If you've been diagnosed with herpes, you may be worried about what this means for your intimate relationships and daily life. Will you experience frequent outbreaks? Is there a risk of passing it on to your partner?
While these concerns are valid, antiviral medications and prevention strategies can help you manage outbreaks and significantly reduce the risk of transmission, enabling you to maintain healthy intimate relationships.
What is herpes simplex virus (HSV) infection?

Herpes is one of the most common viral infections, and many people carry it without realising. It's caused by the herpes simplex virus (HSV), which comes in two types, HSV-1 and 2. These viruses can cause sores or blisters, known as outbreaks, that may appear on:
The mouth (oral herpes)
The genitals (genital herpes)
Other parts of the body
What causes HSV infection?
HSV infection is caused by the herpes simplex virus, which spreads through close personal contact. Understanding how HSV spreads can help you feel more informed and in control:
Direct skin-to-skin contact during kissing or sexual activity
Contact with infected skin or mucous membranes
HSV can also spread even when there are no visible sores, because the virus can sometimes “shed” from the skin (asymptomatic shedding). Once the virus enters your body, it’ll often stay dormant for long periods in your nerve cells, and many people experience few or no outbreaks over time.
Types of herpes
While herpes can't be fully cured, it can be managed effectively. Antiviral medications help keep outbreaks minimal and reduce transmission risk, allowing you to maintain your health and quality of life. Herpes can affect different parts of your body depending on the type of virus. Here's a table to help you understand the main types of herpes:
| Type | What it affects | How it spreads | Common symptoms | What you should know |
|---|---|---|---|---|
| Genital herpes (HSV-2) | Genitals, anus, and nearby skin | Vaginal, oral, or anal sex
Can spread without visible sores | Painful blisters or sores
Flu-like symptoms (first outbreak)
Discomfort urinating
Swollen lymph nodes | Not everyone has symptoms. Outbreaks vary in frequency. |
| Oral herpes (HSV-1) | Mouth and lips | Kissing
Sharing utensils or lip balm
Most contagious during outbreaks | Cold sores or blisters around mouth
Tingling before outbreak | This herpes type is most contagious during outbreaks and most people have HSV type 1 by adulthood. |
| Herpetic whitlow | Fingers and thumbs | Direct contact with infected sores
Through breaks in skin | Intense pain and swelling
Reddened, tender blisters near fingernails | Healthcare workers and children are at higher risk. |
How do you know if you have herpes?
The only certain way to know if you have herpes is through testing. Many people show no symptoms or experience very mild signs that are easy to miss.
Common herpes symptoms to watch for:
Tingling, itching, or burning sensations around the genital area, anus, or mouth (often before sores appear)
Painful, fluid-filled blisters, or sores in these areas
Sores that break open, crust over, and heal within a few weeks
Flu-like symptoms during the first outbreak (fever, body aches, or swollen lymph nodes)
Some people with herpes never have visible sores but can still pass the virus to others. This is why testing is so important, especially if you're sexually active or concerned about exposure.
If you're concerned about herpes or want to get tested, our O&G specialists at Thomson Medical are here to help. Request an appointment with Thomson Medical for personalised care and support.
Our sexual health specialist in Singapore
Loading...
What are the different stages of a herpes infection?
A herpes infection progresses through three main stages, primary infection, latency, and reactivation. Knowing these stages can help you recognise what's happening in your body and manage symptoms more effectively.
Stage 1: Primary infection
This is when HSV first enters your body. For many people, this stage passes without any symptoms at all. If symptoms do show up, you might notice:
Fever and body aches
Blisters or sores around the mouth (oral herpes) or genitals (genital herpes)
The first outbreak usually lasts a few weeks. While it can feel uncomfortable, it's simply your body responding to the virus.
Stage 2: Latency (dormant phase)
After the initial infection, the virus settles into nerve cells and becomes inactive. During this time, it causes no symptoms and can't spread to others. Many people stay in this quiet phase for months or even years without experiencing any outbreaks.
Treatment options of herpes
Whilst there's currently no definitive cure for herpes, outbreaks can be managed effectively with the right medication and self-care. Many people experience fewer and milder outbreaks over time.
Antiviral medications:
Antiviral drugs reduce the severity and duration of outbreaks. Common options include:
Aciclovir
Famciclovir
Valaciclovir
These work best when taken at the first sign of symptoms like tingling or itching.
Pain management:
Over-the-counter pain relievers such as paracetamol or ibuprofen can help ease discomfort during outbreaks.
Suppressive therapy:
For frequent or severe outbreaks, your doctor may recommend daily antiviral medication to reduce recurrence and lower transmission risk.
Self-care measures:
Keep affected areas clean and dry
Wear loose and breathable clothing
Apply a cold compress to reduce pain and swelling
Get plenty of rest
With the right treatment and self-care, you can manage herpes confidently.
When to seek for medical advice
You don't have to face this alone. Seeking medical advice early can give you clarity, relief, and the right treatment to help you feel better sooner. You should see a healthcare provider if you:
Notice unusual sores, blisters, or painful bumps around your mouth, genitals, or other areas
Experience tingling, burning, or itching that feels different from normal
Have flu-like symptoms (fever, body aches, or swollen glands) along with sores
Think you may have been exposed to herpes through intimate contact
Are pregnant or planning to conceive and have genital herpes
Since everyone's experience with herpes is unique, a consultation with a specialist can provide the personalised care you need. Request an appointment with Thomson Medical for support and guidance.
How to prevent herpes transmission
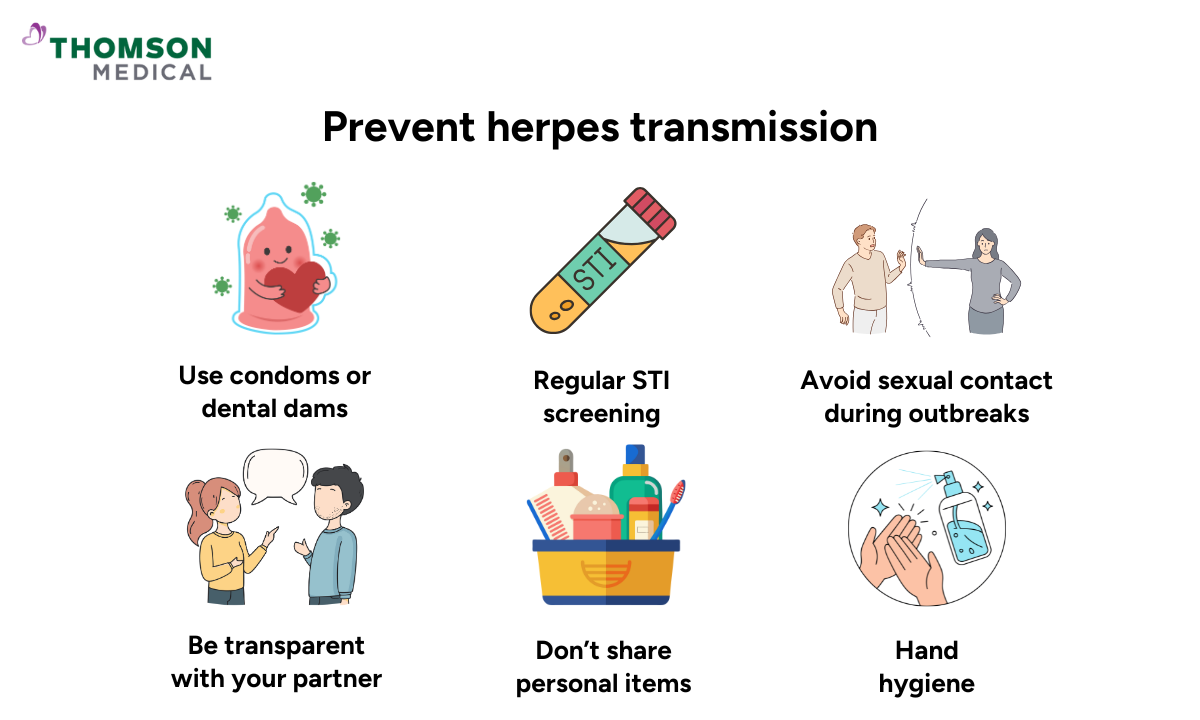
While herpes is common and manageable, taking steps to reduce transmission can protect both you and your partner. Here's what you can do to lower your risk.
If you don’t have herpes:
Practice safe intercourse by using condoms or dental dams
Avoid intimate contact when your partner has visible sores or symptoms
Ask partners about their sexual health history
Consider regular STI screening if you're sexually active
Don't share personal items like lip balm, utensils, or razors
Wash your hands regularly, especially after touching affected areas
If you have herpes:
Use condoms consistently, even when you don't have visible sores (the virus can still spread through asymptomatic shedding)
Avoid sexual contact during outbreaks or when you notice early warning signs like tingling
Take daily antiviral medication (suppressive therapy) to reduce transmission risk
Have an open, honest conversation with your partner about your diagnosis
Avoid kissing if you have oral herpes sores
For pregnant women:
If you have genital herpes and are pregnant or planning to conceive, speak with your healthcare provider. They can help manage your condition safely to protect your baby during pregnancy and delivery.
FAQ
Can herpes be cured?
There's currently no definitive cure for herpes, as the virus stays in your body for life. However, it can be managed effectively. Antiviral medications like aciclovir, famciclovir, and valaciclovir can:
Make outbreaks shorter and less severe
Reduce how often they happen
Lower the chance of passing it to your partner
Starting treatment at the first sign of symptoms leads to quicker recovery. With proper care, you can live comfortably while managing herpes.
Is herpes an STI?
Yes, genital herpes is a sexually transmitted infection. It spreads through skin-to-skin contact during sexual intercourse, including vaginal, oral, and anal contact.
What can be mistaken for herpes?
Several conditions can look similar to herpes, which is why accurate diagnosis matters. Common conditions that may be mistaken for herpes include:
Genital warts (HPV)
Ingrown hairs or shaving irritation
Yeast infections
Insect bites
Folliculitis
If you're not sure about any symptoms, you can speak with a healthcare provider for proper testing.
What cream can be used for herpes?
Aciclovir cream works well when you apply it at the first sign of symptoms like that telltale tingling or burning. Your doctor can help you find what works best for your situation.
How can you get rid of herpes sores quickly?
The fastest way is to start antiviral medication like aciclovir as soon as you feel symptoms coming on. It helps sores heal quicker and eases the discomfort while you recover.
Can you live a normal life with herpes?
Absolutely. Many people live full, active lives whilst managing herpes. You can still have healthy relationships, enjoy intimacy, pursue your goals, and have children with proper medical support. The diagnosis might feel overwhelming at first, but with the right care, herpes becomes just a small part of your life, not something that defines you. You can live fully and confidently.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
