Finding out you have genital warts can be alarming, but it doesn’t mean anything is “wrong” with you. This is a common, manageable condition, and treatment is usually simple and effective. With the right care, you can get it under control, lower the risk of passing it on to your partners, and enable yourself to maintain healthy intimate relationships.
What are genital warts?

Genital warts are a common sexually transmitted infection (STI) caused by low-risk HPV types 6 and 11 of the human papillomavirus (HPV). They appear as small, flesh-coloured or whitish growths in your genital or anal area.
Sometimes they form clusters with a cauliflower-like texture. While they’re often painless and treatable, a proper diagnosis is important because HPV can also include strains that are linked to cervical and other cancers. Additionally, many people who have HPV don't develop visible warts straight away, so they may carry the virus unknowingly.
Recognising genital wart symptoms
Although HPV doesn’t always cause symptoms, when they do appear, they can vary from person to person. Here is what you might notice:
Small growths in the genital or anal area:
These may be flesh-coloured, white, or grey. They can appear raised or flat, with either a smooth or rough texture.
Cauliflower-like clusters:
Several warts may grow together, forming a cluster that resembles a small cauliflower.
Itching or mild discomfort:
You might feel a persistent itch or slight irritation where the warts are present.
Light bleeding during intimacy:
If warts are rubbed during sexual activity, they may bleed slightly. This happens when the delicate skin is disturbed.
Some genital warts are so small and flat they're nearly invisible. Even when you can't see them, the infection may still be present. That is why regular check-ups are important, as they help pick up changes early, even when everything seems normal.
How genital warts differ in women and men
The location and experience of genital warts can differ between women and men. Here's what you should look for:
Genital warts in women
In women, warts can appear on the external or internal genital area, including:
Vulva or vaginal walls:
Labia, clitoris, vaginal opening, or inside the vagina and may be noticed during washing or self-checks.
Cervix:
Often not visible without a pelvic examination.
Around the anus:
Can occur even without anal intercourse, as HPV may spread from nearby skin.
Some women also experience itching, burning, or unusual discharge. Even though the strains causing warts are usually low-risk, regular Pap smears remain important because other HPV strains can cause cervical cell changes.
Genital warts in men
For men, genital warts are also common and treatable, and they tend to show up on:
Penis or scrotum:
On the shaft, head, foreskin, or scrotal skin.
Groin or upper thighs:
Especially along skin folds where friction occurs.
Around or inside the anus:
More common with anal intercourse, but HPV can spread through skin-to-skin contact.
What causes genital warts and how are they spread?
Genital warts are caused by certain strains of HPV, most commonly types 6 and 11. These are known as low-risk strains because they don't cause cancer.
The low-risk HPV strains that cause genital warts are different from the high-risk strains (like types 16 and 18) linked to cervical cancer. Having genital warts doesn't mean you have a cancer-causing strain.
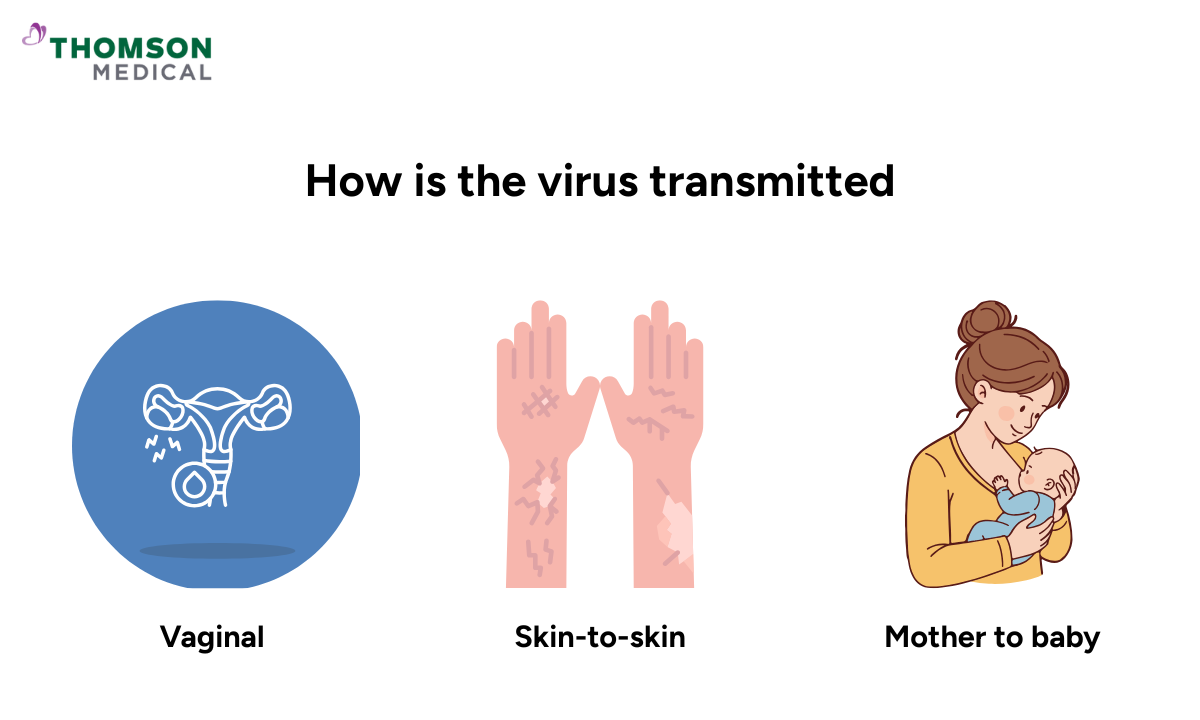
How HPV spreads
HPV is very common and spreads through intimate skin-to-skin contact. Here's how transmission happens:
During sexual activity:
The virus spreads through vaginal, anal, or oral intercourse. You can also get it from genital touching, even without penetration.
Skin-to-skin genital contact:
Because HPV lives in skin cells, close genital contact is enough to pass it from one person to another.
From mother to baby (rare):
In uncommon cases, a mother with genital warts can pass the virus to her baby during vaginal delivery.
HPV is incredibly common. In fact, most sexually active people will have some form of HPV at some point in their lives. It's so easily spread that even protected sexual activity doesn't guarantee complete prevention, though condoms do reduce your risk.
Our sexual health specialists in Singapore
Loading...
How are genital warts diagnosed?
Getting a diagnosis is straightforward and helps you understand your next steps. Your doctor will use one or more of these methods:
Physical examination:
In most cases, your doctor can diagnose genital warts by simply looking at the affected area.
They'll check for the characteristic appearance of warts on your genitals, groin, or anal area.
Colposcopy (for women):
If your doctor needs a closer look at your cervix or vagina, they may suggest a colposcopy. This uses a special magnifying instrument to examine areas where warts might be too small to see with the naked eye.
Biopsy (in rare cases):
If the diagnosis isn't clear, the warts look unusual, or they haven't responded to treatment, your doctor might take a small tissue sample.
This is sent to a laboratory to confirm what's happening and rule out other conditions.
Treatment options for genital warts
While there's currently no definitive cure for HPV itself, the warts it causes can be effectively treated and managed. Your doctor will recommend the best approach based on the size, number, and location of your warts.
Topical prescription medications
These are creams or solutions you apply at home, such as imiquimod, podophyllotoxin, or trichloroacetic acid (TCA). They work by helping your immune system fight the virus or by breaking down the wart tissue.
In-clinic procedures
Cryotherapy:
Freezing the warts with liquid nitrogen so they blister and fall off.
Electrocautery:
Using an electric current to burn away the warts.
Surgical removal:
Removing larger or stubborn warts with a scalpel under local anaesthetic.
Laser treatment:
Using an intense beam of light to destroy extensive or difficult-to-treat warts.
Warts may come back after treatment because the virus can stay dormant in your skin. You might need several sessions to achieve clear skin, and that's completely normal.
If you’re experiencing symptoms that could be genital warts, request an appointment with us today and our specialists can help to find the right treatment for your condition.
Preventing genital warts
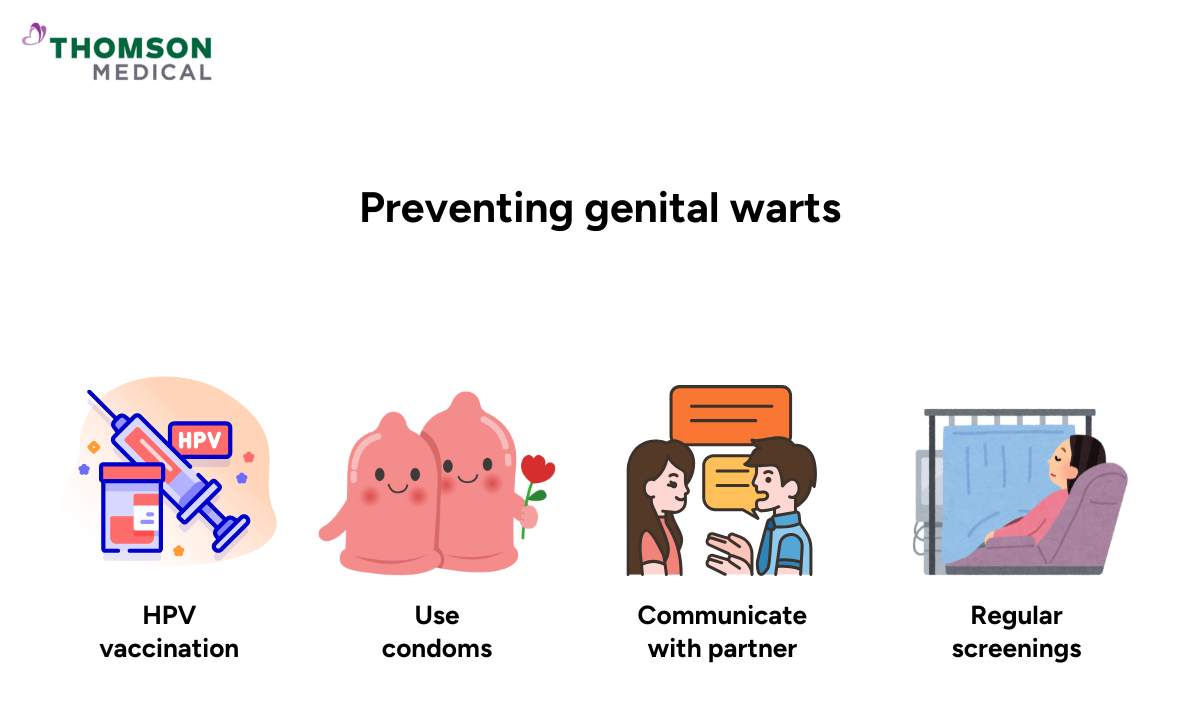
While genital warts are common and treatable, taking steps to protect yourself can reduce your risk of getting HPV.
HPV vaccination
The most effective prevention method is the HPV vaccine. It protects against the strains that cause most genital warts (types 6 and 11) and high-risk strains linked to cervical cancer. It works best when given before becoming sexually active but can still offer protection afterwards. HPV vaccination is for:
Young people, ideally before age 26
Both women and men
Speak with your doctor to see if it's right for you
Safer sex practices
Use condoms:
While they don't provide complete protection, condoms significantly reduce your risk.
Communicate openly:
Talk with partners about sexual health and STI testing
Get regular screenings:
Women should have routine cervical screening to detect early changes.
If you have genital warts
Avoid sexual contact when warts are visible
Inform partners so they can get checked if needed
Wait until your doctor confirms treatment is complete
Taking preventive steps isn't just about protecting yourself, it's about looking after your long-term health and wellbeing.
FAQ
Are genital warts cancer?
No, genital warts are not cancer. They're caused by low-risk HPV strains (types 6 and 11), which are completely different from the high-risk strains linked to cancer.
What do genital warts look like?
They can show up differently for different people:
- Small bumps that might be flesh-coloured, pink, or whitish
- Single spots or clusters that sometimes look a bit like cauliflower
- Occasionally so small you can barely see them
Can genital warts be cured?
Genital warts can usually be treated effectively, and many people see them clear with the right care. While treatments remove the warts, HPV may still remain in the body for a period of time. In many cases, the immune system suppresses or clears the virus naturally within about one to two years.
Does having genital warts mean you have an STI?
Yes, genital warts are an STI caused by HPV. Some people carry HPV without any symptoms for a long time, so warts can appear even when you haven’t had recent new partners. If you’re unsure, a clinician can confirm what’s going on and guide you on the next steps.
Should you be worried if you have genital warts?
Feeling worried is completely understandable, but genital warts are both treatable and manageable. With regular check-ups and safe practices, you can protect your health and your partner's too. You've already taken an important step by learning about this and seeking care.
Is HPV for life?
Not always. Many people's bodies clear the virus naturally within two years. For others, it might stay dormant, which can mean warts occasionally return. Either way, with the right care, you can manage it well.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
