If you have ever wondered at what age cervical cancer is most likely to develop, you are certainly not alone. Many women have similar questions as they grow older and begin learning about the importance of health screening.
While cervical cancer can develop at any adult age, it is more often diagnosed in midlife. Learning how factors such as age, HPV exposure, and screening habits influence risk can help you feel more confident about taking timely steps towards cervical cancer screening and prevention.
Common age group for cervical cancer
In Singapore, cervical cancer is the 11th most common cancer among women overall and the 5th most common in women aged 15–44, meaning that it affects women across many different age groups.
Age-specific incidence rate
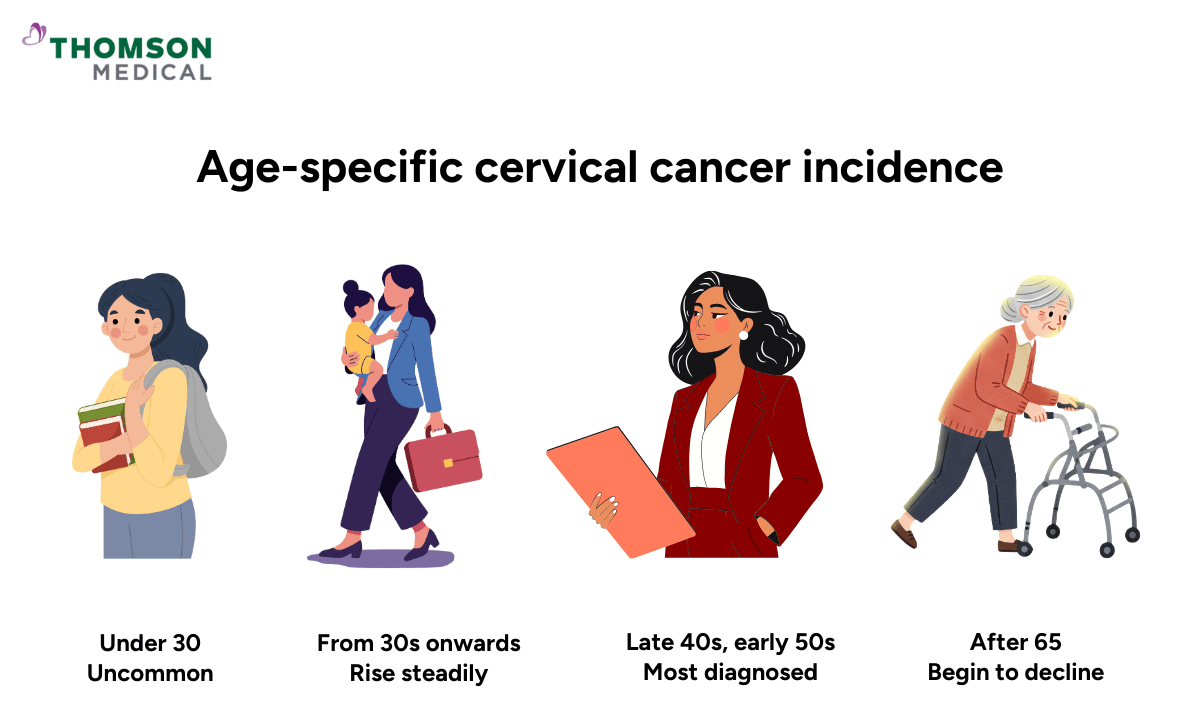
Cervical cancer does not affect all age groups equally. For women under 30, cervical cancer is uncommon.
However, from your 30s onwards, the numbers start to climb. Women in their late 40s and early 50s are diagnosed most often. This timing usually reflects human papillomavirus (HPV) infections from years or even decades earlier that progressed quietly without being detected.
After 65, your risk starts to drop. This happens largely because of regular Pap smears, better awareness about cervical health, and HPV vaccines – all of which help to catch and treat abnormal cells before they become cancerous.
Why is cervical cancer rare in young women?
Cervical cancer is uncommon in young women because it takes a long time – usually a decade or more – for HPV to develop into cancer.
HPV infection is common in younger women, especially in the first few years after they start having sex. But here's the good news: in most cases, your immune system clears the virus on its own within one to two years. When your body gets rid of the infection naturally, there isn't enough time for the cell changes that lead to cancer to develop.
Does the risk of cervical cancer decrease as you get older?
Your risk of cervical cancer usually drops after menopause, but it doesn't go away completely. If you've kept up with regular cervical cancer screenings and received the HPV vaccine, your risk later in life is much lower.
That said, older women who've never been screened, missed appointments, or have ongoing high-risk HPV infections can still develop cervical cancer. That's why it's still important to follow screening guidelines, even after you've gone through menopause.
If you are unsure about your own risk or screening history, consulting an O&G specialist can help clarify when and how often cervical screening is right for you. Schedule an appointment with Thomson Medical today.
Our cervical cancer specialist
Loading...
Prevention and early detection of cervical cancer
Knowing when cervical cancer usually happens is helpful, but what really protects your health is prevention. By catching problems early, you can reduce the risks and improve your chances of successful treatment.
HPV vaccination
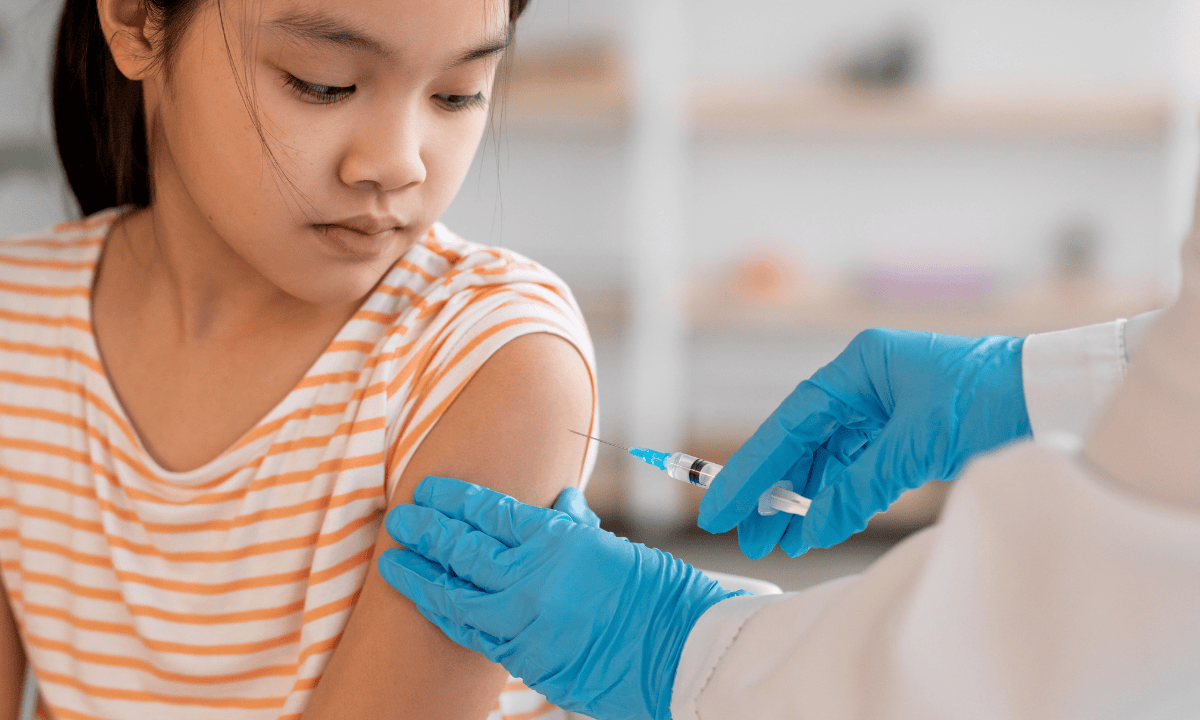
The HPV vaccine protects you against the high-risk virus types that cause most cervical cancers, especially HPV types 16 and 18 (which are behind the majority of cases worldwide).
In Singapore, HPV vaccination is strongly recommended. The national programme encourages girls from age 9 onwards to get vaccinated before they start having sexual activities, as this is when the protection is most effective.
But the vaccine isn't just for teenagers. If you're an adult woman who hasn't been vaccinated yet, you can still benefit, as the vaccine protects against some high-risk HPV strains you might not have encountered yet. Even if you're already sexually active, getting vaccinated can lower your risk going forward.
Regular screening
Regular cervical screening is still important, even if you've already been vaccinated. Pap smears and HPV tests can find abnormal or precancerous cells before any obvious symptoms appear, allowing you to get treated before they turn into cancer.
The Singaporean Ministry of Health recommends:
Women aged 25 to 29: Pap smear every three years
Women aged 30 and above: HPV DNA test every five years
Regular screening and timely vaccination remain the most effective ways to protect against cervical cancer. If you would like guidance on cervical screening or HPV vaccination, request an appointment with Thomson Medical today. Our O&G specialists are here to support you at every stage of life.
FAQ
When am I most at risk for cervical cancer?
The risk is highest in women in their 30s to 50s, when long-term high-risk HPV infections have had time to develop into cancer. HPV can occur at any age after sexual activity, but cancer usually takes years to form.
Can a 25-year-old get cervical cancer?
Yes, but it is very uncommon. Cervical cancer is rare under 30 because HPV-related cell changes usually take many years to become cancer.
At what age does HPV cause cancer?
HPV infection can occur at any age after becoming sexually active, but cancer develops only after persistent infection over many years. As a result, HPV-related cancers most often appear in women in their 30s, 40s, or later.
What age is too late for HPV vaccination?
The vaccine works best before HPV exposure, usually in early adolescence. Catch-up vaccination is commonly offered up to age 26. After this, some adults may still benefit, but effectiveness may be lower.
What age should cervical cancer screening start?
Screening usually begins at age 21 or 25, depending on guidelines. This timing balances early detection with the fact that younger women often clear HPV naturally.
Why is cervical screening stopped at 64?
Screening often stops around age 65 for women with consistently normal results, as their risk becomes very low. Those who have not been regularly screened or have risk factors may need continued follow-up.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
Reference:
Bruni L, Albero G, Serrano B, et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Singapore. Summary Report, 10 March 2023. https://hpvcentre.net/statistics/reports/SGP.pdf. Accessed 8 Jan 2026.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
