An intimate moment with your loved one should bring you closer together. However, if you experience a burning sensation when urinating or feel the constant need to urinate within a day or two of having sexual intercourse, intimacy may no longer feel the same.
If these symptoms describe what you're experiencing, it's likely that you are dealing with a urinary tract infection (UTI) caused by sexual intercourse. While these infections undoubtedly cause frustration, they are preventable and treatable, so you can continue to enjoy intimacy without worry.
What is a UTI?
A urinary tract infection (UTI) occurs when bacteria enter your urinary tract (also known as the urinary system) and cause an infection. The most common cause of UTI is Escherichia coli (E. coli), a bacterium that normally lives in your digestive system.
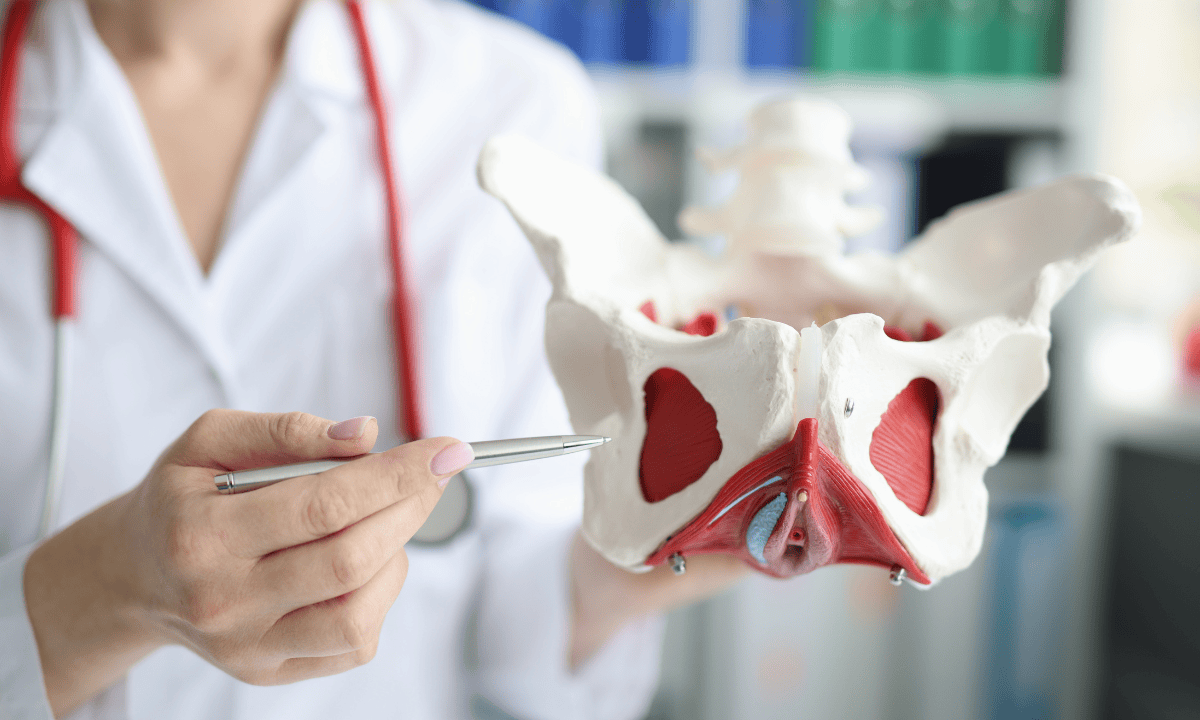
Your urinary tract is responsible for filtering waste and excess fluid from your blood and removing it from your body as urine. It consists of:
Two kidneys, the organs that filter waste from your blood
Two ureters, the thin tubes that carry urine from your kidneys to the bladder
A bladder, the hollow organ that stores urine
A urethra, the tube that carries the urine out of your body
Most infections affect the lower urinary tract (the bladder and urethra). If left untreated, the infection can travel upwards to the kidneys, which can lead to complications.
Why does sexual intercourse increase your risk of getting a urinary tract infection (UTI)?
The reason is that, during both penetrative and oral intercourse, bacteria can be introduced to the urethra. During penetrative intercourse, the motion can push bacteria from the areas near the vagina and rectum closer to the urethra. Meanwhile, during oral intercourse, bacteria from the mouth can enter the genitals and reach the urethra.
For this reason, UTIs after sex (also known as postcoital UTIs) are one of the most common health issues associated with sexual activity.
Although both men and women can contract UTIs from intercourse, women are more likely to develop this condition. This is because the female urethra is shorter than the male urethra (approximately 4 cm compared to 20 cm), meaning bacteria have less distance to travel to reach the bladder. The urethra is also closer to the vaginal and anal openings in women, making it easier for bacteria to enter during oral or penetrative intercourse.
Risk factors
While post-coital UTIs can affect any sexually active individual, there are factors that can increase your risk of developing this condition, including:
Having a history of recurrent UTIs.
Engaging in frequent sexual activity.
Having diabetes or a weakened immune system.
Being postmenopausal, as declining oestrogen levels reduce protective vaginal bacteria.
Using certain types of contraception, such as spermicides or diaphragms, that can disrupt the natural balance of vaginal bacteria.
Not urinating after sexual intercourse, which allows bacteria that have entered the urethra to cause an infection.
Experiencing vaginal dryness, which can cause friction during intercourse and lead to small tears, increases the likelihood of contracting an infection.
Common symptoms of UTI after sex
UTI symptoms usually show up within 12 to 48 hours of having sexual intercourse. The most common and characteristic sign of a UTI is dysuria, which causes a burning feeling when you urinate. Other common symptoms include:
Frequent urge to urinate, even if only a small amount of urine is passed
Cloudy, strong-smelling, or bloody urine
Pelvic discomfort or pressure in the lower abdomen
Rectal pain (in men)
When should you see a doctor?
Although UTIs after sex usually only infect the lower urinary system, if left untreated, they can travel to the kidney and cause a kidney infection (pyelonephritis). Since this is a serious condition, you should see a doctor if you experience any of the following symptoms:
Nausea
Vomiting
Fever and chills
Pain in your lower back or side
During your appointment, your doctor will typically diagnose a UTI through a simple urine test and prescribe antibiotics (usually for 3 to 7 days). Most people experience significant relief within 1 to 2 days of starting treatment. Pain relief medication may also be recommended to help reduce discomfort.
If your symptoms don't improve within 1 to 2 days or you frequently get UTIs after intercourse, don't hesitate to consult a specialist. At Thomson Women's Clinic, our specialist can help assess your symptoms and provide a personalised treatment plan. Schedule an appointment today.
Our sexual health specialists
Loading...
How do you know if you have a UTI after sex or something else?
Due to the similarity of their symptoms, UTIs can be mistaken for a sexually transmitted infection (STI) or a vaginal infection. The only way to be certain is to get tested for these conditions through a urine test or swab. However, there are differences between them:
UTI symptoms:
Frequent urination
Burning sensation during urination
Bladder pain or pelvic discomfort
Cloudy, strong-smelling, or bloody urine
Usually not accompanied with unusual vaginal discharge
STI symptoms:
Pain during intercourse
Genital itching, sores, or blisters
Sometimes accompanied by fever
May cause urinary discomfort similar to a UTI
Unusual discharge from the vagina or penis
Vaginal infection symptoms (vaginal yeast infection or bacterial vaginosis):
Itching and irritation in the vaginal area
Abnormal discharge with unusual odour
Usually no burning urination unless vaginal tissue is severely inflamed
A UTI is not a sexually transmitted infection. While they can happen after sexual intercourse, you can't pass them to your partner or vice versa. UTIs occur when bacteria, usually E. coli from your body, enter the urethra from the surrounding genital and anal areas.
STIs, on the other hand, are transmitted when someone has an infection and passes bacteria, viruses, parasites, or fungi that cause it through sexual contact.
Can UTIs after sex be prevented?

Yes. Because sexual activity can introduce bacteria to the urinary tract, prevention strategies focus on reducing bacterial transmission and eliminating any that may enter. These include:
Urinate before and after sex to flush out bacteria that may have entered the urethra.
Stay well-hydrated throughout the day to help dilute urine and encourage frequent urination, which naturally flushes bacteria from your urinary tract.
Use water-based lubricant if you experience vaginal dryness during sex, as this prevents friction and irritation that can create tiny injuries near the urethra.
Wash your genital area with warm water and a gentle, unscented cleanser before and after sexual intercourse.
Avoid harsh feminine products, douches, and scented soaps, as these can disrupt your natural bacterial balance.
Choose cotton underwear, which is more breathable and absorbs moisture, helping to reduce bacterial growth.
If you are at risk of UTIs, it is best to avoid spermicides and diaphragms, as these can remove the healthy bacteria that help keep germs that cause infections in check.
Consider cranberry supplements or juice, which contain compounds called proanthocyanidins that may prevent bacteria from adhering to the bladder walls.
If you are postmenopausal, a decrease in oestrogen can increase your risk of developing a UTI. In this case, you could consider vaginal oestrogen therapy to help restore protective vaginal bacteria.
If you experience recurrent UTIs after sex despite following prevention strategies, speak to your doctor about taking prophylactic antibiotics, which are low-dose antibiotics taken after intercourse. This option should only be used under medical guidance, however, to avoid contributing to antibiotic resistance.
If you're experiencing frequent UTIs after sexual intercourse despite trying various prevention strategies, it's recommended that you consult a specialist. At Thomson Women's Clinic, our specialists will work with you to identify the cause of your UTIs so you can enjoy intimacy worry-free. Schedule an appointment today.
FAQ
Why does having intercourse increase your risk of getting a UTI?
During sexual activity, the thrusting motion can push bacteria from the genital and anal areas into the urethra. Women are particularly susceptible because their urethra is shorter than men's, meaning bacteria can reach the bladder more easily.
The female urethra is also located closer to the anus, which makes it easier for bacteria such as E. coli to enter the urinary tract.
Can you get a UTI from oral intercourse?
Yes. Although it is less common than with penetration, bacteria can still be introduced into the urethra from the mouth during oral intercourse, which can lead to a UTI. Good oral hygiene and urinating afterwards can help reduce this risk.
Is it safe to have sexual activity with a UTI?
While it is possible, having intercourse with a UTI is not recommended until the infection has cleared. Having sexual intercourse during a UTI can worsen the symptoms, cause additional discomfort, and potentially push more bacteria into the urethra, which can delay recovery.
For your comfort, it's best to wait until you have completed your treatment and your symptoms have cleared up.
What can you do to reduce your risk of a UTI after sex?
There are several methods that can help prevent UTIs after sexual intercourse:
- Urinate before and after sexual intercourse to flush out bacteria
- Stay well hydrated throughout the day
- Use a water-based lubricant if you experience vaginal dryness
- Avoid spermicides and diaphragms if you're prone to UTIs
- Wash your genital area with warm water before intercourse
- Choose breathable cotton underwear
If you continue to experience frequent UTIs after sex despite taking these precautions, consult your doctor about preventive options.
How can I tell whether urinary symptoms after sex are caused by a UTI or an STI?
UTIs typically cause painful urination and the need to urinate frequently without any unusual vaginal or penile discharge. STIs, on the other hand, may cause unusual discharge, genital sores or blisters, and pain during intercourse, as well as urinary discomfort.
It's important to understand that a UTI is not an STI. While UTIs can occur after intercourse, they are caused by bacteria entering your urinary tract rather than being transmitted from your partner. If you're unsure about your symptoms, consult your doctor for proper testing and diagnosis.
What pill do you take after sexual intercourse to prevent UTI?
If you frequently experience UTIs after sex, doctors may prescribe prophylactic (preventive) antibiotics, which you take as a single dose immediately after sexual intercourse. This approach, known as postcoital prophylaxis, has been shown to reduce the recurrence of UTIs in sexually active women.
However, you should only take these medications under medical supervision, as your doctor will determine the most appropriate antibiotic for you based on your medical history and any previous urine cultures. Long-term use requires monitoring to prevent antibiotic resistance.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your medical condition, schedule an appointment at Thomson Women’s Clinic.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
