As you get older, it is natural to wonder whether cervical cancer screening is still necessary. Many women feel that the danger may have passed, especially if they have been in a long-term relationship or are no longer sexually active.
However, cervical cell changes can take a long time to develop, and age alone does not remove the risk. Learning how cervical cancer can affect women later in life, and when screening is still recommended, can help you make informed and confident decisions about your health.
Can older women get cervical cancer?
Yes, cervical cancer can affect women over 50, and understanding why can help you stay proactive about your health during and after menopause. Whilst screening programmes have led to an overall decrease in cervical cancer rates, it remains important to stay vigilant, particularly if you haven't had regular screenings.
The current guidelines in Singapore recommend cervical screening for women up to at least age 65, even if you've had a history of normal results.
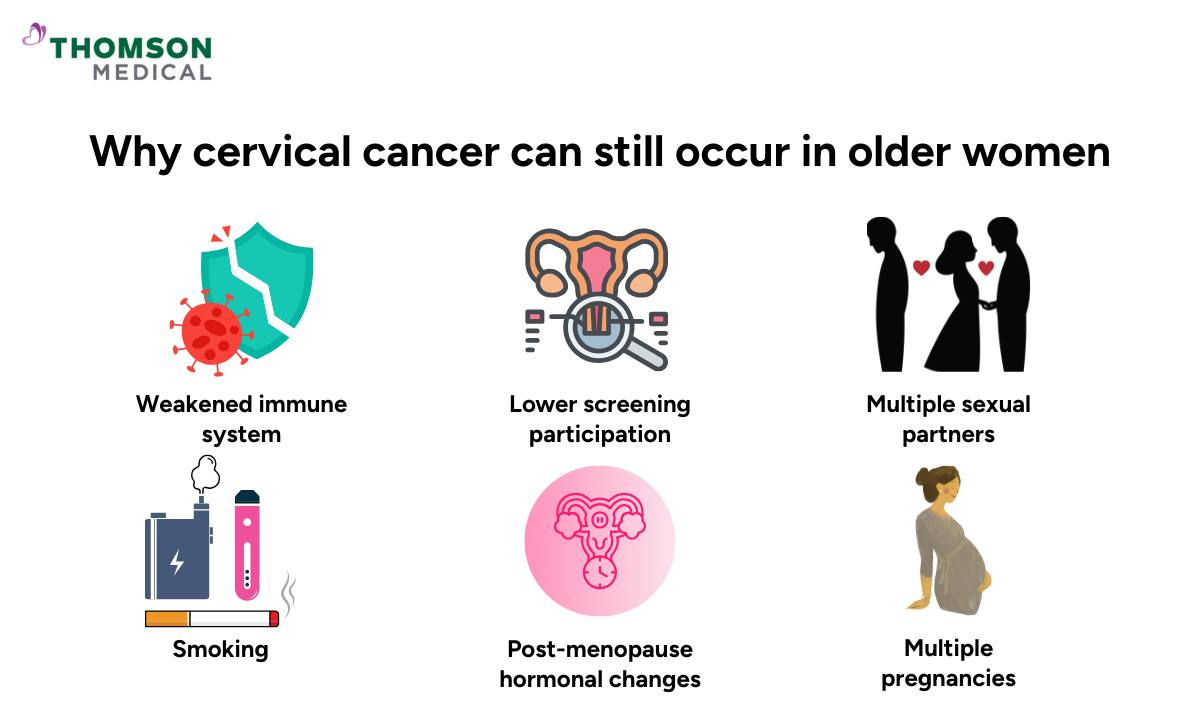
Why cervical cancer can still occur in older women
While cervical cancer is very rare in women under 20, the likelihood of developing it tends to increase gradually as you move through different life stages.
Most cases are diagnosed in women between 35 and 44 years of age, with the average age at diagnosis being around 50. However, risk doesn't simply disappear after these peak years. Even if you've had regular cervical cancer screenings in the past, it's worth discussing your individual risk with your doctor as you age.
Nearly all cervical cancers develop from high-risk types of human papillomavirus (HPV) that persist in the body. You may have been exposed many years ago. Whilst most women naturally clear HPV within two years, persistent infections can gradually cause cell changes over 10 to 20 years, eventually developing into cancer.
Several factors can increase the likelihood of cervical cancer as you age:
Weakened immune system
Your immune system naturally becomes less robust with age (immunosenescence)
This makes it harder to fight off existing HPV infections
Your body may be less able to prevent abnormal and cancerous cells from progressing
Lower screening participation
Some women may not realise screening remains important through their 50s and 60s
In Singapore, screening is recommended until age 69
If you weren't screened regularly earlier or have missed recent screenings, any pre-cancerous changes may go undetected
Other contributing factors
Having had multiple sexual partners (higher HPV exposure)
Multiple pregnancies
Smoking (past or present)
Being overweight
Post-menopausal hormonal changes
Seeing yourself amongst these risk factors can feel concerning, but it doesn't mean you're guaranteed to develop cervical cancer. They're simply a gentle reminder of why screening is such a powerful tool in looking after your health.
Signs of cervical cancer in older women
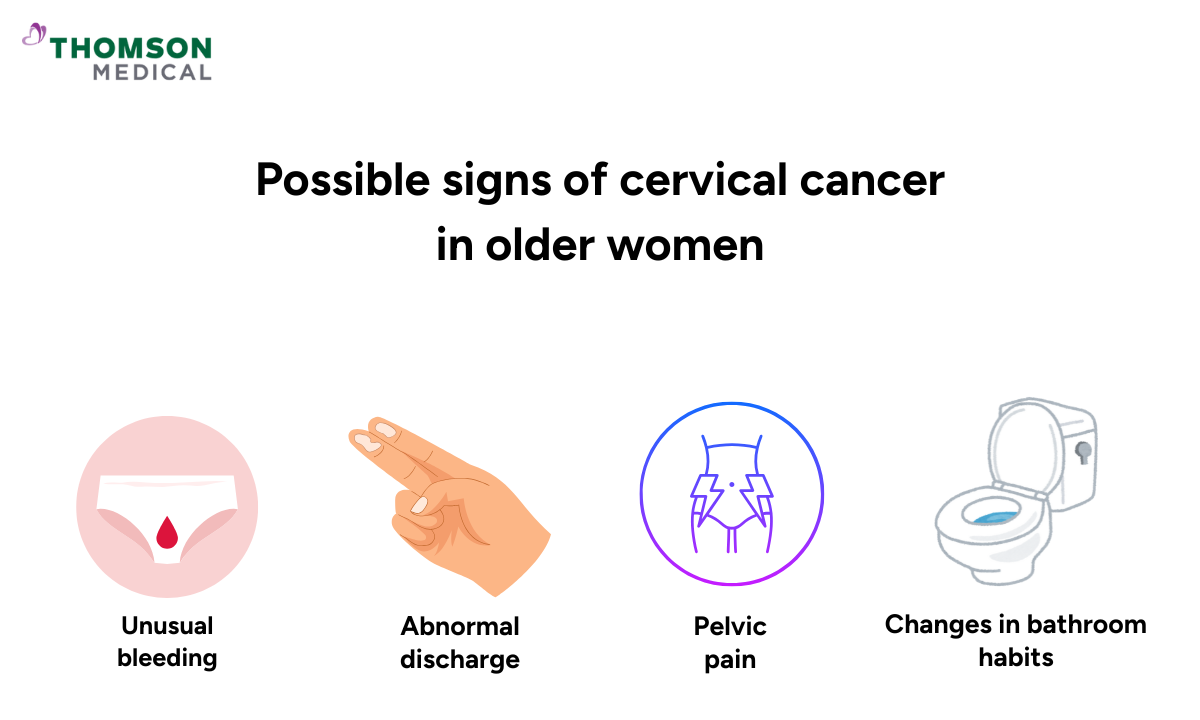
Whilst early-stage cervical cancer often has no symptoms, it's important to know what changes you should look out for. The main signs of cervical cancer in older women include:
Unusual bleeding:
Vaginal bleeding after menopause, after intercourse, or between periods
Abnormal discharge:
Unusual discharge, particularly if watery, blood-tinged, or with an unpleasant odour
Pelvic pain:
Pain during intercourse, persistent lower back pain, or unexplained leg pain
Changes in bathroom habits:
Altered bowel or bladder habits, or discomfort during urination
Noticing these symptoms can be unsettling, but try not to jump to conclusions yet. Most of the time, they're linked to conditions that are much easier to manage than cervical cancer. Still, if you're experiencing unusual bleeding after menopause, it's important to reach out to your doctor promptly, because getting answers will bring clarity and help you move forward with confidence.
If you'd like to discuss your cervical health or have concerns about any symptoms, you can request an appointment with Thomson Medical. Our women's health specialists are here to support you with personalised care.
How screening matters for older women
In Singapore, cervical cancer screening is recommended until age 69. Here's what you need to know:
Cervical cancer can occur at any age:
More than 20% of cervical cancer cases are diagnosed in women over 65
HPV risk doesn't disappear:
High-risk HPV infections can persist or be newly acquired, even in older women
Early detection saves lives:
Screening can detect abnormal cells before they become cancerous, giving you the best chance for successful treatment
Therefore, it is recommended that you follow the cervical screening guidelines in Singapore:
Continue screening until age 69:
This is the general recommendation for women who have been sexually active
Don't stop without medical advice:
Always discuss your individual screening plan with your doctor before stopping
Your screening history matters:
You may be able to stop screening at 69 if you've had consecutive negative results over the past 10 years, but this should be confirmed by your doctor
Following these screening guidelines gives you strong protection, and knowing when to contact your doctor between screenings completes that circle of care.
When to seek medical advice
Knowing when to reach out for medical advice helps you take charge of your cervical health. Here are situations where a conversation with your doctor is particularly important:
A history of abnormal cervical cells or pre-cancerous changes
A previous diagnosis of cervical cancer
A weakened immune system (from conditions like HIV/AIDS or medications such as steroids or immunosuppressants)
A history of diethylstilbestrol (DES) exposure before birth
Together with your doctor, you can map out a screening journey that honours where you are in life and your personal health background. The challenge with early cervical changes is their silence; you won't feel them developing, which is exactly why screening matters so much. If something does catch your attention between appointments, pay attention to that inner voice and seek medical advice as soon as you can.
Our cervical cancer specialists
Loading...
Whether you're due for routine screening or experiencing symptoms that concern you, our women’s health specialists at Thomson Medical can help. Schedule an appointment with us to discuss your cervical health with a specialist who understands your needs.
FAQ
Is cervical cancer common in older women?
Cervical cancer is less common in older women compared to younger age groups, with the highest rates occurring between ages 35 and 44.
The risk persists because cervical cancer develops slowly, often over 10 to 20 years from persistent HPV infection. This is why regular screening remains important as you age. In Singapore, screening is recommended until age 69 to help detect any changes early, when they're most treatable.
What are the five warning signs of cervical cancer?
The main warning signs to be aware of include:
Abnormal vaginal bleeding
Pain during intercourse
Pelvic pain
Changes in vaginal discharge
Discomfort when urinating
If any of these sound familiar, try not to worry, because they're usually caused by other, less serious conditions. Still, it's always worth having a conversation with your doctor to understand what's going on and get the support you need.
How does the risk of cervical cancer change after menopause?
Your risk of cervical cancer doesn't disappear after menopause. In fact, it can persist or even increase with age, particularly if you haven't had regular screening throughout your life. High-risk HPV infections can still occur in post-menopausal women, with some studies showing infection rates may increase after age 65.
Can HPV cause cervical cancer later in life?
Yes, a persistent infection with high-risk HPV can lead to cervical cancer later in life, even many years after initial exposure. HPV can cause pre-cancerous changes in cervical cells that develop very slowly over time, sometimes 10 to 20 years. This is why you might have been exposed to HPV decades ago, and those cell changes are only now becoming a concern.
How often should you get cervical screening after 50?
In Singapore, screening recommendations after age 50 depend on your age and screening history:
Ages 50-69: Continue with HPV testing every 5 years (if you're 30 or over, HPV testing is the recommended screening method)
After age 69: You may be able to stop screening if you've had consecutive negative results over the past 10 years, but this should be discussed with your doctor
It's always best to discuss your specific screening needs with your healthcare provider, who can create a personalised plan that's right for you.
Are cervical screenings necessary if I'm not sexually active?
Yes, cervical screening is still recommended even if you're not currently sexually active. Here's why:
You may have been exposed to HPV in the past, which can remain dormant for years
Singapore guidelines recommend screening for all women aged 25-69, regardless of sexual activity
HPV can be transmitted through close genital contact, not just intercourse
If you've never been sexually active, your risk is very low, but it's still worth discussing your individual situation with your doctor.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment