Did you know? Between 2018 and 2022, gynaecological cancers (including uterine, ovarian, and cervical cancers) ranked as the fourth, sixth, and tenth most common cancers among women in Singapore, according to the 2022 Singapore Cancer Registry Annual Report.
Although this cancer is common, many women don't realise they have it. This is because they often develop without any immediate symptoms, or the symptoms they do present are similar to those of other common gynaecological conditions, such as abnormal bleeding.
What is gynaecological cancer management?
Gynaecological cancer management refers to the process of diagnosing, treating and supporting women with cancers affecting the reproductive organs. Because not all gynaecological cancers are the same, management depends on factors such as the stage of the cancer, any other health conditions you have, and your preferences.
Each type of cancer begins in a different part of your reproductive system and displays distinct signs, risk factors, and treatment approaches. That's why early detection and finding the right specialist are crucial. A gynaecological oncologist, a specialist in cancers of the female reproductive system, can recommend the most appropriate treatment based on your cancer type and stage.
5 common gynaecological cancers
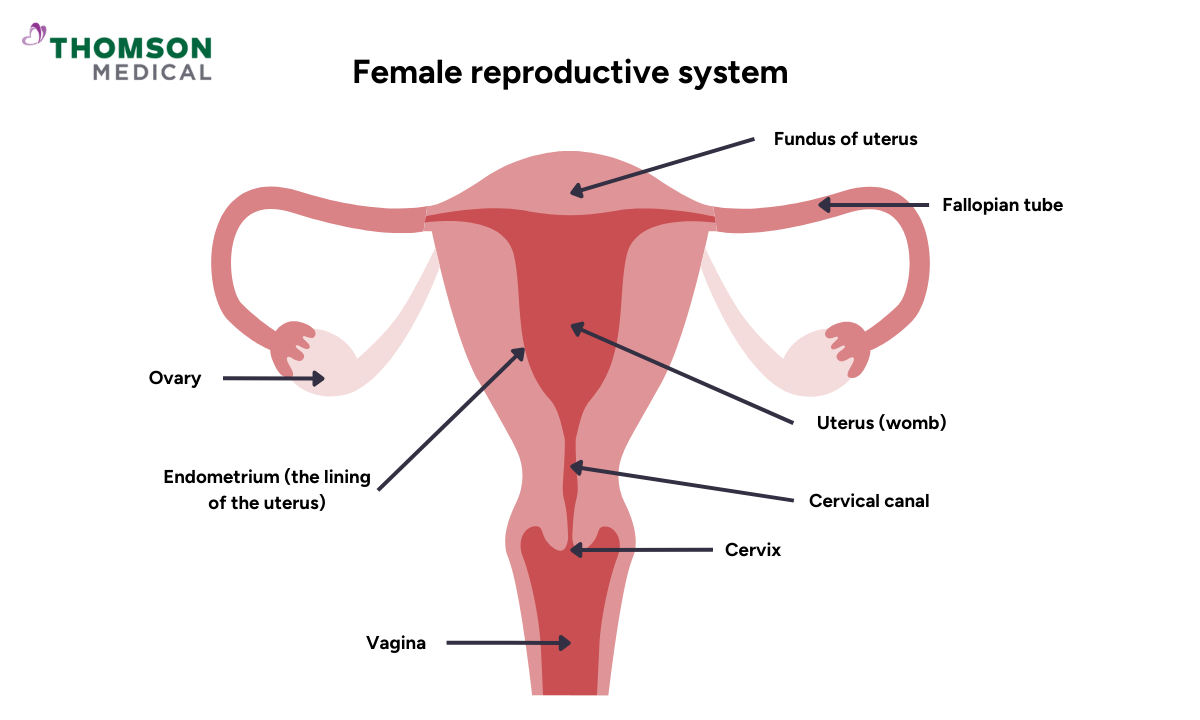
The female reproductive system includes several organs, such as the uterus (womb), the ovaries (where eggs are produced), the cervix (the lower part of the womb), the vagina, and the vulva (the outer genital part).
Cancers that originate in any of these parts of the reproductive organs are known as gynaecological cancers. The five most common types of gynaecological cancer are:
Uterine (endometrial) cancer
Endometrial cancer, or uterine cancer, is a type of cancer that originates in the lining of the uterus, known as the endometrium. This lining is where the early foetus (embryo) implants and continues to grow. It is one of the most common gynaecologic cancers that usually affect postmenopausal women.
Cancerous changes in the lining of the womb typically take place in a woman's late 40s, with endometrial cancer most commonly diagnosed in women in their 50s and 60s. However, unlike ovarian cancer, this condition is usually detected in the first stage of development, also known as FIGO Stage I.
Ovarian cancer
Ovarian cancer occurs when abnormal cells in the ovaries start to grow and divide uncontrollably, forming a tumour. These cancerous cells can eventually spread to nearby tissues or organs. As the ovaries are located deep within the pelvis, symptoms may not appear until the disease has progressed, making early detection difficult.
Ovarian cancer may develop because of a combination of genetic, hormonal, and environmental factors. Some of these factors may increase the likelihood of mutations in ovarian cells or create a hormonal environment that promotes tumour growth. Ovarian cancer is often described as a "silent disease" because its symptoms can be vague or overlooked.
Cervical cancer
Cervical cancer develops in the cells of the cervix, the lower, narrow part of the uterus that connects to the vagina. It is most often caused by persistent infection with the human papillomavirus (HPV).
Treatment options depend on the stage of the cancer and its specific characteristics, but early detection offers the best chance for successful treatment. Regular cervical screening (Pap smear or HPV test) can help detect changes early, before they develop into cancer.
Vaginal cancer
The vagina, also known as the birth canal, is a muscular tube that connects the womb with the outer part of the genitals (vulva). It's a rare form of cancer that most often occurs in the cells lining the vagina; the cells multiply quickly and can harm healthy body tissue.
Vaginal cancer may not cause any symptoms at first. As it grows, vaginal cancer may cause signs and symptoms, such as:
Painful urination
Frequent urination
Constipation
Pelvic pain
Abnormal vaginal discharge or bleeding
A lump or mass in the vagina
Vulvar cancer
Vulvar cancer starts as a growth of cells on the vulva, which is the outer part of your genitals. This includes the clitoris, labia (the vaginal lips), and the perineum (the skin between the vagina and the anus).
Vulvar cancer is rare and usually forms as a lump or sore on the vulva, often causing itching. Although it can occur at any age, vulvar cancer is typically diagnosed in older adults. Treatment often begins with surgery to remove the cancer and a small amount of surrounding healthy tissue.
Upon receiving a gynaecological cancer diagnosis, it’s normal to feel anxious about what will happen next. At Thomson Women's Clinic & Cancer Surgery, our gynaecological oncologists understand your concerns, take the time to answer your questions and explain your options clearly, and support you throughout your treatment. Schedule your appointment today.
Our gynaecological oncologist
Loading...
Gynaecological cancer management
Now that you understand the different types of gynaecological cancers, let's discuss how they're managed. Treatment approaches vary depending on your specific cancer type, stage, overall health, and personal circumstances, including whether you hope to preserve fertility.
Surgery
Surgery is the primary treatment for most gynaecological cancers, particularly when caught early. The type of surgery depends on your specific diagnosis and how far the cancer has spread.
Common surgical procedures include:
For cervical cancer:
For early-stage cervical cancer, surgery often involves removing the cervix (trachelectomy) or the uterus (hysterectomy).
Fertility-preservation options, such as cone biopsy or Loop Electrosurgical Excision Procedure (LEEP), may also be available for very early-stage cancer.
For ovarian cancer:
Unilateral salpingo-oophorectomy removes the affected ovary and its fallopian tube while preserving the other ovary and your uterus, allowing you to have children in the future.
Bilateral salpingo-oophorectomy with hysterectomy removes both ovaries, both fallopian tubes, and the uterus. After this procedure, natural pregnancy is no longer possible. But if you froze eggs or embryos before the surgery, surrogacy might be an option.
Cytoreductive (debulking) surgery removes as much visible cancer as possible from the abdomen and pelvis. This procedure is used for advanced-stage ovarian cancer and aims to remove all visible tumours.
Your surgeon may use laparoscopy (a minimally invasive surgery) or laparotomy (open surgery that requires an abdominal incision) during the procedure. The choice depends on the extent of your cancer and your individual circumstances.
For uterine cancer:
Treatment for uterine cancer usually includes the removal of the fallopian tubes and ovaries, called a salpingo-oophorectomy.
During surgery, your surgeon may also remove lymph nodes through a sentinel lymph node biopsy, which helps determine your cancer's stage and whether the cancer has spread to nearby lymph nodes.
For vulvar and vaginal cancers:
For vulvar and vaginal cancers, your surgeon may perform laser surgery, using a laser beam to remove precancerous cells or very early-stage abnormalities.
Local excision, or wide local excision, removes the cancer and a small amount of normal tissue around it. Nearby lymph nodes may also be removed for testing to identify if cancer has spread.
Vulvectomy removes part (partial vulvectomy) or all (complete vulvectomy) of the vulva and possibly some nearby lymph nodes.
Pelvic exenteration is a procedure used only for advanced or recurrent cancer that hasn't responded to other treatments. It may remove your lower colon, rectum, bladder, cervix, vagina, ovaries, and nearby lymph nodes.
Chemotherapy
Chemotherapy uses strong drugs to fight cancer cells throughout your body. It's often recommended after surgery to eliminate any remaining cancer cells or before surgery to shrink tumours and make them easier to remove.
Many chemotherapy medicines exist. Most chemotherapy medicines are given through a vein (intravenously), while some come in pill or liquid form that you can take at home. The type and amount of chemotherapy are adjusted depending on the cancer characteristics, stage, and how your body responds to treatment.
Radiation therapy
Radiation therapy uses high-energy beams to kill cancer cells in specific areas of your body. It may be used alone or in combination with surgery and chemotherapy. There are a few types of radiation therapy used for gynaecological cancers:
External radiation therapy involves directing beams of high-energy radiation from a machine outside your body towards the tumour. This is similar to having an X-ray but uses a stronger radiation dose.
Internal radiation therapy (brachytherapy), where the radioactive material is placed inside the body near the cancer cells, delivers high doses while minimising damage to the surrounding healthy tissue.
Chemoradiotherapy, a combination of chemotherapy and radiation therapy, enhances the effectiveness of treatment. This combination approach makes cancer cells more sensitive to radiation and is commonly used for locally advanced gynaecological cancers.
Targeted therapy
Targeted therapy is a treatment that uses medicines to attack specific chemicals in cancer cells. It works by targeting proteins that control how cancer cells grow and spread. By blocking these proteins, targeted treatments can cause cancer cells to die.
Immunotherapy
Immunotherapy uses medicine to stimulate the immune system's ability to recognise and destroy cancerous cells. Cancer cells pretend to be healthy so they can hide from your immune system. Immunotherapy helps target these signals so the cancer cells can’t trick your body into thinking it’s a healthy cell.
Your treatment plan will be customised based on your specific cancer type and stage. Your specialist will help you decide which treatment is most appropriate for your condition.
At Thomson Women's Clinic & Cancer Surgery, our specialists understand your concerns and will help to explain all the available options. They will work with you to create a treatment plan tailored to your specific situation. Schedule an appointment for a consultation with a gynaecological oncologist.
How you can prevent gynaecological cancer

Although not all gynaecological cancers can be completely prevented, there are important steps you can take to significantly reduce your risk.
Regular gynaecological cancer screening, including Pap smears and HPV tests, is recommended for all women who have been sexually active. These screenings can detect precancerous changes before they develop into cancer. The HPV vaccine also provides strong protection against the virus that causes cervical, vaginal, and vulvar cancers.
Early detection through regular screening is important, because early-stage cancers are generally more treatable and have a better outcome.
Thomson Medical's 4-in-1 women screening
To help prevent gynaecological cancers, early detection is important, as symptoms may not appear until advanced stages. A regular screening can help identify abnormal changes and potential warning signs before they progress.
To help prevent these conditions, we offer a 4-in-1 women's screening package to detect potential issues early, when they're most treatable. These include:
Consultation & examination with a gynaecological oncologist
Pap smear
HPV test
We also offer the HPV vaccine to help protect against cervical, vaginal, and vulvar cancers. The vaccine works best when given before age 14, but adults up to age 26 (and sometimes 45) can still benefit.
You're not alone
Receiving a cancer diagnosis can feel overwhelming, but remember – you are not alone in this journey. At Thomson Women's Clinic and Cancer Surgery, our specialists provide thorough support, from diagnosis to treatment and follow-up care. We are here to support you with:
Dedicated specialists to guide you through your treatment options.
Regular check-ups and monitoring to ensure you receive the best possible care.
Counselling services to help you and your loved ones cope with the emotional aspects.
Treatment cost
Treatment costs vary depending on your specific cancer type and treatment plan. For instance, the cost of laparoscopic surgeries, commonly conducted as day surgeries, typically falls between SGD 7,200 and 11,570. Additional charges may arise for pre-surgery consultations, imaging tests (such as X-rays or CT scans), medications, and post-surgery follow-up appointments.
Fortunately, there are several programmes in Singapore that can help lower the total cost, such as MediSave, MediShield Life, and Integrated Shield Plans. Each of these offers different levels of coverage depending on your eligibility and insurance arrangements.
This price was last updated in June 2025. Treatment costs may have changed since then. For current pricing, detailed insurance coverage information, and personalised financial guidance, contact our medical concierge team.
FAQ
Should I see an O&G or a gynaecological oncologist?
If you've been diagnosed with or suspect you may have a gynaecological cancer, it's recommended to consult a gynaecological oncologist. A gynaecological oncologist is a specialist who has completed both obstetrics & gynaecology (O&G) training and additional subspeciality training specifically in the diagnosis and surgical management of gynaecological cancers.
What are the common types of gynaecological cancers?
The five main types of gynaecological cancer are cervical, ovarian, uterine (endometrial), vaginal and vulvar. Each begins in a different part of the female reproductive system and has different risk factors, symptoms, and treatment approaches.
Cervical, ovarian and uterine cancers are the most common, ranking as the fourth, sixth, and tenth most common cancers among women in Singapore between 2018 and 2022.
How can I reduce my risk of gynaecological cancers?
While you can't prevent all gynaecological cancers, you can significantly reduce your risk by:
- Regularly undergo screenings, such as Pap smears and HPV tests, to detect cervical cancer.
- Getting an HPV vaccination, which protects against the virus that causes cervical, vaginal and vulvar cancers.
- Maintain a healthy lifestyle, including a healthy weight, eating a balanced diet, not smoking, and limiting your alcohol consumption.
- If you have a family history of gynaecological or breast cancers, genetic counselling can help you assess your risk.
The Ministry of Health recommends that all women aged 25 and over who are or have been sexually active undergo regular cervical cancer screening.
What are the main treatment options for gynaecological cancers?
The treatment you receive will depend on the type, stage and location of your cancer, as well as your overall health and circumstances. The main treatment options include:
- Surgery, which is often the primary treatment and can range from minimally invasive laparoscopic procedures to more extensive operations.
- Chemotherapy uses powerful drugs to kill cancer cells throughout the body and is usually given before or after surgery.
- Radiotherapy uses high-energy beams to kill cancer cells in specific areas.
- Targeted therapy involves medicines that attack specific proteins in cancer cells.
- Immunotherapy helps your immune system recognise cancerous cells and destroy them.
Your gynaecologic oncologist will create a personalised treatment plan based on your diagnosis and needs.
What is the role of chemotherapy in gynaecological cancer treatment?
Chemotherapy uses strong drugs to kill or slow the growth of cancer cells. It plays different roles depending on your cancer type and stage. Most chemotherapy for gynaecological cancers is given intravenously (through a vein), though some comes in pill form. Your oncologist will determine the specific drugs, dosage, and schedule based on your cancer type and response to treatment.
When is radiation therapy recommended for gynaecological cancers?
Radiation therapy uses high-energy beams to kill cancer cells, and it may be recommended at various stages of treatment.
- It can be used as the primary treatment for early-stage cancers when surgery isn't feasible due to tumour size or location.
- It may also be used before surgery (neoadjuvant therapy) to shrink large tumours, making them easier to remove.
- It may also be used after surgery (adjuvant therapy) to eliminate any remaining cancer cells in the treatment area.
- It can also be used for advanced cancer to shrink tumours that have spread to other areas or relieve symptoms.
There are two main types of radiation therapy, external beam radiation therapy, where radiation is delivered from outside the body, and brachytherapy, where radioactive material is placed inside the body near the cancer cells.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations for your specific conditions, schedule a consultation with our gynaecological oncologists at Thomson Women's Clinic & Cancer Surgery.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Dr Ryan Lee Wai Kheong
Obstetrics & Gynaecology (O&G)
Thomson Specialists Woodleigh (Women's Health)
English, Mandarin
Prudential, Great Eastern, Adept, MHC and 4 others

