Many couples who have trouble conceiving naturally explore different fertility treatments such as intrauterine insemination (IUI). This procedure can improve the chances of fertilisation, but its success depends on several key factors.
In this article, we’ll explain what affects IUI success rates and help you make informed choices on your journey to becoming parents.
What is IUI?
IUI for women is a fertility treatment where doctors put washed and concentrated sperm directly into a woman's womb during ovulation. This procedure is done to ensure that enough healthy sperm reaches the egg, allowing it to be fertilised more easily.
IUI is less invasive and more affordable than in vitro fertilisation (IVF). Because of this, doctors often recommend it as a first fertility treatment. A fertility clinic usually performs IUI under medical supervision. Doctors may combine it with ovulation-inducing medication to improve results.
Who are the good candidates for IUI?
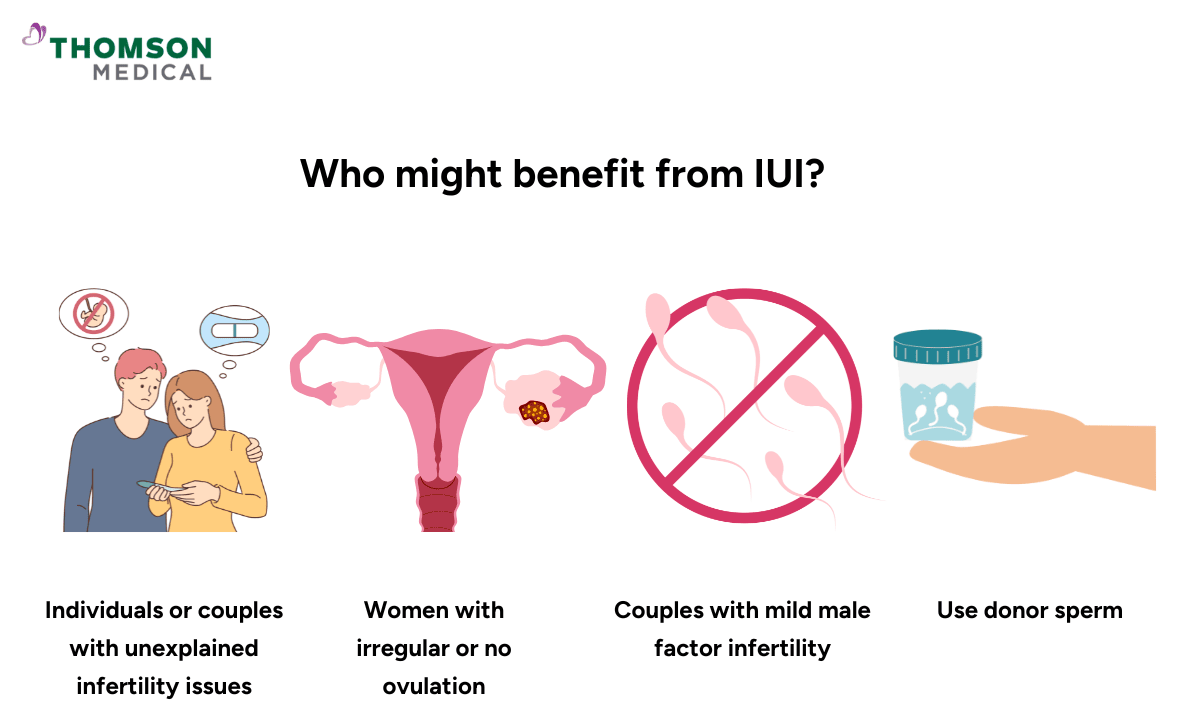
The following people are considered good candidates for IUI:
Couples with mild male infertility, such as low sperm count or motility
Women experiencing cervical problems or mild endometriosis
Women have irregular or absent ovulation, such as with polycystic ovary syndrome (PCOS)
Individuals with unexplained infertility after undergoing standard fertility tests
LGBTQ+ individuals or single women using donor sperm
Couples experiencing ejaculation issues or sexual dysfunction
What affects intrauterine insemination success rates?
IUI success rates, on average, range from 5% to 20% per cycle. Factors such as the patient's age, fertility diagnosis, and treatment plan influence these rates.
Among the factors affecting success rates, younger women and those using fertility medications usually have higher success rates. Conversely, the success rate is lower for older women or those who rely on natural cycles, which are cycles without fertility drugs.
In addition to age and fertility treatments, proper timing, sperm quality, and the number of cycles attempted all play a critical role in improving outcomes.
Age of the individual undergoing treatment
For individuals under 35, the chances per cycle are usually highest, ranging from about 10% to 20%.
Ages 35–40 see moderate success rates (10–15%).
Over 40, success drops to around 5% or less, mostly because egg quality naturally declines with age.
Cause of infertility
Couples with unexplained infertility often respond well to IUI.
If the issue is with your sperm, such as a lower count or motility, the odds depend on those numbers.
For ovulation difficulties, medication to help control ovulation can improve your chances.
Use of fertility medications
A "natural cycle" IUI (no medication) is less likely to work than a cycle with medication.
Medicines like Clomid or gonadotropins can help to stimulate cycles and increase the number of follicles, which improves the chances of conception.
Sperm quality and total motile sperm count
For IUI, the ideal post-wash motile sperm count is usually considered to be a value greater than 10 million.
Under 5 million motile sperm tends to lower the chance of success.
Healthy fallopian tubes
Since fertilisation occurs in the fallopian tubes, at least one of them must be open and functional for IUI to work.
If both tubes are blocked or severely damaged, IUI is unlikely to help, and IVF may be considered instead.
Timing and monitoring of ovulation
For success, insemination must be carefully timed with ovulation.
Monitoring through ultrasounds or hormone tests ensures that sperm are introduced when the egg is released, thereby increasing the chances of conception.
The hCG "trigger shot" helps time the IUI perfectly, ensuring it occurs at the right moment during the woman's fertile window.
Number of IUI cycles attempted
Success improves over time because each additional IUI cycle increases the cumulative chances of pregnancy.
Many couples conceive within 3–6 treatment cycles.
For more personalised information about whether IUI is the right fertility treatment for you, and to discuss your unique situation, consider consulting a fertility specialist. You can contact Thomson Medical to arrange a consultation and receive expert guidance tailored to your fertility needs and treatment options.
Our fertility specialists
Loading...
Comparison of IUI success statistics: natural vs medicated cycles
Cycle type | Success rate | Notes |
Natural IUI | 4–10% | Best for younger women with regular ovulation cycles. |
Clomid/Letrozole | 10–15% | It enhances ovulation and increases the number of available eggs. |
Injectables (FSH/gonadotropins) | 15–20% | The risk of twins or multiples increases with higher pregnancy rates. |
How to maximise your IUI chances of success?
Use fertility medications if your doctor suggests them:
Medicines can stimulate the ovaries to produce more eggs, which increases the chances of fertilisation during IUI.
Ensure accurate ovulation timing:
Success depends on performing IUI at the right moment—just before or during ovulation. Regular monitoring with scans and hormone tests ensures correct timing.
Optimise sperm health:
Lifestyle choices strongly affect sperm quality. Avoid smoking, limit alcohol, and minimise heat exposure (like hot baths) to improve sperm motility and sperm count for IUI.
Maintain a healthy Body Mass Index (BMI):
Both underweight and overweight conditions can disrupt hormone balance and ovulation, reducing the chances of conception. Keeping your weight in a healthy range supports fertility.
Manage stress effectively:
High stress can interfere with hormone regulation. Practices like yoga, meditation, counselling, or mindfulness can help you stay calm and positively impact fertility treatment outcomes.
Follow your clinic’s instructions carefully:
Each step, from taking medications to coming in for scheduled monitoring, plays a vital role. Strictly following medical guidance ensures maximum benefit from your IUI cycle.
When should I consider IVF instead?
After 3–6 unsuccessful IUI cycles:
If several attempts do not result in pregnancy, IVF may be the more effective next step.
Women over the age of 38–40:
Egg quality and ovarian reserve decline with age, and IVF generally provides higher success rates compared to IUI for older women.
Severe male factor infertility:
If sperm counts, motility, or morphology are too low for IUI, IVF with ICSI (intracytoplasmic sperm injection) offers a better chance of conception.
Presence of tubal blockages:
Since fertilisation cannot occur if both fallopian tubes are blocked, IVF is needed because it bypasses them completely.
Situations requiring advanced techniques:
Couples who require genetic testing of embryos (preimplantation genetic testing – PGT) or who plan embryo freezing for the future will benefit more from IVF.
FAQ
How does age affect the IUI success rate?
Success rates are closely linked to a woman’s age. Younger women, especially those under 35, generally have higher chances of success. After 35, both egg quality and ovarian reserve (the number of eggs remaining) begin to decline, which lowers the chances of pregnancy with IUI.
Does IUI increase the chance of pregnancy?
Yes, IUI can increase the chances of pregnancy by placing prepared sperm directly into the uterus during ovulation. This artificial insemination procedure increases the likelihood of sperm meeting the egg compared to timed intercourse. IUI helps especially with mild male fertility issues. It also helps with unexplained infertility or problems with the cervix.
What is the IUI success rate per cycle by age, specifically for women under 30 and for those over 40?
Women under 30 often have IUI success rates close to 15–20% per cycle. Women over 40 usually have much lower success rates, often below 5%. This drop happens mainly because their egg quality decreases.
How does the success rate of the second IUI compare to the first?
The success rate for a second IUI cycle is generally similar to that of the first, but it may slightly decrease based on individual factors. Success rates often improve over several cycles, with many couples conceiving by the third to sixth attempt.
Can lifestyle changes improve IUI success?
Yes, simple lifestyle adjustments can make a noticeable difference in fertility outcomes:
Eating a balanced, nutrient-rich diet
Exercising regularly (but avoiding excessive workouts)
Avoiding smoking, alcohol, and recreational drugs
Reducing stress through yoga, meditation, mindfulness, or counseling
What are the next steps after failed IUI cycles?
A failed cycle does not signify the end of your fertility journey. Next steps may include:
Re-evaluating your treatment plan with your fertility specialist
Adjusting medications or protocols
Performing additional tests to rule out hidden causes
Considering advanced treatments such as IVF if needed
What are the signs of a successful IUI?
Some women may notice early pregnancy-like symptoms, but they are not always reliable. Possible signs or symptomps of successful IUI include:
Mild abdominal cramping or spotting (implantation-related)
Breast tenderness or bloating due to hormonal changes
A positive pregnancy test is the only sure way to confirm pregnancy. Doctors usually do this test about 14 days after the IUI procedure.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
For more information, contact us:
Thomson Fertility
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Request an Appointment