Cervical cancer is the 10th most common cancer among women in Singapore, yet it's highly preventable. Regular screening and HPV vaccination stop most cases before they develop. Here's what you need to know about risk factors, symptoms, and prevention.
What is cervical cancer?
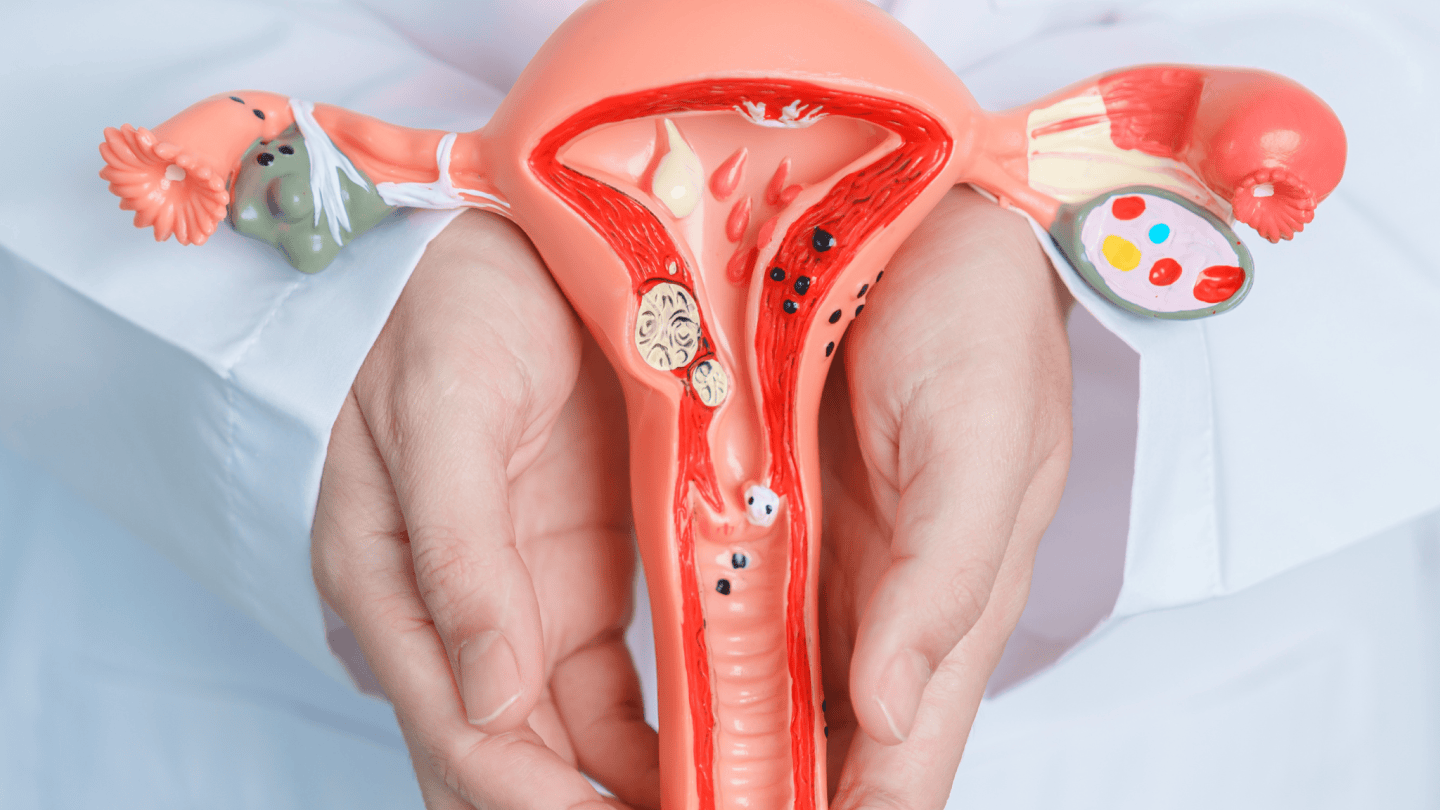
Cervical cancer develops in the cells of the cervix, the lower part of the uterus connecting to the vagina. It starts with abnormal changes in cervical cells, known as precancerous changes or dysplasia, which can develop into cancerous tumours over time. This type of cancer progresses slowly, providing opportunities for early detection and intervention.
Prevalence of cervical cancer in Singapore
Despite an advanced healthcare system, cervical cancer remains a significant health issue in Singapore. According to the Singapore Cancer Registry, it is one of the top ten cancers affecting women in the country.
What causes cervical cancer?
