Ovarian cancer can be challenging to detect early because its symptoms are often subtle and easy to mistake for something less serious. This can understandably raise concerns, especially for women who are worried about their long-term health or have a family history of the condition.
Although there is no guaranteed way to prevent ovarian cancer, there are steps you can take to help lower risk and support early detection. Understanding the factors that influence risk and the steps that support early detection can help you take a proactive and reassuring approach to your health.
What causes ovarian cancer?
Ovarian cancer starts when cells in or near your ovaries begin growing abnormally. Sometimes it begins in your fallopian tubes (the tubes connecting your ovaries to your uterus) and then spreads to the ovaries.
The truth is, there's not always a clear answer for why it develops. It's linked to many factors, including genetic changes, hormonal factors, and cell damage that your body can't repair properly. Some of these genetic changes run in families, while others simply develop as you get older.
Who is most at risk of developing ovarian cancer?
Ovarian cancer is sometimes called a "silent disease" because its symptoms can be easy to miss or mistake for something less serious.
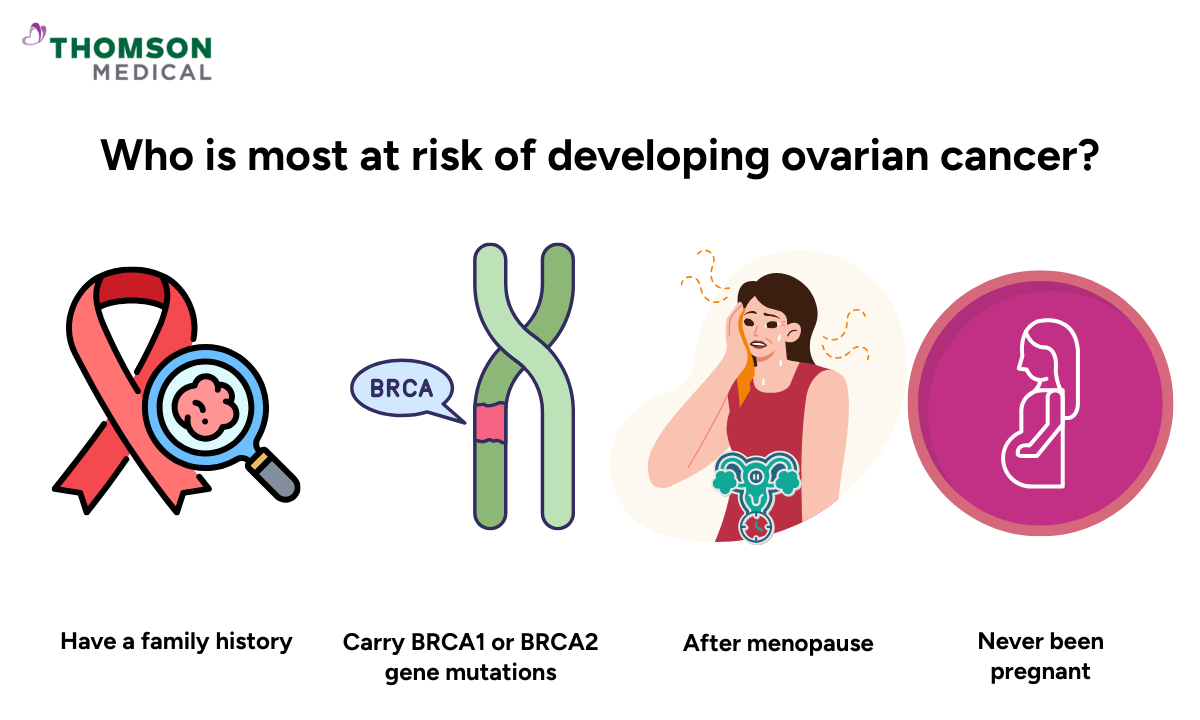
While anyone with ovaries can develop ovarian cancer, some risk factors might increase your chances:
Have a family history of ovarian or breast cancers
Carry BRCA1 or BRCA2 gene mutations (sometimes called a BRCA gene fault)
Are older, especially after menopause
Have never been pregnant
Have certain hormonal or reproductive histories
If you recognise multiple risk factors in yourself, it's completely natural to feel concerned. Your doctor is there to support you. They can assess your individual risk in a caring, personalised way and talk through whether additional testing might be right for you.
If you’re concerned about your risk of related cancers, request an appointment with Thomson Medical for a personalised risk assessment. Our specialists can advise whether genetic testing, closer monitoring, or further screening is appropriate for you.
Ovarian cancer specialist
Loading...
What should you do if it runs in your family?
If you have relatives who've had ovarian cancer, it's natural to feel concerned about your own risk. While you can't change your family history, you can take steps to understand and manage your risk.
Here's what you can do:
Talk to your doctor about your family history
Consider genetic testing and counseling to understand your personal risk
Learn the warning signs to watch for
Discuss screening and prevention options that work for you
Finding out you carry a genetic mutation can feel overwhelming, but it also means you have choices. Your doctor can talk you through preventive options, which might include surgery for some women, based on your age, health, and personal circumstances.
Can ovarian cancer prevention lower your risk?
You can't completely prevent ovarian cancer, but there are a few steps you can take that might improve your chances.
Genetic awareness and testing
If ovarian cancer or breast cancer runs in your family, genetic testing can help you understand your risk. Testing looks for inherited gene changes like BRCA 1 or BRCA 2 that increase your chances of developing these cancers.
If you test positive for a genetic mutation, you and your doctor can create a plan that might include:
More frequent screening to catch any changes early
Preventive surgery if appropriate for your situation
Other risk-reducing strategies tailored to your needs
Your doctor can guide you through what these results mean for you personally.
Hormonal and reproductive factors
Birth control pills, pregnancy and breastfeeding affect your hormones in ways that might offer some protection. Your risk may be lower if you:
Use birth control pills (also called oral contraceptives) for several years
Have been pregnant and breastfed
Had a tubal ligation
However, decisions about birth control or family planning should always be based on what's right for your life, not just cancer prevention.
Healthy lifestyle choices
Staying healthy won't prevent ovarian cancer on its own, but certain habits may reduce your risk alongside supporting your overall wellbeing.
Here are some steps that may help:
Maintain a healthy weight
Eat a balanced diet with plenty of fruits, vegetables, and whole grains
Stay physically active
Avoid unhealthy habits such as smoking
These habits work by supporting your body's overall health and may help protect against various cancers. Even small changes can add up over time, so be kind to yourself as you make adjustments.
When should you see a doctor?
You don't need to wait for symptoms to talk about your risk. You should consider getting checked if you:
Have a family history of ovarian or related cancers and haven't discussed it with your doctor
Want to explore genetic testing
Experience persistent bloating, pelvic pain, feeling full quickly, or changes in appetite that last more than two weeks
During your visit, your doctor can perform a pelvic exam, review your symptoms, and recommend tests like CA-125 or imaging if needed.
Getting checked doesn't mean something is wrong. It gives you clarity and ensures you have the support and information you need to make the best choices for your health.
If you have concerns or a family history of ovarian cancer, request an appointment with Thomson Medical to review your risk. Our doctors can create a monitoring plan based on your individual situation.
FAQ
Can lifestyle and food really prevent ovarian cancer?
Lifestyle and dietary changes can help lower your risk, but they cannot fully prevent ovarian cancer. Eating more fruits and vegetables, whole grains, and lean proteins supports your immune system and helps your body stay strong.
Does taking birth control reduce the risk of ovarian cancer?
Yes. If you've used birth control pills long-term, you may have lowered your ovarian cancer risk. This protective effect can last for years even after you stop taking them. Other procedures you may have had, like tubal ligation, may also offer some protection.
Does hormone replacement therapy affect my risk?
If you're using or considering hormone replacement therapy for menopause, it's important to discuss this with your doctor. Long-term use of hormone replacement therapy may slightly increase your ovarian cancer risk. Your doctor can help you weigh the benefits for managing menopause symptoms against potential risks.
Should I get genetic testing if it runs in my family?
If multiple close relatives in your family have had ovarian cancer or related cancers, genetic counselling is often recommended. A counsellor can help you understand whether testing is right for you and what your results might mean for your health and prevention options.
Why is there no routine screening test for ovarian cancer?
Current tests aren't accurate enough to screen all women routinely. They might miss cancer or give false alarms, leading to unnecessary worry or procedures. Tests like CA-125 or ultrasound are typically used only when you have symptoms or known risk factors.
How can I detect it early?
Early detection is challenging, but paying attention to your body is your best tool. Watch for symptoms like persistent bloating, pain in your pelvic area, and feeling full quickly. If you notice these symptoms are new for you and they don't go away, contact your doctor.
What happens if ovarian cancer spreads?
If your ovarian cancer spreads, it may reach nearby organs in your reproductive system or pelvic region and sometimes your lymph nodes (glands that filter body fluids).
If you're facing advanced cancer, your treatment options may include targeted therapy (medicines that attack specific cancer cells). Your doctor will work with you to determine the best approach for your situation.
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
Reference:
Momenimovahed, Z., Tiznobaik, A., Taheri, S., & Salehiniya, H. (2019). Ovarian cancer in the world: epidemiology and risk factors International Journal of Women S Health, Volume 11, 287–299. https://doi.org/10.2147/ijwh.s197604
Xiang, H., Wang, L., Sun, L., & Xu, S. (2024). The risk of ovarian cancer in hormone replacement therapy users: a systematic review and meta-analysis. Frontiers in Endocrinology, 15, 1414968. https://doi.org/10.3389/fendo.2024.1414968
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment