine lining, which is important for maintaining a potential pregnancy. Following this, there is a waiting period of about two weeks before you can take a pregnancy test to see if the cycle was successful.
Alternatives to IUI: When to consider IVF
Many people try IUI for a few cycles before considering more advanced fertility treatments. The number of IUI cycles needed for pregnancy typically ranges from 3 to 6 attempts, after which your doctor may suggest IVF as the next step due to its higher success rates.
IVF could be worth considering if:
You’re over 35 and haven’t conceived after several IUI attempts
There’s severe male factor infertility, such as very low sperm count or poor sperm quality
Both fallopian tubes are blocked
You require preimplantation genetic testing (PGT) because of a known genetic condition
You’ve experienced recurrent pregnancy loss
You’re a same-sex couple or single parent wanting to boost success rates with donor eggs or sperm
If you have one of these situations, your journey does not end here. Your care team may guide you toward a treatment that has a higher chance of success based on your unique circumstances.
FAQ
Is IUI painful?
Most people find IUI isn’t painful. The procedure is similar to a Pap smear, where a thin, flexible catheter is gently inserted through the cervix to place washed sperm directly into your uterus.
You might feel some mild cramping or pressure during insertion and possibly light spotting or discomfort afterward. The whole process usually takes just a few minutes, no anaesthesia is needed, and most people can go back to their normal activities right away.
How many IUI cycles should I try?
Most fertility specialists say to try 3 to 4 IUI cycles before thinking about other treatments like IVF. This is based on cumulative pregnancy rates, where success tends to build over multiple cycles.
Younger patients or those with unexplained infertility often benefit from more cycles. If you don’t conceive after 3–4 cycles, your doctor may re-evaluate your fertility plan based on your age, test results, and overall response to treatment.
Does IUI work for everyone?
IUI is not effective for every type of infertility. It works best for mild male infertility, irregular ovulation, unexplained infertility, donor sperm insemination or mild endometriosis.
IUI may not work for people with blocked or damaged fallopian tubes. It may also fail for those with severe sperm problems, very low ovarian reserve, or moderate to severe endometriosis.
Can I do IUI if I have irregular periods?
Yes! You can do IUI even if your periods are irregular. However, ovulation usually needs to be induced or closely monitored. Your doctor might prescribe medications such as Clomid or letrozole to stimulate ovulation for conditions like PCOS or anovulation.
Ultrasound monitoring and possibly a trigger shot help time the IUI perfectly, which improves your chances, even if your cycle isn’t predictable.
What’s the best age to do an IUI?
The best age for IUI is generally under 35, when fertility and egg quality tend to be higher. Success rates for women under 35 are usually around 10–20% per cycle. These rates gradually decrease after 35 and more sharply after 40. Women over 40 can still try IUI. Doctors often suggest fewer attempts before considering IVF, especially when timing matters.
Can IUI be used after a failed IVF cycle?
Sometimes, IUI might be an option after IVF hasn’t worked, depending on the reason for the IVF failure and your current fertility health. You might consider IUI if:
The IVF failure was due to technical issues, like trouble with embryo transfer
Your ovarian reserve is good and your fallopian tubes are healthy
You want to try a less invasive approach before another round of IVF
However, if IVF fails because of poor egg quality or fertilisation problems, your doctor may recommend different treatments to increase your chances.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
For more information, contact us:
Thomson Fertility
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Request an Appointment