Have you ever experienced pain or discomfort in the outer part of your genitals but found it difficult to pinpoint the cause? Sometimes, the pain comes and goes while other times, it persists and affects your daily life.
Even if you can't see anything wrong on the outside, what you're feeling is real and not just your imagination. If this sounds familiar, vulvodynia, a common chronic condition that affects women of all ages, could be the cause of your symptoms.
What is vulvodynia?
Vulvodynia is ongoing discomfort or vulvar pain (pain in the external female genital area) lasting at least three months without a clear cause. The pain may feel like burning, stinging, or soreness. Often, the vulva looks normal without any visible sign, making the condition difficult to spot or be mistaken for another vulvar condition.
What types of vulvodynia are there?
Doctors usually classify by where the pain occurs and whether something triggers it. There are two main types:
Localised vulvodynia:
Pain is focused in a specific area of the vulva, for example, the entrance to the vagina.
The pain usually starts when the area is touched or pressed. It can also happen during intercourse, when putting in a tampon, or after sitting for a long time.
Generalised vulvodynia:
Pain occurs across a wider area of the vulva.
The pain may be provoked (triggered by touch, intercourse, or tampon use) or unprovoked (occurring without contact).
How can vulvodynia affect your life?
Living with vulvodynia can be uncomfortable affect your daily life in many ways. Simple activities like sitting for too long, exercising, or wearing tight clothes can lead to pain. Additionally, sexual activity may also become painful, which can lead you to avoid it, and may negatively affect your relationship.
You may also feel sad, worried, or isolated, particularly because the source of your pain is not immediately visible. This can lead to you being misunderstood or dismissed.
The good news is, with proper care, many women start to feel better. If the pain is preventing you from living normally or causing stress in your relationship, it’s recommended that you see a doctor.
What are the symptoms of vulvodynia?
The symptoms of vulvodynia can differ from woman to woman, ranging from mild irritation to severe pain that can make daily life difficult. However, there are a few common symptoms. Which include:
Pain or discomfort in the vulva without an obvious cause that last for at least three months
Feel like burning, stinging, throbbing,or itching
Pain that worsen during sexual intercourse or tampon use, or may be present without any contact
Our women's health specialist
Loading...
What causes vulvodynia?
There’s no single known cause. Doctors believe several factors may play a role:
Nerve injury or over-sensitive nerve endings in the vulva
Hormonal changes or issues with hormone receptors
Pelvic floor muscles get too tight suddenly (muscle spasms) or become weak
Chronic inflammation
Previous infections that might trigger changes to nerves or tissues
In rare cases, past sexual trauma may contribute to pelvic pain and muscle tension
Some women have very sensitive nerves in the vulva, making even light touch painful, while others develop it after an infection, injury, or surgery.
What conditions often happen with vulvodynia?
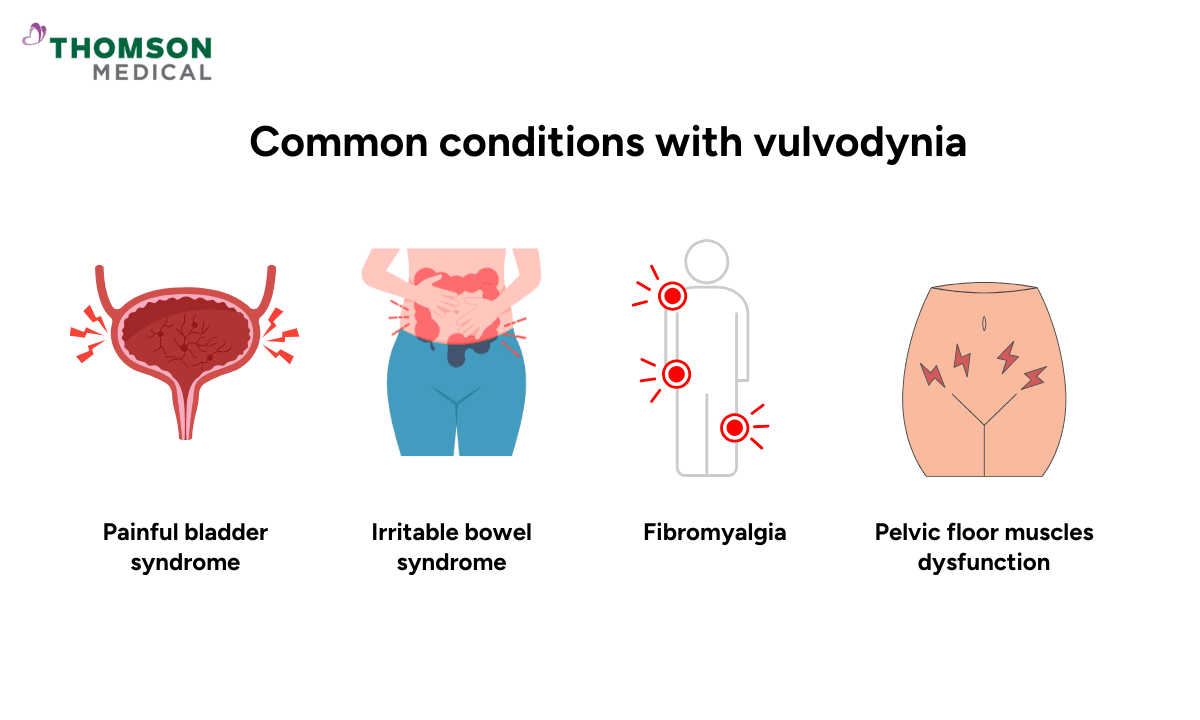
Vulvodynia may occur alongside other chronic pain or pelvic conditions such as:
Painful bladder syndrome (also called interstitial cystitis)
Irritable bowel syndrome
Fibromyalgia (long-term condition that causes widespread body pain and fatigue)
Pelvic floor muscles dysfunction, where the muscles around pelvis become weak
These overlapping conditions suggest that vulvodynia might be linked to other long-term pain condition in the body, not only the vulva. A doctor can help find out which conditions are linked and suggest the right treatment to ease the pain.
If you’ve been struggling with pain that hasn’t improved or you think it might be connected to other pelvic conditions, request an appointment with Thomson Medical. Our specialists can help identify the cause and provide a tailored treatment based on your medical condition.
How is vulvodynia diagnosed?
Diagnosis relies on careful assessment rather than a single test. The doctor will first ask about your symptoms and health history. The doctor will then gently examine the vulva during a pelvic exam. Sometimes, they may use a soft cotton swab to press on different spots to see which areas feel painful. This simple check is called the cotton swab test and helps the doctor understand where the pain is coming from.
Some tests may also be done to make sure it is not an infection or skin problem. Because the vulva often looks normal, the doctor depends on what you describe and where the pain happens to make the diagnosis.
Sometimes doctors may first check for other common problems, like yeast infections or sexually transmitted infections (STIs), before diagnosing vulvodynia. If no other cause is found and pain has lasted at least three months, then vulvodynia may be diagnosed.
How is vulvodynia treated?
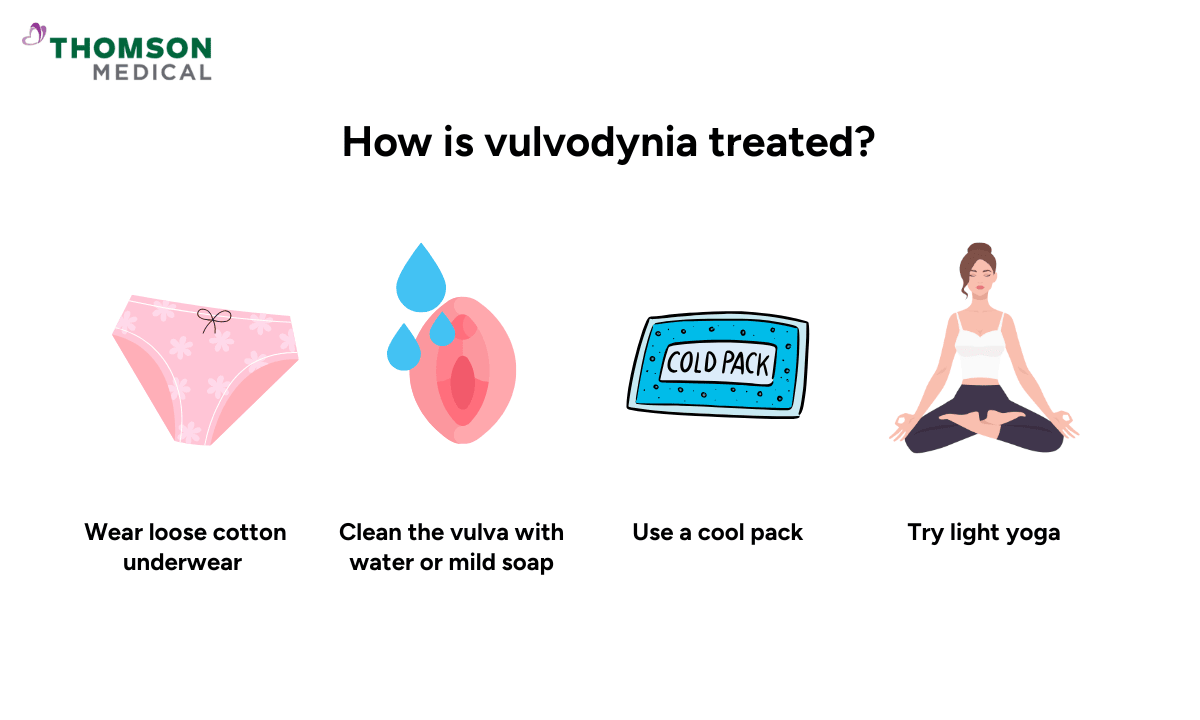
Treatment for vulvodynia often requires a combination of approaches tailored to your individual needs. The treatments include:
Medications:
May include local anaesthetics (numbing creams), nerve-pain medications, or antidepressants.
Physical therapy:
Targeting for pelvic floor muscle issues.
Injections:
Nerve blocks and injections are rarely the sole treatment for vulvodynia.
A muscle-relaxing injection (using botulinum toxin type A) may be given to ease tightness in the pelvic area.
Lifestyle and skincare changes:
Wearing loose, breathable cotton clothes and avoiding tight garments.
Wash the vulva area with plain water or mild soap.
Use lubricants during intercourse.
A cool pack or warm shallow bath may help soothe pain.
Cognitive behavioural therapy (CBT):
This helps you notice negative thoughts and respond in practical ways.
You may also be encouraged to keep a daily pain diary to track when symptoms appear and what seems to help.
Relaxation and self-care::
Deep breathing, gentle stretching, or light yoga.
Write down when the pain happens, what triggers it, and how strong it feels.
With patience and the right care, many women find relief and start to feel more comfortable again.
When should I see a doctor?
It’s normal to feel unsure about when to seek help, especially if the pain comes and goes. However, it’s always better to get checked early rather than wait for it to worsen. See a doctor if you have pain, burning, or irritation in the vulva that lasts for more than a few weeks. The doctor may do a physical exam to check the area and better understand the cause.
You should also get checked if the pain is affecting your mood, intimacy, or makes it hard to sit or do your daily activities comfortably. Early diagnosis helps avoid months or years of unexplained discomfort and gives you a better chance at relief.
If you’ve been dealing with persistent vulvar pain or irritation, don’t hesitate to consult a specialist. Request an appointment with Thomson Medical for a proper assessment and guidance toward effective relief.
FAQ
When will I notice the pain in my vulva?
The vulvar pain can start slowly or suddenly. Some women feel it during intercourse, when using a tampon, or during a doctor’s check-up. Others may feel burning or stinging even when they are not touching the area. The pain can come and go or stay for a long time.
What does vulvodynia feel like?
The pain may feel like burning, stinging, or soreness in the vulva. Some women feel sharp or shooting pain, while others feel a dull ache. The pain can be in one spot or all over the vulva. It may happen when touched, during intercourse, or even when sitting for a long time. Sometimes, it can happen for no clear reason at all.
Does vulvodynia ever go away?
Yes, it can get better with the right care. It may not go away on its own, but many women feel much better after treatment. Medicines, gentle exercises, pelvic floor therapy and lifestyle changes can help reduce pain. With early care and patience, most women can live more comfortably again.
Can I prevent vulvodynia?
Although there is no definitive way to prevent it, you can take care to protect the area. Use fragrance-free products, wear loose cotton underwear, and avoid tight clothes. Also, being gentle during intercourse and keeping the area clean and dry can help reduce irritation.
Is vulvodynia common?
Yes, it is quite common, but many women do not know about it. Some think it is just an infection or normal irritation. Because of this, many do not talk about it or get help right away. Knowing more and seeing a doctor early can make a big difference.
Can vulvodynia affect intimacy or relationships?
Yes, it can. Pain during intercourse may cause worry or make a woman avoid intimacy. This can affect closeness with a partner. Talking openly with your partner, joining support groups and getting advice from a doctor or counsellor can be helpful. With the right treatment and support, many women still enjoy happy and close relationships.
If you’re experiencing ongoing vulvar pain, burning, or discomfort, it’s important to get checked rather than self-treating. Request an appointment with Thomson Medical to discuss your symptoms and, if needed, undergo an STI screening. Our specialists provide confidential consultation, clear explanations of your results, and clear guidance to help you manage your sexual and reproductive health.
Reference:
Torres-Cueco, R., & Nohales-Alfonso, F. (2021). Vulvodynia—It Is Time to Accept a New Understanding from a Neurobiological Perspective. International Journal of Environmental Research and Public Health, 18(12), 6639. https://doi.org/10.3390/ijerph18126639
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
