Many women start to think about ovarian cancer as they move into new stages of life. You might find yourself wondering whether your age puts you at higher risk or whether certain symptoms should be taken more seriously.
Ovarian cancer is most commonly diagnosed after menopause, with most cases occurring in women over the age of 50. That said, age is only one part of the picture. Understanding how risk changes over time, which types of ovarian cancer are seen at different ages, and when it is worth speaking with your doctor can help you stay informed without unnecessary worry.
At what age does ovarian cancer most often occur?
Ovarian cancer most commonly affects women after menopause, with rates peaking between ages 55 and 64. About half of all cases are found in women aged 63 or older.
This means if you're in your 60s or beyond, staying alert to symptoms and maintaining regular checkups becomes particularly valuable. At the same time, most women in this age group will never develop ovarian cancer.
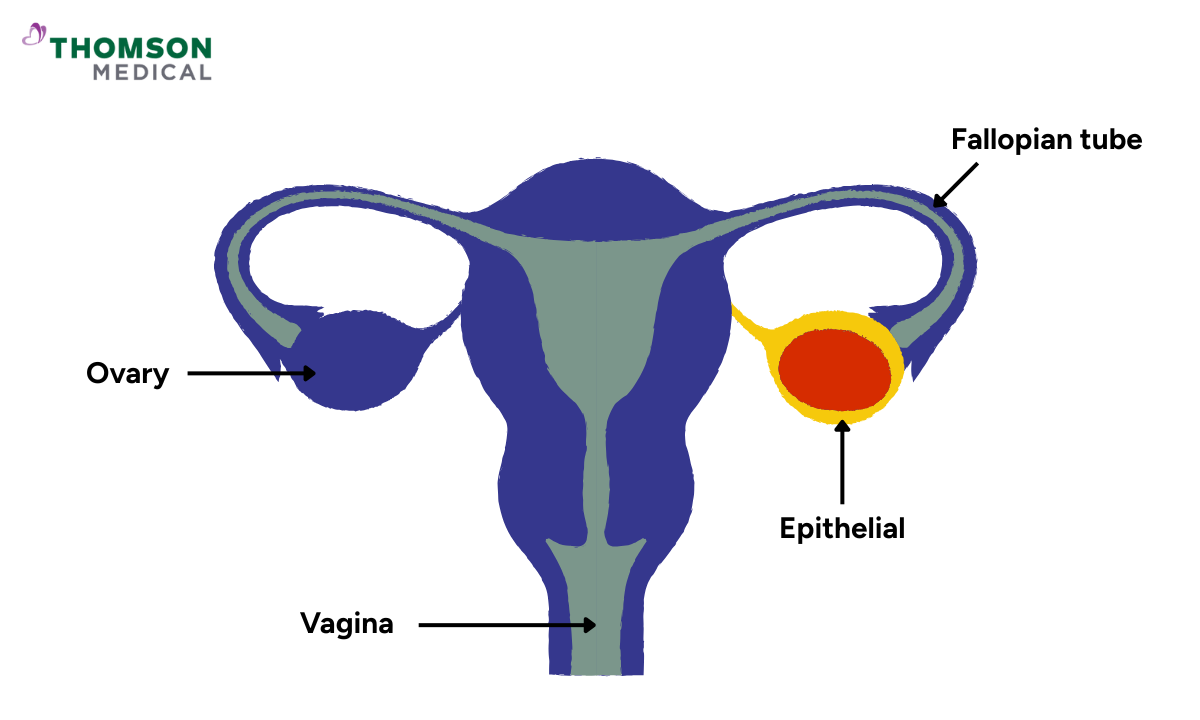
The most common form is epithelial ovarian cancer, which accounts for about 90% of cases. This type:
Develops in the outer layer of the ovary and fallopian tubes
Primarily occurs in women after menopause
It is most often diagnosed between ages 60 and 65
Women under 30 account for less than 1% of cases, while those under 40 represent 10 to 15% of all diagnoses. These numbers show that ovarian cancer is less common in younger women. However, if you're under 40 and experiencing ongoing symptoms, they're still worth discussing with your doctor since early diagnosis improves treatment success.
Can younger women get ovarian cancer?
Ovarian cancer is more common in older women, but younger women in their 20s and 30s can get it too.
The types of ovarian cancer that affect younger women are different from those in older women – fortunately, the treatment usually works better for younger women who get ovarian cancer.
Germ cell tumours
These develop from the cells that become eggs and mainly affect women between 10 and 30, making up 70% of ovarian tumours in this age group. They usually affect just one ovary, and treatment works well even when the tumour has spread.
