If you're preparing for intrauterine insemination (IUI), you've likely heard about post-wash sperm count – but what does this number actually mean for your chances of success? Is there a minimum count needed? What's considered "good"? And if your count is lower than expected, does IUI still make sense?
Knowing post-wash sperm count, the threshold numbers fertility specialists look for, and how other factors influence IUI success rates can help you set realistic expectations and make informed decisions about your fertility treatment path.
What is IUI?
IUI is a low-risk fertility treatment where sperm is placed directly into your uterus (womb) around the time you ovulate. The aim is to get healthy sperm closer to the fallopian tubes, which increases the chances of fertilisation happening naturally inside your body.
IUI works well for people with mild male factor infertility, ovulation problems, or unexplained infertility. It's also commonly used by individuals using donor sperm. Many people successfully conceive through IUI, and it might be the right option for you too.
What is sperm washing?
Before IUI can happen, the semen sample needs to be prepared through a process called sperm washing. This laboratory technique cleans the sample to remove several things that could interfere with pregnancy:
Non-motile sperm (sperm that don't swim properly)
White blood cells
Debris and seminal fluid that might cause cramping or allergic reactions
The washing process concentrates the healthiest and most active sperm into a smaller volume. Essentially, your doctor is selecting the strongest swimmers to give you the best possible chance of success.
What is post-wash sperm count?
Once the sperm washing is complete, your doctor will measure how many actively swimming sperm remain in the prepared sample. A post-wash sperm count tells you how many actively swimming sperm remain after the semen sample has been washed and concentrated. This is one of the key numbers that will help determine your path forward.
This number matters because only motile sperm (sperm that can swim effectively) can travel through the uterus, reach the egg, and fertilise it. The result is usually given as total motile sperm count (TMSC). This number reflects both the quantity and quality of the sperm that will be used in your IUI procedure.
What is a favourable post-wash sperm count for IUI?
Your post-wash sperm count directly affects your chances of success. Here's what the numbers mean:
Post-wash TMSC | IUI Success |
More than 10 million motile sperm | This is considered ideal and is associated with the highest IUI success rates. |
5-10 million motile sperm | You have reasonable pregnancy chances in this range, though success rates may be slightly lower than the ideal range. |
1-5 million motile sperm | The success rate is lower, but IUI may still work depending on other factors like your age, timing, and whether you're using fertility medications. |
Less than 1 million motile sperm | This means low success rates for IUI. At this level, your doctor may suggest other treatments like IVF (in vitro fertilisation), ICSI (intracytoplasmic sperm injection), or using donor sperm. |
These alternatives often have better success rates for lower sperm counts, so you still have effective options.
If your post-wash sperm count falls below the ideal range or you’re unsure how your numbers affect your IUI success, request an appointment with a Thomson Medical fertility specialist. Our doctors can review your semen analysis in detail and explain your chances based on TMSC and guide you toward the most suitable next step.
Our IUI specialists in Singapore
Loading...
What are the factors affecting IUI success beyond sperm count?
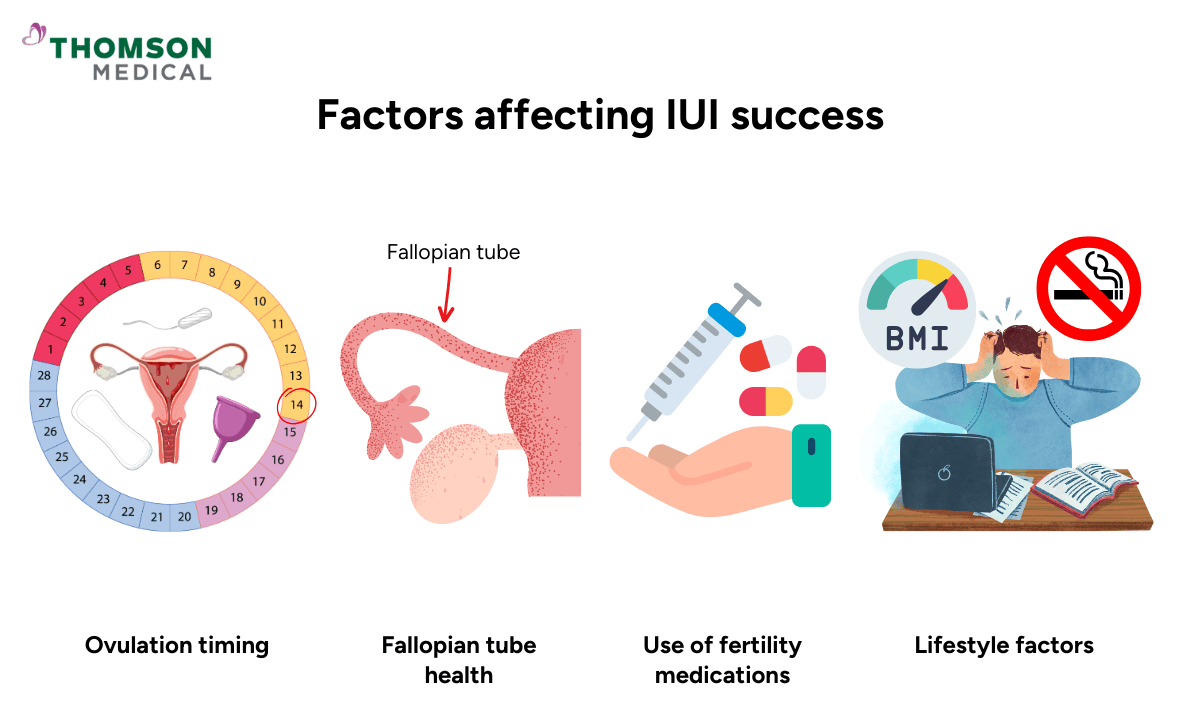
While sperm quality matters greatly, other factors play an equally important role in whether IUI works. Your fertility specialist will consider all of these when planning your treatment.
Age of the female partner:
Fertility naturally declines with age, particularly after 35. After 35, these rates gradually decrease to around 10% or less per cycle.
Ovulation timing:
The IUI must happen at exactly the right time, usually within 24 to 36 hours before ovulation.
Your doctor may use ultrasound monitoring or hCG trigger shots for IUI (a hormone injection that causes ovulation) through ovulation induction to ensure the timing is perfect.
Fallopian tube health:
At least one of your fallopian tubes must be open and working properly for IUI to succeed.
The sperm needs to travel through your fallopian tube to meet the egg. Blocked or damaged tubes will prevent pregnancy even with good sperm counts.
Uterine environment:
A healthy womb lining is important for a fertilised egg to implant successfully.
Your lining needs to be thick enough (usually at least 7–8 mm) and have the right structure to support a pregnancy.
Use of fertility medications:
Fertility drugs like clomiphene citrate or letrozole for IUI are often used during ovarian stimulation to improve the number and quality of eggs released.
These IUI medications can significantly boost your chances to improve your success rates, especially when combined with acceptable sperm counts. Medicated cycles typically have higher success rates than natural cycles.
Lifestyle factors:
Smoking, poor diet, high BMI, stress, and alcohol can negatively affect your results.Both partners' lifestyle choices matter.
How to decide if IUI is right for you
Beyond sperm count, IUI might be a suitable choice in these situations:
You or your partner have mild male factor infertility (slightly low count or motility)
You're experiencing unexplained infertility and have been trying for 6–12 months
You have cervical mucus issues preventing sperm from entering the uterus naturally
You have ovulatory issues but respond well to medication
If you have blocked fallopian tubes, are older, have endometriosis, or your partner has serious sperm problems, your doctor might suggest going straight to IVF instead of trying IUI. It doesn’t mean you’ve failed; it simply means there may be a more effective path for your circumstances.
It’s worth sitting down with your fertility specialist to review your full picture. If you want personalised guidance, you can request an appointment with a Thomson Medical fertility specialist to discuss your realistic success rates and whether IUI is the best next step for you.
FAQ
What is the normal sperm count after washing for IUI?
The post-wash sperm count refers to the total number of motile sperm in the sample after it has been processed for IUI, typically measured as the Total Motile Sperm Count (TMSC). A TMSC of 5–10 million motile sperm after washing is considered acceptable for IUI. A TMSC greater than 10 million is ideal and associated with higher success rates. While pregnancy is possible with lower counts, chances decrease significantly below 1 million motile sperm post-wash.
What is the sperm quality required for IUI?
For IUI to work, you need well-shaped, fast-swimming sperm that can reach and fertilise the egg. Key indicators include at least 30–50% motility with progressive forward movement, 4% or more normal forms using Kruger strict criteria, and pre-wash concentrations above 15 million sperm/mL.
Can IUI work with a low post-wash sperm count?
Yes, IUI can sometimes result in pregnancy even with low post-wash sperm counts, but the chances are lower. If there are 1 to 5 million motile sperm, the success rate is reduced, but pregnancy is still possible. If there are less than 1 million motile sperm, IUI success is rare. In these cases, IVF or ICSI is often recommended, as these treatments can work with much lower sperm counts.
Can lifestyle changes improve sperm count before IUI?
Yes, sperm quality responds to lifestyle changes made 2–3 months before IUI, the time needed for sperm to mature. You can eat a balanced diet rich in vegetables, lean protein, omega-3s, and whole grains.
Consider supplements like zinc, folic acid, and CoQ10 after consulting your doctor. Maintain a healthy weight, as obesity lowers testosterone and sperm quality. Avoid hot baths, saunas, and tight underwear as they raise scrotal temperature. Quitting smoking and reducing alcohol can significantly improve sperm count and quality.
Is natural IUI still possible with a lower sperm count?
Natural IUI refers to an IUI cycle without ovulation-inducing medication. It's performed in patients who ovulate regularly on their own. If sperm count is borderline or mildly low, natural IUI may still be attempted, but the success rate will likely be lower than with medicated cycles.
For severely low counts, combining IUI with ovulation-stimulating drugs (like clomiphene or letrozole) may improve chances by increasing the number of eggs available for fertilisation. For severely low counts, natural IUI usually isn't recommended, and IVF may offer better results.
What if the post-wash sperm count is unexpectedly low on the day?
This can feel devastating after all your preparation. Your fertility doctor will review the situation and decide on the safest and most effective next step. They may still recommend proceeding with IUI if the count is borderline.
In some cases, they may freeze the sperm sample and ask for another sperm collection, discuss alternatives such as IVF or ICSI, or talk through the option of donor sperm if the count is extremely low or the sperm are immotile. They may also suggest repeating the semen analysis and postponing the IUI until a better-quality sample can be obtained. Your doctor will explain each option and guide you based on what is best for your circumstances.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical.Request an appointment with Thomson Medical today.
Reference:
Ok, E. K., Dogan, O. E., Okyay, R. E., & Gulekli, B. (2013). The effect of post-wash total progressive motile sperm count and semen volume on pregnancy outcomes in intrauterine insemination cycles: A retrospective study. Journal of the Turkish-German Gynaecological Association, 14(3), 142–145. https://doi.org/10.5152/jtgga.2013.52280
For more information, contact us:
Thomson Fertility
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Request an Appointment