You have been experiencing a dull ache in your lower abdomen, particularly when you urinate or during intercourse. At first, you might dismiss it as period cramps or a minor issue such as constipation or bloating. However, if the discomfort persists, these symptoms could be an early sign of pelvic inflammatory disease (PID).
To help protect your reproductive health and prevent complications, you can take proactive steps by learning about its causes, warning signs, risk factors, and treatment options.
What is pelvic inflammatory disease (PID)?
PID is a severe infection of female reproductive organs that can occur at any age but is most common in women between 15 and 25 years old. It is an infection that affects your uterus (womb), fallopian tubes, and ovaries. It usually happens when bacteria from the vagina or cervix move up into the pelvic area. Without treatment, it can lead to long-term health issues like chronic pelvic pain, infertility, or ectopic pregnancy.
Causes of PID
PID occurs when bacteria move up from the vagina or cervix into the uterus, fallopian tubes, or ovaries that can lead to infection and swelling. There are many different microorganisms that can cause PID, which include:
Sexually transmitted infections (STIs)
STIs or microbes linked to bacterial vaginosis cause PID in 85% of cases. Chlamydia trachomatis and Neisseria gonorrhoeae are the most common germs that cause disease. These bacteria can infect the cervix without showing any signs and then move up, hurting the delicate lining of the reproductive organs. Without early treatment, even mild infections can progress into PID.
Normal vaginal bacteria
Not all cases of PID are caused by STIs. Bacteria that normally live in the vagina can sometimes grow and spread up to the uterus and fallopian tubes. This is more likely to happen when the balance of vaginal flora is disrupted, like after douching (washing your vagina), taking antibiotics, or hormonal imbalance.
Medical procedures
Any procedure that opens a pathway from the vagina to the uterus can allow bacteria to enter. For example:
Having an intrauterine device (IUD) inserted, especially if you do it when you have an STI that hasn't been diagnosed yet.
Gynaecological procedures such as endometrial biopsy, termination of pregnancy, or dilation and curettage.
Following miscarriage or childbirth, when the cervix is open and bacteria can easily move up.
PID risk factors
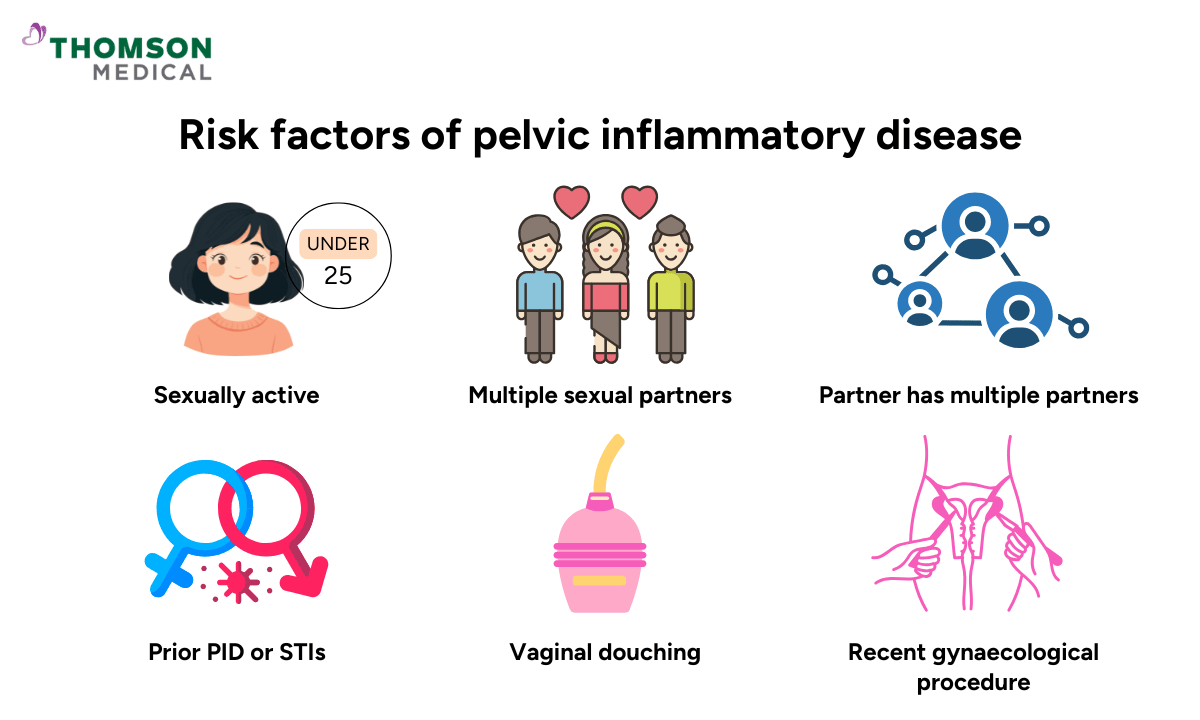
According to these causes, you are more likely to develop PID if:
You are sexually active and under 25 years old
You have multiple sexual partners
You have a partner with multiple partners
You have had PID or STIs before
You practise vaginal douching (washing your vagina)
You have recently had a gynaecological procedure
Symptoms of PID
Different women can have different symptoms of PID. Some women may only feel a little bit of pain or no symptoms at all, which makes it easy to miss the condition. Others may have sudden, severe pain and other signs of an infection.
Lower abdominal pain
This is often the most common complaint. The pain could be dull and constant, or it could come on suddenly and be sharp. It usually hurts in the lower belly, just below the navel, and sometimes radiates to the lower back or thighs. PID pain is often on both sides of the body, can be mild to severe, and may get worse during physical activity, urination, or menstruation.
Pain during intercourse
A lot of women say they feel discomfort or pain during sexual intercourse, particularly with deep penetration, which may be linked to inflamed pelvic tissues.
Painful urination
If inflammation or infection spreads to nearby urinary structures, you may feel pain or a burning sensation when passing urine. You may also need to urinate more frequently than usual.
Abnormal vaginal discharge
You might have an abnormal discharge if you have PID. The discharge might be thicker than usual and have a yellow or green colour and an unpleasant smell, which could mean an infection.
Irregular menstrual bleeding or spotting
Some women notice bleeding between periods or after sexual intercourse, while others have heavier or longer menstrual cycles.
Fever, chills, and fatigue
If the infection is more severe, you may have a fever, chills, nausea, fatigue, or generally feeling unwell. These are signs that the infection is spreading and needs urgent medical attention.
Don’t ignore abdominal pain, unusual discharges, or irregular bleeding.Schedule an appointment today with obstetrician & gynaecologist (O&G) specialists at Thomson Medical to get a diagnosis and treatment. Early care can help protect your fertility, ease your pain, and safeguard your long-term health.
Our specialists who can treat PID
Loading...
When you should see a doctor
PID sometimes starts quietly, but it can get worse quickly and cause long-term issues such as chronic pelvic pain, infertility, ectopic pregnancy, and abscesses in the pelvic region. If you notice any of the following warning signs, you should go to the doctor right away.
Severe pelvic or abdominal pain:
Strong, persistent pain in the lower abdomen or pelvis may mean that the infection has spread deeper into the reproductive organs or caused complications.
High fever with chills:
A fever, especially if it comes with chills or sweats, is a sign that your body is fighting an infection and needs antibiotics.
Ongoing nausea or vomiting:
It can signal that the infection is affecting your overall health and may put you at risk of dehydration.
Abnormal, heavy, or smelly discharge:
Vaginal discharge that changes in colour, amount, or smell is a strong sign of infection.
It's always better to see a doctor if you're not sure about your symptoms. Even mild or vague pain can be cause for concern, especially if you are more likely to get STIs.
PID diagnosis
There isn’t a single test that can confirm PID. Instead, your doctor diagnoses it based on your symptoms, medical history, and gynaecological examination.
Initial assessment
Your doctor will ask about your medical background, sexual health history, and the symptoms you’ve been experiencing. This helps identify possible risk factors and guide the next steps.
Pelvic examination
A pelvic exam is usually performed to check for pain in your reproductive organs and to look for abnormal vaginal discharge. You may feel some pain during this exam, especially if you have PID.
Swab tests
Your doctor often takes swabs from your vagina and cervix to look for bacterial infections like Chlamydia trachomatis, Mycoplasma genitalium, or Neisseria gonorrhoeae. A positive test result supports the diagnosis of PID, but it’s important to remember that many women with PID may still have negative swab results.
Additional investigations
Because PID can be difficult to confirm, further tests may be required to either strengthen the diagnosis or rule out other causes of pelvic pain and infection. These could be:
Urine or blood tests to check for infection.
Pregnancy test to rule out pregnancy-related causes of symptoms.
Transvaginal ultrasound to provide a clear view of the uterus, ovaries, and fallopian tubes.
How PID is treated

The main goal of treating PID is to clear the infection as quickly as possible, ease the symptoms, and prevent long-term complications. Most of the time, treatment is usually straightforward, but it needs to start as soon as possible.
Medications
Your doctor may prescribe a combination of antibiotics to cover the wide range of bacteria that can cause PID, including STIs and other vaginal bacteria.
If your infectious condition is mild or moderate, you may have oral medications.However, if the condition is more severe, your doctor may suggest antibiotics through an IV. Even if your symptoms get better in a few days, you should still finish the whole course of antibiotics to make sure the infection is gone for good.
You might also be told to take pain relievers to help with pelvic pain or fever along with antibiotics.
Do I need to be admitted to the hospital?
Most women with PID can be treated at home, but you may need to be admitted if:
The infection is severe
You are pregnant
You have an abscess in the fallopian tubes or ovaries
Your symptoms don’t get better with the first oral treatment
While you're in the hospital, you might get antibiotics through an IV, pain relief, and close monitoring until your condition gets better.
Treatment of sexual partners
STIs are a common cause of PID, so it's important that your sexual partner get tested and treated as well. There is a high risk of reinfection if your partners don't get treated.
What to avoid during treatment
Your doctor may tell you to avoidsexual intercourse until the full course of antibiotics has been completed, and you and your partner are confirmed clear of infection. This prevents reinfection and gives your body the best chance to heal.
Early treatment with the right antibiotics not only relieves pain but also protects your fertility and long-term health.Schedule an appointment with Thomson Women's Clinic today to receive a personalised treatment plan.
Preventing PID
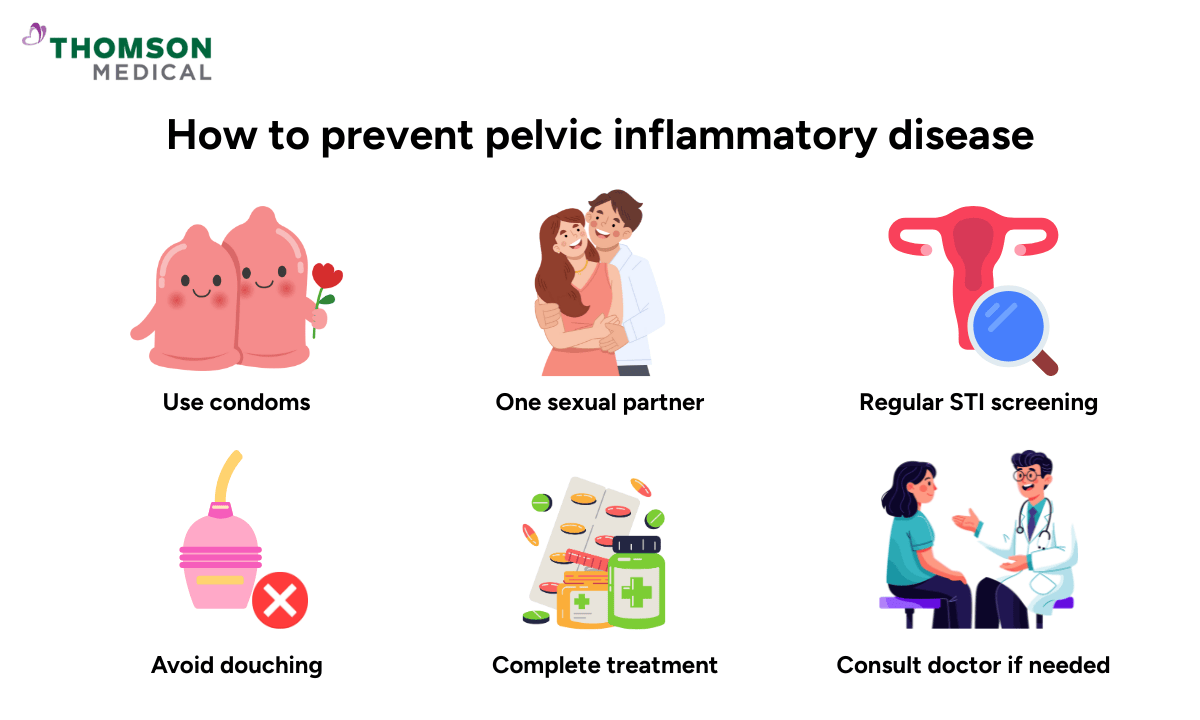
You can avoid PID by taking simple, regular steps that mostly focus on keeping your vagina healthy and lowering your risk of getting an infection.
Practice safe sexual activities
Condoms stop bacteria from moving from one partner to another by creating a barrier. One of the best ways to lower the risk of STIs that can lead to PID is to always use condoms during intercourse.
Limit the number of sexual partners
The safest kind of relationship is one where both partners are tested and free of infection and are only with each other.
Get regular STI screening
A lot of STIs that cause PID don't show any symptoms, so you could be infected without knowing. Regular STI testing can help find infections early and treat them before they get worse, especially if you are under 25, sexually active, or have a new partner.
Avoid douching
Douching throws off the natural balance of healthy bacteria in the vagina, which makes it easier for harmful bacteria to move up into the reproductive tract. The vagina cleans itself, so all you need to do is wash the outside with mild soap and water.
Complete the full course of antibiotics
If you have an STI, you should always take the full course of treatment, even if your symptoms get better. If you stop too soon, bacteria may stay, which raises the risk of PID and reinfection.
If you have abnormal symptoms, see a doctor
Don't ignore warning signs like pelvic pain, abnormal discharge, or pain during sexual intercourse. Early assessment and treatment lower the risk of severe health issues.
FAQ
How long does it take for PID to show up?
Some women may not notice any symptoms until complications happen, but symptoms can show up a few days to weeks after infection.
Is it possible to get PID without having an STD?
Yes. Although STIs are the most common cause of PID, it can also happen because of normal vaginal bacteria, giving birth, experincing a miscarriage, having a termination of pregnancy, or undergoing a medical procedure.
What naturally kills PID?
There is no proven natural cure for PID. Antibiotics are necessary to get rid of the infection. Natural remedies may help with overall health but should not replace medical treatment.
Is PID contagious?
No, PID itself is not contagious. However, the germs like chlamydia or gonorrhoea that cause PID can be sexually transmitted.
If I had PID, when can I continue having intercourse?
You should only have sexual activity again after your treatment is over, your symptoms are gone, and your doctor says the infection is gone. To avoid getting the disease again, your partner should also be checked.
What happens if PID is not treated?
If PID is not treated, it can cause severe and long-lasting complications, such as:
- Chronic pelvic pain
- Scarring and adhesions in the fallopian tubes
- Infertility
- Ectopic pregnancy (a pregnancy outside the uterus, often in the fallopian tube)
- Abscesses in the pelvic region
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