Sex cord stromal tumours
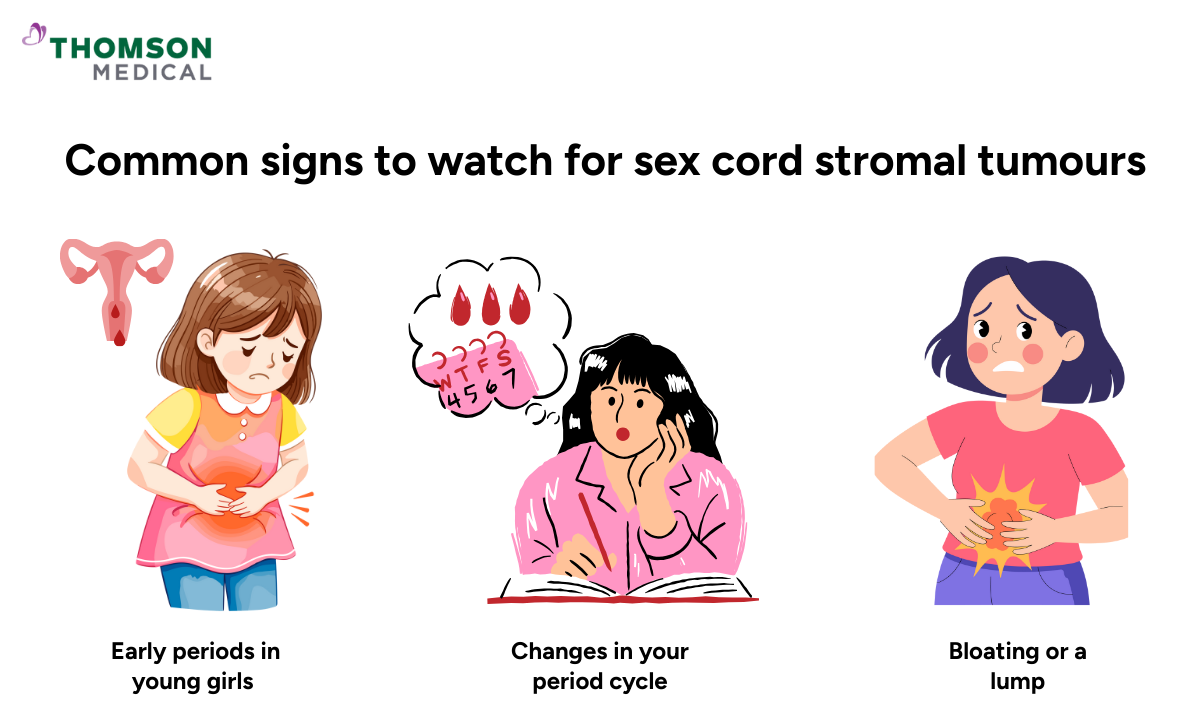
Sex cord stromal tumours, also called stromal ovarian cancer, are rare and grow in the tissue that supports your ovary. They often appear in women under 30.
Because they produce hormones, you might notice:
Excess body hair
Early periods in young girls
Changes in your period cycle
Bloating or a lump
If you're a younger woman experiencing similar symptoms, don't dismiss them just because ovarian cancer is rare in your age group. These specific tumour types can have distinct symptoms, and acting on persistent warning signs typically leads to better outcomes.
These different types help explain why age is such an important factor. The cancer you might develop changes as you get older, which is why doctors consider your age when assessing risk.
Ovarian cancer specialist
Loading...
What other factors affect your risk?
While age is the strongest predictor of ovarian cancer, it doesn't work alone. Several other factors can raise or lower your overall risk, and knowing them can help you see your personal health picture more clearly.
Family history and genetics
If your mother, sister, or daughter had ovarian cancer before age 50, your risk increases three to four times.
Certain inherited gene mutations also significantly raise your risk:
BRCA genes (BRCA1 and BRCA2 mutations)
Lynch syndrome (caused by mutations in DNA repair genes)
PTEN gene mutation
These genetic changes are also linked to breast, endometrial, and colorectal cancers. This means genetic testing can help you understand your risk for multiple types of cancer at once and help your doctor create a screening plan tailored to your specific genetic profile.
Lifestyle and reproductive factors
These are risk factors, not certainties. Many women with one or more of these factors never develop cancer.
Several aspects of your health and life choices can affect your risk:
Not having children:
Women who've never given birth have a 24% higher risk compared to those who've had one child.
Hormone replacement therapy:
Using HRT, especially for 10 years or longer, increases your risk for certain types of ovarian cancer.
Smoking:
Cigarette smoking raises your risk by about 31%, particularly for certain cancer types.
Endometriosis:
This condition increases your risk more than four times, especially for specific types of ovarian cancer.
Weight after menopause:
Excess weight in postmenopausal women leads to higher oestrogen levels, which can promote cell growth in the ovaries.
Remember, these are simply factors that influence probability, not guarantees. Many women with these risk factors never develop cancer. Knowing your personal risk profile helps you and your doctor create a monitoring plan that's right for you.
Understanding how genetic conditions and lifestyle factors shape your risk gives you more control over your health. Request an appointment at Thomson Medical to review your family history, discuss family history or testing, and create a personalised plan for monitoring and prevention based on your individual risk profile.
Why does age increase ovarian cancer risk?
You might be wondering what actually makes ovarian cancer more likely as you age. Getting older brings natural changes that can increase vulnerability to cancer.
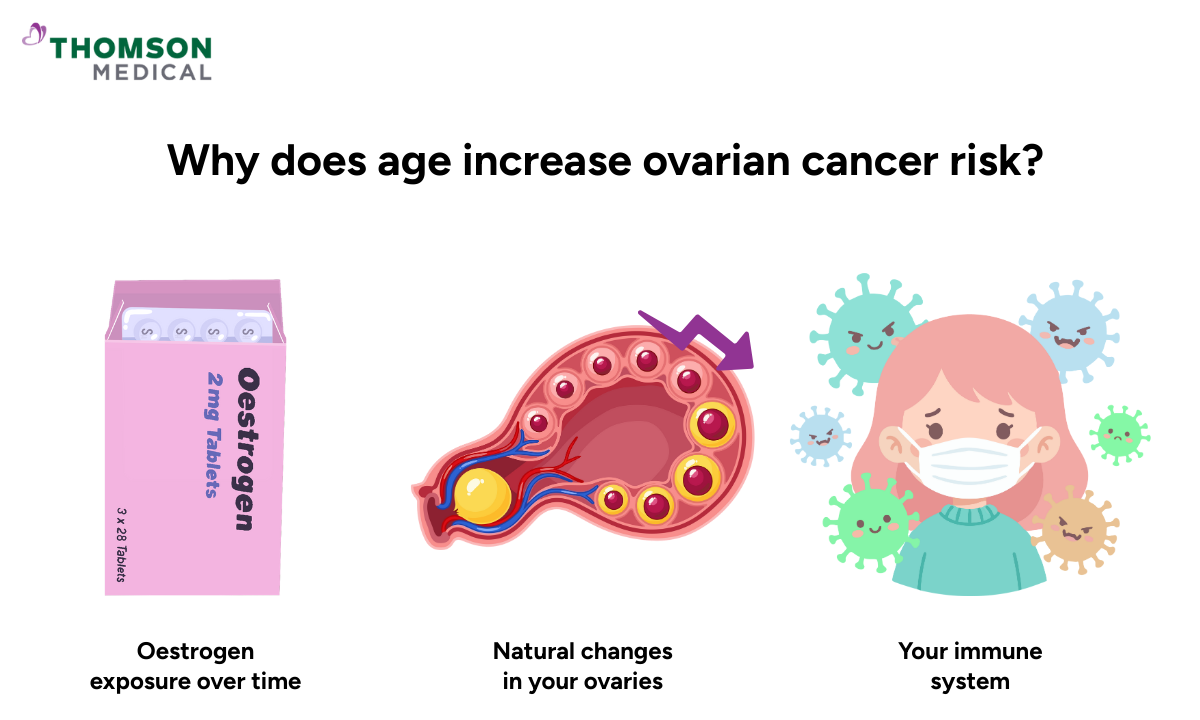
Oestrogen exposure over time
Your ovaries are exposed to oestrogen throughout your reproductive years. This prolonged exposure can damage cells and make them more vulnerable to cancer.
Factors such as when you started your period or went through menopause weren't in your control. Your risk tends to be higher if you started periods before 14, went through menopause after 50, or take hormone replacement therapy.
Understanding these factors simply helps your doctor assess your overall risk and recommend appropriate monitoring. It doesn't mean you will develop cancer.
Natural changes in your ovaries
As you age, your ovaries go through natural changes. When your egg supply gradually decreases, it triggers shifts in your hormone levels.
These shifts can create conditions in your ovaries where abnormal cells are more likely to develop. This is one reason the contraceptive pill may offer protective benefits. By regulating ovulation, it gives your ovaries a break from continuous hormonal cycling.
Your immune system
As you get older, your immune system doesn't work quite as sharply as it once did. It becomes less effective at spotting and fighting cancerous cells. This means damaged cells have a better chance of growing into cancer instead of being caught and cleared away by your body's defences.
This is why regular screenings and paying attention to ongoing symptoms become important as you age. Finding problems while they're still in their earliest stages offers better treatment options.
These changes are a normal part of ageing, and having them doesn't mean you'll definitely develop cancer. They simply help explain why risk increases over time and why staying aware of your body becomes increasingly important.
When should you talk to your doctor?
Your health deserves attention, and asking questions or sharing concerns with your doctor is always the right choice. You don't need to feel embarrassed or worry about wasting their time.
Get checked if you notice any of these symptoms and they've lasted more than two weeks:
Abdominal or pelvic pain
Bloating that doesn't go away
Changes in how often you need to urinate or have bowel movements
Loss of appetite
Feeling constantly tired
Your doctor may conduct a pelvic examination to check for any unusual lumps or swelling and order a blood test to measure protein levels that may indicate cancer.
If you have a family history of ovarian or breast cancer, talk to your doctor about appropriate screening options, which may include genetic counselling or specific tests based on your risk level.
These symptoms can be caused by many different things, most of which aren't cancer at all. But persistent symptoms deserve a proper checkup to find out what's going on. Catching potential problems early almost always leads to better outcomes.
Understanding your outlook
Whether you're in your 20s or 70s, the most important step is staying informed about your body and seeking medical advice when something feels off. Early detection improves outcomes across all age groups.
Younger women often have better outcomes when diagnosed. Women aged 45 and under have nearly six times better long-term survival rates compared to women aged 85 and over.
This happens because cancer in younger women is often found at more treatable stages and responds better to treatment. But many older women can and do beat ovarian cancer.
What matters most is getting regular checkups and seeing your doctor when something doesn't feel right. Being proactive about your health, regardless of your age.
Early action can make a real difference to outcomes. Request an appointment at Thomson Medical to discuss your personal risk, review any symptoms you may be experiencing, and plan appropriate check-ups or tests. Getting clarity early helps you make informed decisions and access the right care at the right time.
FAQ
At what age does ovarian cancer usually occur?
Most cases happen after age 50, with diagnoses most common between ages 55 and 64. While ovarian cancer can develop at any age, it's uncommon in women under 40.
Can you get ovarian cancer in your 20s or 30s?
Yes, though it's rare. Younger women often develop germ cell tumours or sex cord stromal tumours rather than epithelial ovarian cancer, and these types usually respond well to treatment.
Does ovarian cancer risk increase with age?
Yes, your chances increase as you age, particularly after menopause, with the highest rates occurring in women between 55 and 64.
What type of ovarian cancer affects younger women?
Younger women usually develop germ cell tumours or sex cord stromal tumours. Older women are more likely to develop epithelial ovarian cancer, which is the most common type overall.
Are women over 60 at higher risk for ovarian cancer?
Yes. Your risk is higher after 60, and about half of all cases are found in women aged 63 or older. The risk continues to increase with age.
Does menopause increase ovarian cancer risk?
Menopause doesn't directly cause ovarian cancer. However, most cases occur after menopause simply because age is the primary risk factor. It's the natural ageing process, rather than menopause itself, that raises your risk.
What are the survival rates for ovarian cancer by age?
Survival rates are often better for younger women. Women aged 45 and under have nearly six times better long-term survival compared to those aged 85 and over. More than 70% of deaths occur in women aged 65 and older.
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
References:
Gayther, S. A., & Pharoah, P. D. (2010). The inherited genetics of ovarian and endometrial cancer. Current Opinion in Genetics & Development, 20(3), 231–238. https://doi.org/10.1016/j.gde.2010.03.001
Lalrinpuii, E., Bhageerathy, P. S., Sebastian, A., Jeyaseelan, L., VinothaThomas, Thomas, A., Chandy, R., & Peedicayil, A. (2017). Ovarian cancer in young women. Indian Journal of Surgical Oncology, 8(4), 540–547. https://doi.org/10.1007/s13193-017-0680-z
Smith, E. R., & Xu, X. (2008). Ovarian ageing, follicle depletion, and cancer: a hypothesis for the aetiology of epithelial ovarian cancer involving follicle depletion. The Lancet Oncology, 9(11), 1108–1111. https://doi.org/10.1016/s1470-2045(08)70281-x
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment