If you’ve noticed that intimacy has become uncomfortable or that your vaginal area feels tight, itchy, or irritated, you’re not alone.
Many women experience vaginal dryness at some point in their lives, while others may notice irritation or itching. However, these issues often go unspoken despite causing discomfort during everyday activities like walking or sitting. It can even make sexual intercourse feel painful or less enjoyable.
The good news is that this condition is treatable. Knowing what causes vaginal dryness, how it’s diagnosed, and the treatment options available can help women take charge of their health.
What is vaginal dryness?
Vaginal dryness occurs when the tissues of the vagina do not produce enough natural moisture. Sometimes, this dryness can even make simple activities such as walking, exercising, or wearing tight clothing uncomfortable.
Normally, the vaginal walls stay lubricated due to oestrogen (a female hormone) and natural vaginal secretions that keep the tissue soft and healthy. When oestrogen levels drop and secretions decrease, the vagina can feel dry, tight, or sore.
What are the symptoms of vaginal dryness?
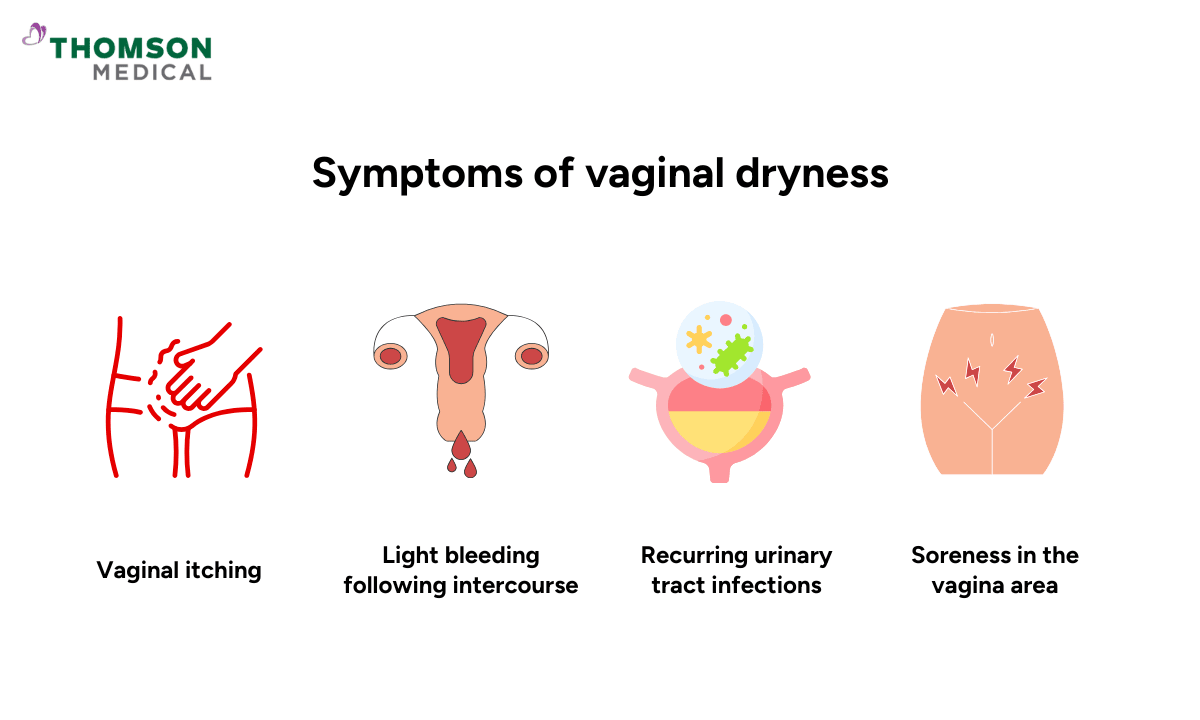
Vaginal dryness can cause significant discomfort in the vaginal and pelvic region. Beyond the physical sensation of dryness itself, this condition can lead to several other symptoms including:
Vaginal itching or stinging sensations
Pain during sexual intimacy or intercourse
Light bleeding after intercourse due to fragile vaginal tissue
Soreness or tenderness in the vagina area
Recurring urinary tract infections (UTIs) that don't resolve or keep coming back
Many women feel embarrassed about vaginal dryness, which can prevent them from discussing their symptoms with a health care provider or partner.
What are the causes of vaginal dryness?
Vaginal dryness has several possible causes. Some are hormonal, while others are linked to lifestyle, medication, or underlying health conditions.
Hormonal changes
Menopause is the most common cause. During menopause, oestrogen levels decrease, reducing the natural vaginal lubrication.
After childbirth and while breastfeeding, oestrogen levels temporarily dip, which can cause temporary dryness.
Certain contraceptives or medications such as birth control pills and hormonal intrauterine devices (IUDs) can affect vaginal moisture due to their hormonal influence.
Medical treatments and conditions:
Cancer treatments such as radiotherapy or chemotherapy in the pelvic area can damage the vaginal lining and vaginal tissue.
Sjögren's syndrome (an autoimmune disorder where the body attacks moisture-producing glands) can cause dryness throughout the body.
Antihistamines and decongestants (often used for colds or allergies) can reduce moisture throughout the body including the vagina.
Antidepressants and anti-anxiety medicines known to cause sexual side effects, including vaginal dryness.
- Smoking can reduce blood circulation and oestrogen levels.
- Stress can lower arousal and natural lubrication.
- Lack of sexual intimacy which decreases vaginal elasticity.
- Not drinking enough water can affect overall hydration, including vaginal moisture.
Lifestyle and psychological factors:
Smoking can reduce blood circulation and oestrogen levels.
Stress can lower arousal and natural lubrication.
Lack of sexual intimacy which decreases vaginal elasticity.
Not drinking enough water can affect overall hydration, including vaginal moisture.
Irritants and hygiene products:
Using harsh soaps or perfumed products can disturb the natural pH balance and vaginal microbiome, and lead to irritation and dryness.
If you’re unsure what’s causing your vaginal dryness, request an appointment with Thomson Medical for a confidential and professional assessment. Our women’s health specialists will help identify the underlying cause and recommend personalised treatments tailored to your needs.
How is vaginal dryness diagnosed?
Diagnosing vaginal dryness usually involves:
Medical history and symptom discussion:
Your doctor will ask about your symptoms, such as dryness, itching, or discomfort during intercourse.
They will also review your medical history, including menopause status, childbirth, breastfeeding, and current medications.
Pelvic examination:
This examination is performed to check for signs such as pale, thin vaginal tissue, loss of elasticity, or irritation.
This allows your doctor to assess the health of your vaginal tissues directly.
Laboratory tests (if needed):
Your doctor may take a small sample of vaginal fluid for laboratory tests to check oestrogen levels or rule out infections.
Diagnosis is usually straightforward, and identifying the underlying cause helps determine the most effective treatment for your situation.
Our specialist
Loading...
How is vaginal dryness treated?
Treatment depends on the cause and severity of the dryness. The goal is to restore comfort and protect vaginal tissue health.
Lifestyle approaches
Drink enough water to support overall tissue moisture
Exercise regularly to improve blood flow to the pelvic region
Manage stress through relaxation techniques and meditation
Quit smoking to improve oestrogen balance and circulation
Eat a balanced diet including healthy fats (such as avocado and salmon) and foods rich in phytoestrogens (plant compounds that act like oestrogen that are found in soy, flaxseed, and chickpeas)
Engage in regular sexual activity to increase blood flow and help maintain vaginal elasticity
Wear cotton underwear to allow better air circulation and reduce irritation
Over-the-counter (OTC) relief
These products can ease discomfort and improve vaginal moisture without a prescription.
Product type | When to use | Duration | Is it safe? |
Water-based lubricant | During intercourse | Short-term | Safe but may dry quickly. Reapply when needed. |
Silicone-based lubricant | During intercourse | Long-lasting | Slippery and durable. Safe to use with condoms. |
Oil-based lubricant | During intercourse (not with condoms) | Long-lasting | Can damage latex condoms. Use pure oils such as coconut oil or mineral oil to lower the risk of infection. |
Vaginal moisturiser | 2-3 times per week | Long-term | Keeps the area moist and helps the vaginal tissues stay soft and flexible over time. |
Choose products that are fragrance-free and avoid those containing alcohol, glycerin, or harsh chemicals, as these can worsen vaginal dryness.
Prescription treatments
Topical oestrogen therapy:
Applied directly to the vagina as a cream, tablet, or ring, these treatments restore moisture and elasticity by replacing local oestrogen levels.
Systemic hormone therapy:
Used when menopausal symptoms (like hot flashes) are also present. Not suitable for everyone. Your doctor will discuss risks and benefits.
Ospemifene (Osphena):
An oral medication that mimics oestrogen’s effects on vaginal tissue. It’s approved for moderate to severe postmenopausal dryness or pain during intercourse.
Prasterone (Intrarosa):
A vaginal insert containing DHEA(a natural hormone) that converts into oestrogen and androgens locally to improve tissue health.
In many cases, simple lifestyle changes or non-prescription options can help. However, persistent or severe symptoms may require medical treatment.
How do you treat a dry vagina naturally?
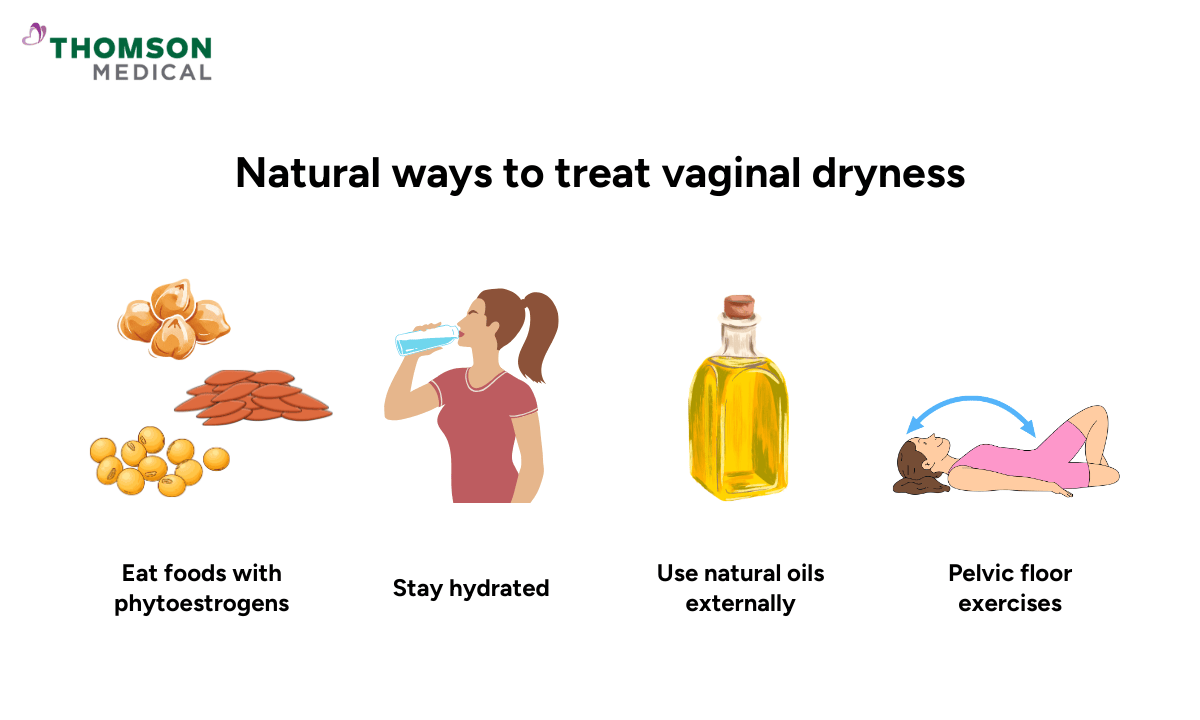
While medical treatments are often most effective, some natural steps can help support vaginal health:
Eat foods with phytoestrogens and healthy fat
Stay hydrated and eat water-rich foods such as cucumber, watermelon, and oranges
Use natural oils externally (like coconut or vitamin E oil) to relieve dryness and test a small area first to check for irritation
Pelvic floor exercises (Kegels) to strengthen muscles and improve blood flow regulation to the vagina
Taking time for intimacy and relaxation can help the body’s natural lubrication process
These natural remedies can help mild cases but do not replace medical evaluation if symptoms persist.
If vaginal dryness continues despite natural remedies, request an appointment with Thomson Medical to speak with our women’s health specialists for personalised care and treatment options.
When should you see a doctor?
It’s important to consult a doctor when vaginal dryness becomes persistent. You should see a doctor if:
Vaginal dryness continues despite using lubricants or moisturisers
Intercourse is painful or causes bleeding
There are symptoms of infection such as unusual vaginal discharge, odour, or itching
You have dryness linked to menopause or a medical condition like diabetes or autoimmune disease
Over-the-counter products don’t help after a few weeks
Persistent dryness can affect quality of life, so professional evaluation ensures proper treatment and peace of mind.
FAQ
Is vaginal dryness common?
Yes, vaginal dryness is common. It affects about 45% of postmenopausal women, but it can also occur at other stages of life due to hormonal or lifestyle factors.
What does a dry vagina feel like?
If you have vaginal dryness, you may feel tightness, itching, burning, or pain during sex. Some women also experience light spotting or tearing of the vaginal tissue.
What foods increase female lubrication?
Foods that can help support natural lubrication and vaginal health include those rich in plant oestrogens (such as soy, flaxseed, and sesame), omega-3 fatty acids (salmon, nuts, seeds), and vitamin C-rich fruits and vegetables. Staying well-hydrated by drinking plenty of water is also important.
What are the common symptoms of vaginal dryness?
If you have vaginal dryness, common symptoms you may experience include burning, itching, discomfort, pain during or after intercourse, urinary urgency, or frequent urinary tract infections.
Why is my vagina dry during sex?
Your vagina may be dry during sex due to several reasons, including hormonal imbalance, certain medications (such as antihistamines or antidepressants), stress, dehydration, or insufficient foreplay before penetration. Hormonal changes during menopause, breastfeeding, or from birth control can also reduce natural lubrication.
Should I avoid certain products if I have vaginal dryness?
Yes, if you have vaginal dryness, you should avoid scented soaps, bubble baths, douches, and petroleum jelly. These can disrupt natural pH balance and worsen irritation. Instead, use gentle, fragrance-free products and wash the external area with water only.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
References:
Lindahl, S. (2014). Reviewing the options for local estrogen treatment of vaginal atrophy. International Journal of Women S Health, 307. https://doi.org/10.2147/ijwh.s52555
Vanderschee, R., & Kostov, S. (2025). Approach to lubricant use for sexual activity. Canadian Family Physician, 71(7–8), e158–e166. https://doi.org/10.46747/cfp.710708e158
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