Human papillomavirus (HPV) causes nearly all cervical cancers. Specifically, persistent infection with high-risk HPV types—particularly HPV 16 and 18—is responsible for approximately 70% of cervical cancer cases worldwide.
How does HPV leads to cervical cancer?
HPV is extremely common. Most sexually active people get HPV at some point, but their immune systems clear the virus naturally within 1-2 years without causing problems.
Cervical cancer develops when:
- High-risk HPV persists in your body instead of clearing
- The virus causes abnormal cell changes in your cervix over time
- These abnormal cells progress from precancerous lesions to invasive cancer
- This process typically takes 10-20 years, which is why screening catches changes early
Not everyone with HPV develops cervical cancer. Your immune system usually eliminates the virus before it causes serious damage.
Who is at risk of cervical cancer?
While HPV is the primary cause, certain factors increase your risk of persistent infection and cancer development:
- Smoking:
- Tobacco use increases the risk of cervical cancer and can worsen the effects of HPV infection.
- Weak immune system:
- Conditions or medications that weaken the immune system can increase susceptibility to HPV infection and cervical cancer.
- Multiple sexual partners:
- Engaging in sexual activity with multiple partners or having a partner who has multiple sexual partners increases the risk of HPV infection.
- Early sexual activity:
- Initiating sexual activity at an early age is associated with a higher risk of HPV infection and cervical cancer.
What are the symptoms of cervical cancer?

Cervical cancer may not cause noticeable symptoms in its early stages, making regular screening crucial. As the cancer progresses, symptoms may include:
- Abnormal bleeding:
- You might experience bleeding between periods, after sex, or after menopause. Your periods may become heavier or last longer than usual.
- Pelvic pain or discomfort:
- You may experience persistent pelvic pain that is unrelated to your menstruation or other known causes.
- You may experience pain during sexual intercourse (dyspareunia)
- Unusual vaginal discharge:
- Increased vaginal discharge that may be watery foul-smelling
- Cervical cancer discharge may contain blood or occur outside of menstrual periods
- Pain or bleeding during urination:
- Painful urination (dysuria) or blood in your urine (haematuria) can occur when cancer affects nearby tissues.
- Other symptoms:
- As cervical cancer spreads, you may develop lower back or abdominal pain, unexplained fatigue, unintentional weight loss, or swelling in one or both legs.
Doctors who can help diagnose cervical cancer
Loading...
How is cervical cancer diagnosed?
- Colposcopy:
- If abnormalities are detected during screening, a colposcopy examines the cervix in greater detail, and areas of abnormality can be biopsied.
- Biopsy:
- A small tissue sample is removed from the cervix for examination under a microscope to confirm the diagnosis and provide information about the type and stage of the cancer.
- There are different types of biopsies which may be performed depending on the location and extent of the abnormality. A biopsy allows for the definitive diagnosis of cervical cancer.
- Imaging tests:
- Ultrasound, CT scan, or MRI may be used to assess the extent of the cancer and guide treatment decisions.
Treatment of cervical cancer
Treatment for cervical cancer depends on the stage of the cancer, overall health, and patient preferences. Options include:
- Surgery:
- Surgical procedures such as hysterectomy (removal of the uterus) or trachelectomy (removal of the cervix) may be recommended for early-stage cervical cancer.
- Radiation therapy:
- High-energy beams are used to destroy cancer cells, often combined with surgery for locally advanced cancer.
- Chemotherapy:
- Drugs are used to kill cancer cells, either with radiation (chemoradiation) or as palliative treatment for advanced cancer.
- Targeted therapy and immunotherapy:
- These treatments target specific molecular pathways and harness the immune system to fight cancer cells.
In addition to these treatment modalities, supportive care such as pain management, nutritional support, and psychological support plays a crucial role in improving the quality of life for women with cervical cancer.
How can cervical cancer be prevented?
There are several ways to prevent cervical cancer. Some of them are listed below.:
- HPV vaccination:
- Vaccination against HPV is highly effective in preventing cervical cancer. It is recommended for adolescents before sexual activity but can also benefit those who have been sexually active.
- Regular cervical cancer screening:
- Pap smears and HPV DNA tests detect abnormal cells or HPV infection early, allowing for timely intervention.
- Safe sex practices:
- Consistent condom use and limiting the number of sexual partners reduce the risk of HPV infection.
- Smoking cessation:
- Quitting smoking reduces the risk of developing cervical cancer.
- Healthy lifestyle choices:
- A balanced diet, regular physical activity, and avoiding excessive alcohol consumption support a strong immune system.
- Screening and treatment of precancerous lesions:
- Prompt treatment of precancerous changes can prevent progression to invasive cancer.
- Procedures such as cryotherapy, loop electrosurgical excision procedure (LEEP), or cone biopsy may be used to remove abnormal cervical tissue.
Treatment at Thomson Medical
At Thomson Women's Clinic & Cancer Surgery, our women's cancer specialists understand that a cancer diagnosis can feel overwhelming. We specialise in comprehensive gynaecological cancer management, combining advanced treatment options with personalised, compassionate care.
What to expect during your care:
- Thorough consultation to discuss your diagnosis and treatment options
- Detailed explanation of recommended treatments and expected outcomes
- Access to advanced treatment technologies and minimally invasive surgical techniques
- Clear information about managing side effects and recovery
- Coordination with oncologists, radiologists, and other specialists as needed
- Ongoing support during and after treatment, with regular monitoring
Prevention is equally important: We also offer a comprehensive 4-in-1 women's screening package that includes consultation, Pap smear, HPV test, and pelvic ultrasound—helping detect abnormalities early when treatment is most effective.
Cervical Cancer Treatment Cost in Singapore
The cost of cervical cancer treatment in Singapore varies significantly depending on the stage of cancer, type of treatment required, and whether you choose public or private healthcare facilities.
Some of the procedures to help treat cervical and ovarian cancer includes:
- Laparoscopic surgery:
- Laparoscopic surgery costs are performed as day surgeries and range from SGD 7,200 to SGD 11,570, depending on whether you choose public or private hospitals.
- Colposcopy:
- The cost of a colposcopy can vary depending on whether it is performed as day surgery or inpatient surgery, which can cost from SGD 1,200 to SGD 10,400.
Additional costs to consider
Beyond the primary treatment costs, you should budget for:
- Pre-treatment consultations and specialist visits
- Diagnostic tests including Pap smears, HPV tests, colposcopy, and biopsies
- Imaging studies such as CT scans, MRI scans, or PET scans
- Laboratory tests and blood work
- Medications for managing side effects
- Post-treatment follow-up appointments and surveillance scans
- Rehabilitation or supportive care services
How does insurance work for cervical cancer treatment?
Understanding insurance coverage for cervical cancer treatment can be complex, as different components may be covered differently:
- Doctor's fees:
- Each specialist has their own panel of insurance providers and coverage arrangements
- Procedures and scans:
- Some procedures like diagnostic imaging or certain surgical techniques may be subsidised by the Singapore government or covered under MediShield Life
- Overall treatment costs:
- Your total out-of-pocket expenses will depend on how your insurance plan covers both the doctor's professional fees and the hospital/procedure costs
Fortunately, there are several programmes in Singapore that can help lower the total cost, such as MediSave, MediShield Life, and Integrated Shield Plans. Each of these offers different levels of coverage depending on your eligibility and insurance arrangements.
This price was last updated in June 2025. Treatment costs may have changed since then. For current pricing, detailed insurance coverage information, and personalised financial guidance, contact our medical concierge team.
FAQ
What are the screening tests for cervical cancer?
Screening aims to detect precancerous changes or early-stage cancer for timely intervention. The main screening tests include:
- Pap smear (Pap test)
- HPV DNA test
This test detects high-risk HPV strains in cervical cells, identifying women at higher risk of developing cervical cancer due to persistent HPV infection. It is often used in conjunction with the Pap smear.
This test detects high-risk HPV strains in cervical cells, identifying women at higher risk of developing cervical cancer due to persistent HPV infection. It is often used in conjunction with the Pap smear.
Do I still need screening if I had the HPV vaccine?
Yes. The vaccine does not protect against all cancer-causing HPV types. Regular screening is still necessary for comprehensive prevention.
Is cervical cancer hereditary?
No. It is caused mainly by HPV infection, not genetic inheritance.
I have no symptoms. Do I still need screening?
Yes. Cervical cancer can be asymptomatic in early stages, and screening can detect abnormal changes before they turn cancerous.
Can men get cervical cancer or HPV?
No, men cannot get cervical cancer because it is a cancer that affects the cervix, an organ unique to the female reproductive system. However, men can be infected with HPV, which may cause other HPV-related cancers such as those of the penis, anus, mouth, or throat.
Can you get cervical cancer without HPV?
Almost all cases of cervical cancer are caused by high-risk HPV infection. However, some very rare types of cervical cancer can develop without HPV involvement. There is currently no suitable screening test for these rare forms of cervical cancer, and common tests like the Pap smear or HPV test are unable to detect them.
The information provided is for general guidance only and should not be considered as medical advice. For a personalised consultation and tailored advice, schedule an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment
