Being told you have a haemorrhagic ovarian cyst can feel unsettling, particularly if it followed issues such as sudden pelvic pain. It is completely natural to feel concerned and want clear answers about what this means for your health.
The good news is that most haemorrhagic ovarian cysts are not serious and often resolve on their own without treatment. Learning how they develop, what symptoms to monitor, and when follow-up is needed can help ease uncertainty and support your peace of mind.
What is a haemorrhagic ovarian cyst?
A haemorrhagic ovarian cyst is a type of functional ovarian cyst that contains blood. It begins as a normal cyst formed during your menstrual cycle, but bleeding occurs when a small blood vessel within the cyst wall ruptures, allowing blood to collect inside the cyst.
These cysts are typically benign (non-cancerous) and not considered a sign of ovarian cancer. They are most commonly seen in teenagers and women of reproductive age who ovulate regularly.
Haemorrhagic ovarian cysts aren’t usually a disease. They often happen as part of the normal way your ovaries work during your menstrual cycle. In most cases, your body naturally absorbs the blood and fluid, and the cyst clears up on its own without needing any treatment.
What causes haemorrhagic ovarian cysts?
Haemorrhagic ovarian cysts develop as part of your normal ovulation process and are not caused by pelvic inflammatory disease or poor lifestyle choices.
Normal ovulation:
Regular ovulation is the main factor, as these cysts form during your natural menstrual cycle.
Hormonal changes:
Natural shifts in your hormone levels can sometimes make a small blood vessel more likely to bleed inside a cyst.
Irregular menstrual cycles:
If your cycles are irregular, hormone fluctuations may be less predictable, which can increase the chance of a cyst forming.
Your risk may be slightly higher if you are using fertility medications or undergoing in vitro fertilisation, or if you have had functional ovarian cysts in the past.
This can understandably bring you concerns, especially when you are already navigating fertility treatment or previous health experiences. It is important to remember that a higher risk does not mean something serious will occur, and many people in these situations go on without complications.
How does a haemorrhagic ovarian cyst develop?
Your ovaries and fallopian tubes are part of a dynamic system that responds to hormonal changes every month to prepare for potential pregnancy. When you have a haemorrhagic ovarian cyst, it is often the result of this normal monthly process.
Follicle formation:
Each month, your ovary forms a small follicle to hold and release an egg as part of your menstrual cycle.
After ovulation:
After the egg is released, this follicle changes into the corpus luteum, which produces hormones to support the rest of your cycle.
Minor bleeding:
Occasionally, a small blood vessel within this structure can break. When this happens, bleeding occurs inside the cyst.
Blood collection and pain:
As blood collects within the cyst, it can stretch the tissue around it, which is why you may feel pelvic pain or discomfort on one side.
Although this experience can be worryingly uncomfortable, it is a common and natural variation of the menstrual cycle and does not mean that something is wrong with your ovaries.
What are the common symptoms?
Many people have no symptoms at all, and the cyst is only discovered incidentally during ultrasound imaging for something else. However, because these cysts contain blood, they can sometimes trigger more noticeable symptoms than a simple fluid-filled sac, including:
A sharp or dull pelvic pain, often localised specifically to one side
A persistent feeling of bloating or heavy pressure in your lower pelvic area
Light vaginal bleeding or spotting between your regular periods, while less common
Discomfort during exercise, sudden movements, or sexual intercourse
Although these symptoms can feel uncomfortable, they are usually temporary. In most cases, your body gradually reabsorbs the blood and the cyst heals naturally over time. Many people find that their symptoms steadily improve without the need for further treatment.
If you experience any of these symptoms or notice changes in your pelvic health, schedule a consultation with Thomson Medical today to get a proper evaluation and personalised guidance.
How it differs from other ovarian cysts
It can be helpful to understand how haemorrhagic ovarian cysts differ from other growths. Your doctor will use clear guidelines and detailed imaging to distinguish between them, helping ensure you receive the right care for your specific situation.
Cyst type | Primary content | Characteristics | Typical outcome |
Haemorrhagic cyst | Blood | Linked to the corpus luteum; often causes pain. | Usually resolves within 1–2 cycles. |
Simple cyst | Clear fluid | Thin-walled; the most common type of functional cysts. | Frequently resolves on its own. |
Dermoid cysts | Tissue/Fat | Dermoid cysts contain tissue like hair or skin and are not cycle-related. | Does not resolve; may need removal. |
Endometriomas | Old blood | Known as "chocolate cysts", linked to endometriosis. | Can be persistent and may need surgery. |
When your cyst is clearly identified, your medical team can avoid unnecessary surgery and focus on gentler options instead. This helps protect your body and reduces disruption to your everyday life.
How are haemorrhagic ovarian cysts diagnosed?
The aim of diagnosis is to confirm that the cyst is benign and to check that it is resolving in a healthy way. Each step helps your doctor decide on the safest and least invasive approach for your care.
A review of your symptoms and how you have been feeling
A discussion about your medical history
A pelvic examination, if needed, to check for tenderness or unusual findings
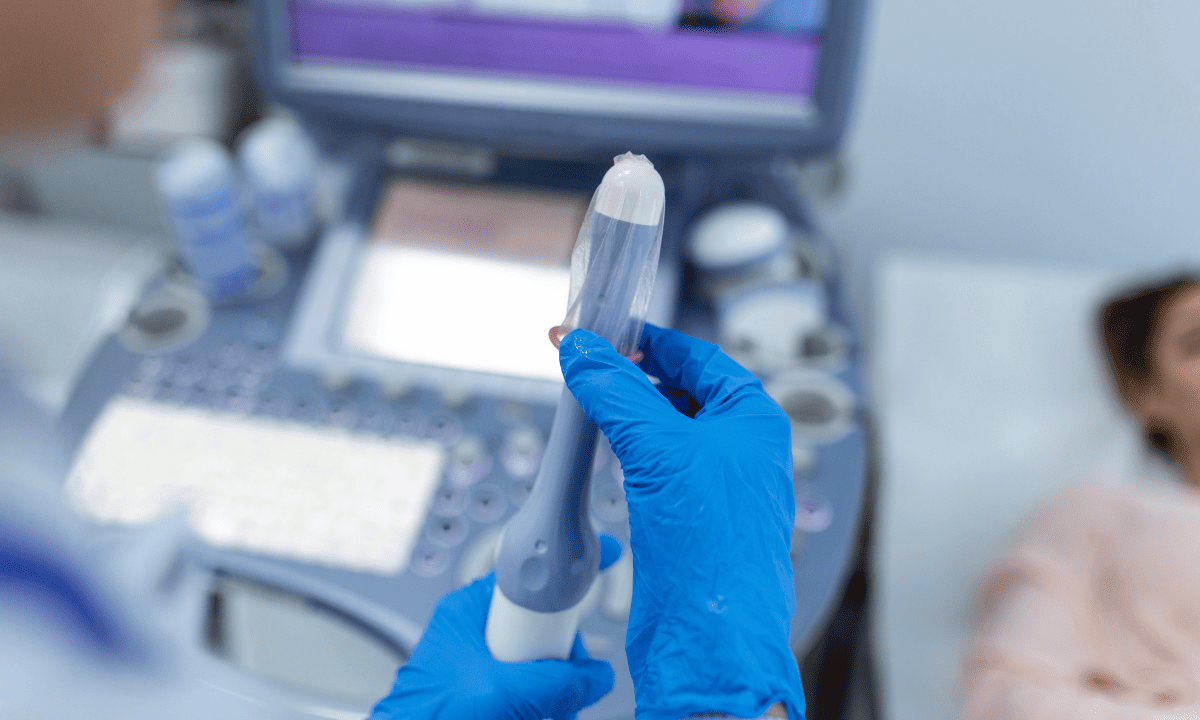
A transvaginal ultrasound, which provides a clear view of the ovaries
A colour Doppler ultrasound, sometimes used to confirm healthy blood flow to your ovary
Further scans, such as CT scans, are rarely needed and are only considered if your doctor feels they would be helpful. Blood tests may sometimes be used to provide reassurance and rule out other concerns, although levels can naturally be higher during your reproductive years.
If you’re experiencing pelvic discomfort or suspect an ovarian cyst, schedule a consultation with a doctor at Thomson Medical to get an accurate diagnosis and personalised care plan.
How to treat haemorrhagic ovarian cysts?
Most haemorrhagic ovarian cysts do not need surgical removal. In many cases, treatment focuses on giving your body time to heal naturally while keeping you comfortable and safe.
Observation and monitoring
The most common approach is "watchful waiting", as most cysts naturally shrink and disappear within 1–2 menstrual cycles. During this time, it is advised that you should:
Attend a follow-up ultrasound scan after six to eight weeks to confirm the cyst is disappearing
Avoid strenuous activity for a short time to lower the risk of an ovarian cyst rupture
Allow your body time to naturally reabsorb the blood inside the cyst
This period of monitoring supports your body’s natural healing and helps you avoid unnecessary medical procedures.
Pain management at home
If you are experiencing discomfort, there are several gentle ways to manage the pain as you wait for the cyst to resolve:
Use warm compresses or a warm water bottle on your lower abdomen to help relax pelvic muscles and ease cramping.
Take over-the-counter pain relievers or prescription medicine if needed.
Some people explore herbs or vitamins to support hormonal balance, but always check with your specialist first.
Taking these steps to manage your physical comfort can make the waiting period much easier and help you maintain your daily quality of life.
Hormonal therapy
In some cases, your doctor may suggest hormonal birth control to help support your recovery, as it can help:
Prevent new cysts from forming by stopping ovulation
Regulate your menstrual cycles
Even though hormonal therapy does not treat or remove an existing cyst, it can reduce your chance of future cysts developing.
Surgical intervention
While surgery is rare, your doctor may recommend it if there are signs that your body needs extra help.
You may be advised to have surgery if:
The cyst causes your ovary to twist (ovarian torsion)
The cyst ruptures and causes significant internal bleeding
The cyst grows very large and continues to cause pain or pressure
Your diagnosis do not clearly confirm that the cyst is benign
While these complications are rare, knowing the signs allows you to act quickly and ensures you receive the best possible care if needed. Many people also find reassurance in learning how to support their body and lower the chance of future problems. Taking simple, proactive steps can help you feel more in control of your health moving forward.
How to prevent haemorrhagic ovarian cyst
Haemorrhagic ovarian cysts cannot be fully prevented. However, there are a few practical steps you can take to help with effective monitoring and care.
Attend regular check-ups so any changes can be monitored early
Keep track of your menstrual cycle and note any new or unusual symptoms
Manage underlying hormonal conditions with your doctor’s guidance
Follow recommended treatment plans if cysts recur
There is no diet or exercise routine that can fully prevent these cysts. What matters most is staying informed and supported throughout your journey. When you understand what is happening in your body and what signs to look out for, it can reduce anxiety, help you recognise changes early, and give you confidence when making decisions about your care.
When to see a doctor

You should contact a healthcare provider right away if you notice any of the following:
Pain that is severe or steadily getting worse
Pain that lasts more than a few days
Sudden changes in your periods
Feeling fatigued, dizzy, or generally unwell
Similar symptoms that make you feel worried or unsure
Our gynaecologic oncology specialist
Loading...
FAQ
Can a haemorrhagic ovarian cyst go away on its own?
Yes. In most cases, it does. Haemorrhagic ovarian cysts are functional cysts, meaning they form as part of your normal menstrual cycle. Most resolve naturally within one or two cycles, around four to eight weeks, as your body slowly reabsorbs the blood and the cyst shrinks.
What causes bleeding inside the cyst?
During ovulation, a small blood vessel in the cyst wall, usually in the corpus luteum, can break. Because the cyst is a closed sac, the blood collects inside instead of draining away. This can stretch the cyst and lead to pain or discomfort.
How is a haemorrhagic cyst different from a chocolate cyst?
A haemorrhagic cyst contains fresh blood and is temporary. It usually disappears on its own. A chocolate cyst, also known as an endometrioma, contains older, darker blood and is linked to endometriosis. These cysts tend to last longer and rarely resolve without treatment.
What should I do if I think the cyst has ruptured?
A rupture can cause sudden, sharp pain. Many small ruptures settle with rest and pain relief. However, a large rupture can cause significant internal bleeding. If you feel faint, develop a fever, or the pain is severe and does not improve, seek emergency medical care immediately.
Will this affect my future fertility?
In most cases, no. Haemorrhagic cysts do not usually damage your ovaries or fallopian tubes. If surgery is ever needed, your surgeon will aim to preserve as much healthy ovarian tissue as possible to protect fertility.
Can I prevent these cysts from coming back?
You cannot fully prevent haemorrhagic cysts through diet or exercise because they are linked to ovulation. In some cases, your doctor may recommend hormonal birth control to stop ovulation, which can help prevent new functional cysts from forming.
Is a haemorrhagic ovarian cyst cancerous?
No. Haemorrhagic cysts are benign (non-cancerous). They have distinct features on ultrasound, often described as lace-like or cobweb patterns, which are very different from the appearance of ovarian cancer. Your doctor may still monitor them closely to ensure they resolve as expected.
When is surgery necessary?
Surgery is uncommon and usually only considered if:
The cyst is very large, typically over five to ten centimetres.
There is a risk of ovarian torsion.
A rupture causes dangerous internal bleeding.
For most people, haemorrhagic cysts resolve without surgery and can be managed safely with monitoring and care.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment